Superficial Pustular Folliculitis of the Face and Neck—A Non-Infectious Eruption Responding to Topical Steroids
ABSTRACT
Background
We have seen patients presenting with tiny, superficial follicular pustules on the face and neck that appeared distinct from common or well-known facial pustular dermatoses, such as acne vulgaris, rosacea, demodicosis, and Ofuji's disease.
Objectives
We aimed to describe the clinicopathologic features, differential diagnosis, and treatment of this pustular eruption in southern Taiwan.
Methods
We retrospectively reviewed the medical records and clinical photos of cases presenting with tiny, superficial follicular pustules on the face and/or neck during July 2017–March 2022. Cases of rosacea, acne vulgaris, demodicosis, and Ofuji's disease were excluded.
Results
A total of 27 patients (26 females and 1 male; mean age of 25.2 ± 4.3 years) were included for analysis. All patients presented with monomorphous, discrete, tiny, superficial pustules on the face and/or neck. The pustules varied from a few to hundreds in number. The eruptions were distributed on the face in 12 (44.4%) patients, the face and neck in 14 (51.8%), and the neck in one (3.7%), and was itchy in 44.4%. The pustules lasted 1 day to 1 month, mostly within 1 week, before treatment, and was recurrent in 81% of cases with 2–20 episodes individually. Twenty-four of the 25 (96%) patients responded well to steroids with complete clearance of pustules. Skin biopsy of pustules performed in three cases showed infundibular pustules filled with neutrophils and a perivascular lymphohistiocytic infiltrate in the dermis. Gram staining revealed negative finding. Bacterial cultures performed in two patients revealed Cutibacterium acnes.
Conclusions
Based on our observation, we would like to propose the term ‘superficial pustular folliculitis of the face and neck’ (SPFFN) for this type of eruption. It is important to be familiar with this particular type of follicular pustulosis, especially when dealing with young females as the pustules respond well to low-potency topical steroids.
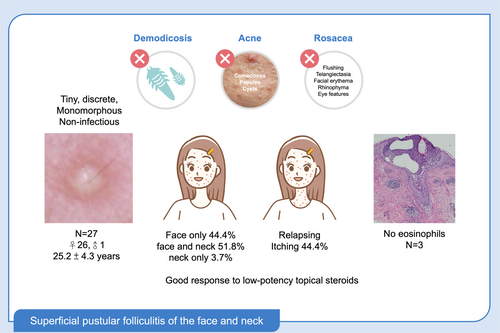
Graphical Abstract
Twenty-seven young patients, mostly females, presenting with monomorphous, discrete, tiny, superficial follicular pustules on the face (44.4%), the face and neck (51.8%) and the neck (3.7%). The eruption was itchy in 44.4%, recurrent in 81% of cases and responded well to topical corticosteroids. Histopathologic findings of 3 cases revealed infundibular pustules filled with neutrophils and a perivascular lymphohistiocytic infiltrate in the dermis. The clinical and pathological chracters indicated a non-infectious follicular pustulosis different from demodicosis, acne, rosacea and Ofuli's disease.
1 Introduction
Pustular eruptions are common features in dermatological practice. There are many conditions that cause pustules on the face and neck. Among the follicular corresponding pustules, rosacea and Ofuji's disease are predominant in females. The typical inflammatory lesions in rosacea are small pustules to large papulopustules in addition to centrofacial erythema [1-3]. Ofuji's disease is a rare pustular dermatosis of unknown etiology, and manifests as small papules and/or pustules typically in an annular configuration involving the face and trunk in some cases [4, 5]. Acne vulgaris is characterised by comedones, follicular papules, pustules and nodules of the face, neck and upper torso [6, 7]. Demodex mites, when present in excessive count, may also cause folliculitis on the face, neck and scalp [8, 9]. Follicular impetigo, also known as Bockhart impetigo, is caused by Staphylococcus aureus. It manifests as superficial, small, fragile, domed pustules. The pustules appear in crops and may fuse together [10]. Pityrosporum folliculitis is an acneiform-papules or pustules caused by overgrowth and infection of Malassezia furfur. The rash is usually monomorphic [11, 12]. Papulopustular rash affects the face and upper body is a common dermatologic side effect of epidermal growth factor receptor (EGFR) inhibitors [13]. Besides, 3 rare photodermatoses including actinic superficial folliculitis [14], actinic folliculitis [15], and acute and recurrent facial pustulosis [16] also present follicular-based pustules.
In terms of non-follicular pustular dermatoses, tinea faciei may be present with pustules in addition to an annular or arcuate active margin. The diagnosis is made by scraping and KOH examination for fungal elements [17]. Acute localised exanthematous pustulosis is a drug reaction characterised by the sudden onset of localised, clustered pinhead-sized, and sterile pustules over an erythematous and oedematous background [18]. Miliaria pustulosa is a variant of miliaria rubra that caused by obstruction of the sweat ducts. The upper trunk, neck, and head are the most commonly affected sites [19]. Pustular allergic contact dermatitis develops after the application of topical agents or fragrance [20, 21].
We observed patients presenting with recurrent, monomorphous, discrete, tiny, superficial follicular pustules on the face and neck. This form of pustular eruption appears distinct from the aforementioned facial dermatoses with follicular pustules and requires differential diagnosis from other facial dermatoses with follicular pustules and different treatment approach.
2 Methods
We reviewed the medical records and photographs of patients with facial and neck pustulosis between July 2017 and March 2022. At the time of diagnosis, all patients presented with monomorphous, tiny, superficial follicular pustules on the face and/or neck but no comedones, papules, cysts, background facial erythema, telangiectasia, facial flushing, eye manifestations, phymatous changes or annular configurations. Demodex densities were evaluated in all cases by the thumbnail-squeezing method (TSM) [22] or superficial needle-scraping (SNS) method [23]. High Demodex density was defined as > 11 mites/cm2 using the TSM [22] or > 2 mites/5 pustules by the SNS method [23]. Patients with high Demodex densities indicating demodicosis were excluded. Clinical outcomes were assessed either by the physician during clinic visits or by the patient, who reported them during subsequent visits or follow-up phone calls.
3 Results
A total of 27 (26 females and 1 male) patients were included for analysis (Table 1). Age ranged from 18 to 34 years with a mean of 25.2 ± 4.3 years. The age of onset was 16–34 (mean 24.2 ± 4.6 years). The pustules were scattered on the face, including the cheeks, forehead, temples, nose, eyelids, nasolabial folds, around the philtrum, chin, and neck. The number of pustules varied from fewer than 10 to several hundred and was limited to the face in 12 (44.4%) patients, the face and neck in 14 (51.8%), and the neck in one (3.7%). Pustules were itchy in 12 of 27 (44.4%). Demodex densities ranged from 0 to 2 mites/5 pustules by the SNS method and 0 to 10 mites/cm2 by the TSM. Skin biopsy of pustules performed in three cases showed infundibular pustules filled with neutrophils, and a perivascular lymphohistiocytic infiltrate in the dermis (Figures 1e, 2c,d, 3c). Gram staining revealed no Gram-positive bacteria. Bacterial cultures performed in two patients revealed Cutibacterium acnes.
| Case no. | Sex | Age | Age of onset | Site of involvement | No. of pustules | Demodex density* | Treatment | Time to complete clearance |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 24 | 24 | Face (forehead, temples, cheeks, chin, nose, glabella), neck | Dozens to numerous | SNS (0), TSM (0) | Systemic steroids, mometasone furoate 0.1% cream, levocetirizine, or BC | 3 days |
| 2 | F | 25 | 24 | Face (forehead, temples, cheeks, chin, around philtrum, glabella), neck | Dozens to numerous | SNS (0), TSM (0) | Systemic steroids, mometasone furoate 0.1% cream, levocetirizine, or BC | 3 days |
| 3 | F | 29 | 24 | Face (forehead, temples, cheeks, chin, around philtrum, nasolabial folds, glabella), neck | Numerous | SNS (0), TSM (0) | BC/desloratadine | 4–7 days |
| 4 | F | 26 | 24 | Face (temples, eyelids, cheeks, chin, nose, nasolabial folds), neck | Dozens to hundreds | SNS (0) | BC | 2–3 days |
| 5 | F | 20 | 19 | Face (cheeks, chin), neck (anterior, occipital hairline, nape), upper back | Hundreds | TSM (0) | BC | 6 days |
| 6 | F | 25 | 22 | Face (forehead, temples, cheeks, chin, nasolabial folds, glabella), | Dozens | SNS (0) | BC | 7 days |
| 7 | F | 29 | 27 | Face (forehead, temples, cheeks, chin), neck, nape | Hundreds | SNS (0), TSM (2) | BC | 1 week |
| 8 | F | 21 | 21 | Face (forehead, glabella, temples, cheeks, nose), neck | Dozens | SNS (0) | BC | < 1 week |
| 9 | M | 28 | 28 | Face (forehead, temples, cheeks, nasolabial folds, glabella), neck | Hundreds | SNS (1) | Systemic steroids + CC | 2 days |
| 10 | F | 27 | 26 | Face (forehead, temples, cheeks, chin, nasolabial folds, nose, glabella, eyelids), neck | Dozens | SNS (0) | BC | 1week |
| 11 | F | 18 | 18 | Face (glabella, eyelids, cheeks, nose, nasolabial folds, chin, lip margins) | Dozens | SNS (2), TSM (2) | CC Metronidazole 0.75% gel | < 1week |
| 12 | F | 21 | 16 | Face (glabella, eyelids, cheeks, nasolabial folds, chin), neck | Hundreds | SNS (0) | BC | 3–7 days |
| 13 | F | 21 | 21 | Face (forehead, glabella, eyelids, cheeks, chin, nose, nasolabial folds) | Hundreds | SNS (1), TSM (6) | Doxycycline, levocetirizine, pimecrolimus 1% cream | Lost to follow-up |
| 14 | F | 20 | 20 | Face (forehead, glabella, eyelids, temples, cheeks, chin, nose, nasolabial folds), neck | Dozens | TSM (10) | Cephalexin/gentamycin 0.1% cream | 5 days |
| 15 | F | 24 | 24 | Face (forehead, glabella, eyelids, temples, cheeks, chin, nose, nasolabial folds), neck | Dozens | SNS (0), TSM (0) | BC | 1–2 weeks |
| 16 | F | 20 | 17 | Neck | Hundreds | SNS (0) | BC | 1 weeks |
| 17 | F | 24 | 24 | Face (forehead, glabella, cheeks, chin) | Dozens | SNS (1), TSM (1) | BC | 4–7 days |
| 18 | F | 22 | 22 | Face (Glabella, cheeks, eyelids, nose, chin) | Dozens | SNS (0) | CC | 4–7 days |
| 19 | F | 23 | 23 | Face (forehead, glabella, cheeks, nose, nasolabial folds, chin), neck | Hundreds | SNS (0), TSM (2) | BC | 4–7 days |
| 20 | F | 29 | 29 | Face (forehead, glabella, cheeks, lip margin, chin), neck | Dozens | TSM (1) | BC | 1 week |
| 21 | F | 23 | 22 | Face (forehead, glabella, cheeks, lip margin, nasolabial folds) | Dozens | SNS (0), TSM (3) | BC/levocetirizine | 2–3 days |
| 22 | F | 33 | 32 | Face (forehead, glabella, eyelids, cheeks, nose, lip margin, nasolabial folds) | Dozens to one hundred | SNS (0) | CC | 4–7 days |
| 23 | F | 26 | 26 | Face (forehead, glabella, eyelids, cheeks) | Dozens | TSM (1) | BC/cephalexin | No response |
| 24 | F | 34 | 34 | Face (cheeks, philtrum) | About 10 | TSM (0) | CC | 3 days |
| 25 | F | 27 | 25 | Face (eyelids, cheeks, philtrum, chin) | Fewer than10 | SNS (0), TSM (2) | BC | 2–3 days |
| 26 | F | 30 | 30 | Face (forehead, temples. eyelids, glabella, cheeks, nose, chin) | Dozens | TSM (4) | BC | A couple days |
| 27 | F | 32 | 32 | Face (cheeks, nasolabial folds) | Fewer than 10 | SNS (0), TSM (2) | CC | 4–7 days |
- Note: * A high demodex density is > 2 mites/5 pustules by SNS or > 11 mites/cm2 by TSM.
- Abbreviations: BC, Betamethasone valerate 0.1% cream; CC, Clobetasol butyrate 0.05% cream, SNS, superficial needle-scraping method; TSM, thumbnail-squeezing method.
According to the patients, the pustules lasted 1 day to 1 month, mostly within 1 week, before treatment. Most patients required treatment to recover, although the disease was self-limiting in 3 patients. Overall, the pustules showed complete responses to steroids in 24 of the 25 (96%) patients within 2 days to 1 week, but to antibiotics (cephalexin 250 mg four times a day and topical gentamycin 0.1% cream) in 1 of 4 (25%) patients. Minocycline was ineffective in 2 cases and cephalexin in one. Most patients had total resolution of pustules after treatment with topical betamethasone valerate 0.1% cream alone.
The summary of the clinical features of 27 patients is shown in Table 2. No clear contributory triggering factors were identified. In every patient, the pustules resolved without scarring or pigmentation. The follow-up period ranged from 3 months to 7 years (mean of 29.1 months). The rate of recurrence was 81%. Five patients had a single episode only. The remaining 22 patients experienced 2–20 episodes of recurrence. The interval of recurrence ranged from 1 week to 5 years. One patient developed persistent facial erythema at a 1-year follow-up.
| Characteristics | Descriptions |
|---|---|
| Age (years) | 18–34, mean ± SD: 25.2 ± 4.3, median 25 |
| Age of onset (years) | 16–34, mean ± SD: 24.2 ± 4.6, median 24 |
| Sex | Female: 26, Male: 1 |
| Location | Face: 12 (44.4%), face and neck simultaneously or subsequently: 14 (51.8%), and neck: 1 (3.7%) |
| Triggers | Noncontributory |
| Itching | 12 of 27, uncertain in 7 |
| Follow-up period | 3 to 84 months (mean ± SD: 29.1 ± 20.6) |
| Self-limiting | 3 |
| Rate of recurrence | 81% (2–20 episodes) |
| Interval of recurrence | 1 week to 5 years |
| Scar or pigmentation | None |
| Response to topical steroids | 24 of 25 (96%) |
| Response to antibiotics (cephalexin) | 1 of 4 |
Five representative cases are described briefly as follows.
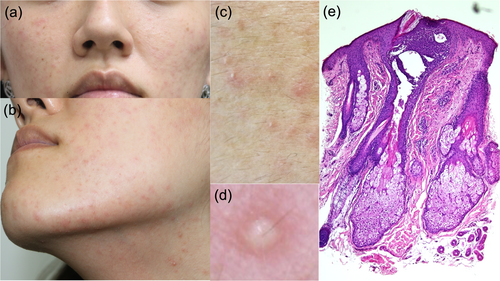
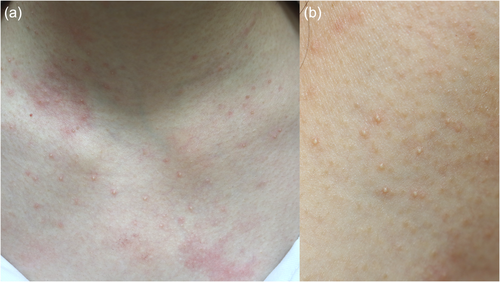
Case 1: A 24-year-old female patient presented with numerous itchy, monomorphous, discrete, tiny, superficial follicular pustules on the face and neck (Figure 1a–d). The rash waxed and waned for 2 months. Demodex examination revealed 0 mites per cm2 or 5 pustules by the TSM and SNS methods. Minocycline and fusidic acid creams were administered under the initial suspicion of bacterial folliculitis. However, the pustules worsened on the following day. The treatment was changed to oral prednisolone 5 mg three times a day, levocetirizine 5 mg daily, and topical mometasone furoate 0.1% cream, with rapid and total recovery of the rash on the 5th day. The eruptions recurred 3 weeks later, and at irregular intervals afterwards, but the recurring rashes responded well to topical corticosteroids treatment.
A skin biopsy was performed on the chin in the 14th week. Histopathology revealed a superficial pustule filled with neutrophils. Dense, superficial, and deep perivascular infiltrations of lymphocytes and histiocytes were observed. Neutrophils and sebum were present in the pustules (Figure 1e). Gram staining revealed no C. acnes or other Gram-positive bacteria.
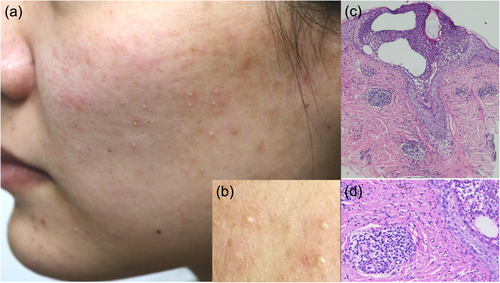
Case 2: A 25-year-old female patient had many monomorphous, discrete, tiny, superficial follicular pustules on the face and neck (Figure 2a,b). The rash recurred every 4–6 weeks in a year, mostly affecting the face but less frequently the neck. No Demodex mites were detected by the TSM and SNS methods. Before the skin biopsy, the patient was treated with oral minocycline 100 mg daily and topical gentamycin 0.1% cream for 5 days without improvement but responded to the same combination of oral prednisolone, levocetirizine, and topical mometasone furoate cream as in Case 1 for 3 days.
The histopathological examination revealed a superficial follicular pustule filled with neutrophils. Mixed inflammatory cell infiltration with lymphocytes, histiocytes, and neutrophils was observed in the superficial perivascular and perifollicular areas (Figure 2c,d). Gram staining revealed no C. acnes or other gram-positive bacteria. The pustules also responded to topical betamethasone valerate 0.1% cream in subsequent flares.
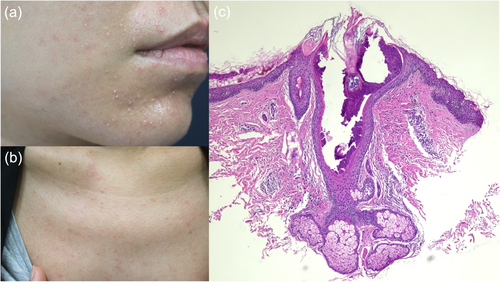
Case 3: A 29-year-old female patient also presented with numerous itchy, monomorphous, discrete, tiny, superficial follicular pustules on the face and neck (Figure 3a,b) for 2 days. A similar episode of rash occurred 5 years ago and lasted for 1 month. The TMS and SNS methods discovered no Demodex. The histopathological examination revealed a superficial follicular pustule filled with neutrophils. Superficial, deep perivascular, and interstitial lymphohistiocytic infiltrations were observed (Figure 3c). Gram staining revealed no C. acnes or other Gram-positive bacteria. With the experience in Case 1 and 2, the pustules were treated with desloratadine 5 mg daily and topical betamethasone valerate 0.1% cream; the rash completely cleared in 3 days.
Case 4: A 26-year-old female patient presented with many discrete, tiny, superficial follicular pustules on the neck for 1 day (Figure 4). No Demodex mites were found from 5 pustules by the SNS method. The rash subsided 2 days after topical betamethasone valerate 0.1% cream. A few tiny pustules occurred on the face 1 week later. The pustules involved the neck only in three subsequent episodes in 5 years. All the subsequent rash responded completely, as in the 1st episode.
Case 5: A 20-year-old female patient presented with many discrete, tiny, superficial follicular pustules on the face and neck, including v-area and nape, and upper back for 3 days (Figure 5). She complained of five episodes of recurrence in the past year and resolution of the prior rash within 1 week after treatment. No Demodex mites were found using the TSM. The rash subsided 6 days after topical betamethasone valerate 0.1% cream and did not recur for the following 5 years.

4 Discussion
Based on the clinical and pathological findings in the present study, the facial follicular pustules appear to differ from other known facial dermatoses with follicular pustules, such as acne vulgaris, rosacea, Demodex folliculitis, Ofuji's disease, Bockhart's impetigo, actinic superficial folliculitis, actinic folliculitis, and acute and recurrent facial pustulosis. Table 3 summarises the characteristic features of these facial follicular pustular dermatoses.
| Diagnosis | Trigger factors | Distribution of lesions | Morphology of lesions |
|---|---|---|---|
| Superficial pustular folliculitis of the face and neck | None | Face and/or neck | Discrete, monomorphous, superficial pustules |
| Acne vulgaris | Positive familial history, dietary habits (milk), oily skin, insufficient sleep, cosmetic make-up use, stress | Face, neck, and even the trunk | Comedones, papules, pustules |
| Rosacea | UV-light, Demodex, stress, heat, exercise, spicy food | Face, rarely extra-facial | Central facial erythema, flushing, telangiectasia, papules, pustules, eye manifestations |
| Demodex folliculitis | Demodex | Most common on the face | Pustules, papules, follicular plugs |
| Bockhart's impetigo | Staphylococcus aureus | Head, neck, trunk, extremities, buttocks, axillae | Erythematous follicular-based papules or fragile pustules |
| Ofuji's disease | None | Face, less on trunk | Pustules, papules, plaques in annular configuration |
| Actinic superficial folliculitis | Sunlight | Most commonly, a symmetrical eruption on the chest, back, arms, or neck | Numerous small follicular pustules, each surrounded by a small red rim |
| Actinic folliculitis | Sunlight | Face, arms, and upper chest | Pustules, papules, erythema |
| Acute and recurrent facial pustulosis | Sunlight, viral, or none | Chin, forehead, cheek, neck | Tightly clustered, fine pustules on a background of light erythema |
The characteristic features of acne vulgaris are comedones, papules, and pustules over the face, neck, and even the trunk [24, 25]. The onset age of acne vulgaris is 12 to 14 years and the severity peaks at the age 16 to 17 years in females and 17 to 19 years in males [26]. Pathogenesis of acne includes androgen-mediated sebum overproduction, hyperkeratosis of folliclular infundibulum with comedo formation from keratin and sebum retention, bacterial colonisation of trapped sebum, and Inflammatory reaction [25]. On the other hand, the rash in the present study is characterised by tiny, monomorphous, superficial pustules without comedones, papules, and inflamed cystic lesions. The striking female predominance with a peak incidence in the third decade of life as well as topical steroids being much more effective than antibiotics allows its differentiation from acne vulgaris.
Pustules are a common feature in rosacea. A diagnosis of rosacea can be made by phymatous changes or persistent central facial erythema that may periodically intensify, or two or more of the following major features, including facial flushing, papulopustules, telangiectasia, and eye manifestations [1, 2]. Various factors, such as genetics, innate immune system, neurogenic vasodilation and inflammation, vascular hypersensitivity, Demodex, ultraviolet radiation, microbiome, and skin barrier dysfunction are proposed to play some roles in rosacea [27]. In the present study, all patients presented tiny pustules without other aforementioned features of rosacea. Besides, common contributory trigger factors of rosacea were not identified in our cases. One patient developed fixed central facial erythema 1 year later, which might be coincidental or indicative of a pre-rosacea state on rare occasions.
Demodex is a normal flora in the skin. It is considered pathogenic when mites are present in large quantities or penetrate into the dermis. A high Demodex density may provoke papules, pustules, or large pores with follicular plugs on the face and neck [8, 28, 29]. In the present study, demodicosis was excluded by the finding of no Demodex or a low density in each case [22, 23].
Follicular pustules may occasionally be seen in patients with seborrheic dermatitis. In the study of Aktaş KE and Aksu ÇA, Demodex infestation rates were significantly higher in the seborrheic dermatitis groups than in controls [30]. In our experience, the pustules associated with seborrheic dermatitis were either acne lesions or Demodex folliculitis proven by Demodex examination. Bockhart's impetigo, also called follicular impetigo, is caused by Staphylococcal aureus infection [10]. The better treatment response of the pustular eruptions to topical steroids than to antibiotics in our cases mitigates the diagnosis of follicular impetigo.
The pustular eruptions in the present study can be differentiated from Ofuji's disease, a classic type of eosinophilic pustular folliculitis (EPF), by lacking annular configuration, post-inflammatory hyperpigmentation, and eosinophilic infiltrates pathologically. Although cases of non-classic EPF lack annular configuration, the histopathological finding of follicular eosinophilic infiltration is the diagnostic hallmark [31-34]. The histopathology of three patients in the present study showed a superficial follicular pustule filled with neutrophils, and a perivascular and interstitial lymphohistiocytic infiltrate without eosinophils allowing differentiation from Ofuji's disease [5, 31, 32] and non-classic EPF. Pustular allergic contact dermatitis consists of multiple small pustules on a swelling erythematous background. The causative agents include topical antibacterial nitrofurazone, isoconazole nitrate, topical minoxidil 2%, and fragrance. Histological features include epidermal spongiosis and dermal oedema in addition to epidermal pustules composed of lymphocytes and occasional neutrophils [21].
Three other facial pustulosis, though rare need to be differentiated from the pustular eruptions in the present study as well. In actinic superficial folliculitis, the rash appears within 24–48 h after intense sunlight exposure and is characterised by a non-itching eruption of numerous small follicular pustules, each surrounded by a small red rim, most commonly on the chest, back, arms, or neck. The pustules are generally self-limited and resolve within days to a week [14, 35, 36]. Actinic folliculitis is characterised by pustules, papules, and erythema distributed on the face, arms, and upper chest. The rash usually develops 4–24 h after sunlight exposure and may respond to isotretinoin or a topical retinoid [37-39]. Acute and recurrent facial pustulosis manifests as tightly clustered fine pustules on a background of light erythema on the chin, forehead, cheek, and neck. The trigger factor may be sunlight, virus, or none [16, 40].
In the present study, the facial follicular pustulosis was not clearly attributed to any trigger factors. The tiny, monomorphous, superficial pustules, but not papules, were scattered on the cheek, forehead, nose, eyelid, chin, and neck. Most patients required treatment with a total resolution of pustules after topical steroid treatment. The features of discrete pustules with no papules, background erythema or clear trigger factors, in combination with good response to topical steroids make the eruptions in the present study differ from these three sunlight-triggered pustulosis.
C. acnes is abundant in healthy, sebum-rich skin and has been linked to acne [41], atopic dermatitis, rosacea, and psoriasis [42]. Though C. acnes was isolated from the pustules in two patients, the pustules responded rapidly to topical steroids rather than antibiotics. Thus, the role of C. acnes remains uncertain. However, the good treatment response to steroids with complete clearance of pustules in 24 of the 25 (96%) patients favours the noninfectious nature of this eruption.
In sum, in our study, 27 young patients presented with recurrent, monomorphous, discrete, tiny, superficial follicular pustules on the face and neck that resolved rapidly and completely with topical corticosteroids in 96% of the cases. The characteristic clinical features, together with histopathologic findings of three cases, appeared distinct from other common as well as rare facial dermatoses with follicular pustules. We would like to propose the term ‘superficial pustular folliculitis of the face and neck (SPFFN)’ for this condition.
A collection of 27 cases of SPFFN from a single dermatology clinic over a 5-year period suggests that SPFFN might not be very rare. In recollection, the first author encountered his first case with a pustular eruption of the face resembling SPFFN that responded to topical steroids in a young woman about 30 years ago. We were not aware of a specific diagnosis for this type of eruption for couple decades. After we had accumulated more experience in diagnosis and differential diagnosis of various facial papulopustular dermatoses, especially rosacea and demodicosis over many years, then the first author came to recognise the characteristic features of SPFFN. When the first author reported the study of SPFFN in an acne rosacea forum in Taiwan in 2021, only a few dermatologists acknowledged seeing sporadic similar cases. One may wonder whether SPFFN has been underdiagnosed in Taiwan because of lacking a clear documentation of this condition in the literature.
Clinically, SPFFN can be easily confused with rosacea and other facial pustular dermatoses. Before the global consensus on rosacea in 2017, SPFFN might have been confused with rosacea based on the diagnostic criteria for rosacea proposed in 2004, in which the diagnosis of rosacea can be made by the presence of one or more features, including flushing, erythema, papules and pustules, and telangiectasia, with a central face distribution [43]. In Taiwan, the easy access to medical care (including private practices and medical centers), patients often seek medical help from multiple doctors. Given the recurrent nature of SPFFN with good response to topical steroids, the clinicians might treat the patients without considering a more specific diagnosis.
We have been studying cases of demodicosis, rosacea, and eosinophilic pustular folliculitis in the last couple decades in the current private practice and Medical Center, and have published several observational studies [22, 23, 31, 32, 44-55]. Because of the personal interest in facial papulopustular dermatoses, the first author has seen a large number of patients (about 11,160 cases) with facial papulopustular dermatoses, including acne, rosacea, eosinophilic pustular folliculitis and demodicosis in recent 5 years. Among these cases, 27 are of this yet-to-be-documented SPFFN, which accounts for about 0.24% of the patients with facial papulopustular eruptions.
On further communication with dermatologists from northern Taiwan, South Korea, Japan, Canada, Germany, and the Philippines, five dermatologists acknowledged that they had seen a few SPFFN-like cases. To our knowledge, there is no documentation of this type of eruption in the PubMed. Whether SPFFN preferentially affects Taiwanese or Asian remains to be determined by more reports of this condition. We hope that the present study could increase the awareness of this disease by dermatologists and other clinicians in Taiwan and beyond, especially when encountering young females presenting with recurrent facial pustules of unknown cause. It is important to include SPFFN in the differential diagnosis in such cases. The limitations of this study include that all patients were seen in a single dermatologic clinic, limiting the generalisability, and histopathology and bacterial cultures were performed on a limited number of cases. Further studies to expand the sample size for bacterial culture and biopsy, as well as examine the microbiota genome, are necessary to further characterise this clinical condition.
5 Conclusions
We described the clinicopathologic features of SPFFN, which appears to be a distinctive form of noninfectious pustular eruption affecting young females almost exclusively, and can be treated effectively with low-potency topical corticosteroids. Awareness of this particular type of follicular pustulosis, especially when it affects young females, can facilitate early diagnosis of SPFFN and provide appropriate treatment.
Author Contributions
Each author has participated sufficiently in the work and met the conditions (i) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; (ii) drafting the article or revising it critically for important intellectual content; (iii) final approval of the version to be published. Hui-Peng Huang takes responsibility for the integrity of the work, from inception to published article.
Acknowledgements
We thank professors Hsien-Ching Chiu, Guen-Soo Lee, Ken Natsuga, Wenchieh Chen, and Jerry Tan for providing information about cases with similar superficial facial pustules in northern Taiwan, South Korea, Japan, Germany, and Canada.
Ethics Statement
All patients in this manuscript have given written informed consent for participation in the study and the use of their deidentified, anonymized, aggregated data and their case details (including photographs) for publication. This study was approved by the Institutional Review Board of National Cheng Kung University Hospital. IRB No: B-ER-112-422.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.