Analysing referral patterns from a primary dermatological clinic to other medical institutions for further care: A survey on patients with certain skin diseases in Japan
Abstract
Background
Various skin diseases exist; some require specialist treatment. Consequently, patients with these conditions are often referred from primary dermatological clinics to other medical institutions for further secondary or tertiary care. However, it has yet to be fully evaluated at primary dermatological clinics which skin conditions necessitate such referrals.
Objectives
This study aims to identify skin conditions that often require further care when treated at a primary dermatological clinic.
Methods
This study enroled 14,306 patients who had visited the Ueo Dermatology Clinic (a primary dermatological clinic in Saiki City, Oita prefecture, Japan) from 1 January 2020 to 31 December 2022. The following clinical information was examined: the primary disease, age, sex, whether referrals (general or emergency) were made after the clinic visit or not, and the reasons for the referrals.
Results
'Eczema and dermatitis' was the most frequent category in the clinic, although the referral rates for this category were not exceptionally high compared to other categories. A large number of emergency referrals was observed for 'Viral infections (herpes zoster),' 'Drug-induced skin reactions,' and 'Bacterial infections (cellulitis)'; a large number of general referrals was observed for 'Malignant skin tumours and melanomas' and 'Benign skin tumours.' Although low numbers, the rates for general and emergency referrals were high in the categories of 'Blistering Diseases,' 'Connective Tissue Diseases,' and 'Vasculitis, Purpura, and Other Vascular Diseases.' In an analysis of the reasons for the referrals, the following reasons ranked highest: requirement for high-level medical treatment, surgical operation, or hospitalisation, and consultation with doctors in departments other than dermatology.
Conclusions
This study identified several skin conditions often requiring additional care when treated at a primary dermatological clinic. Based on these findings, seamless cooperation between primary clinics and specialised medical institutions is anticipated.
INTRODUCTION
A wide variety of skin diseases exist, many of which are treated not only by dermatologists but also by general physicians, paediatricians and other healthcare providers.1, 2 Some skin diseases require specialist treatment. Consequently, patients with these conditions are often referred from general primary clinics and primary dermatological clinics to other medical institutions for further secondary or tertiary care. However, it has not been fully evaluated at those clinics, which skin conditions necessitate such referrals. Several surveys have indicated that skin diseases are not managed by only dermatologists.3-9 Therefore, identifying which skin conditions often require specialised care beyond primary treatment could be invaluable for many clinicians. In Japan, patients can visit primary dermatological clinics directly without first consulting general primary care physicians, and some are referred from those primary dermatological clinics to other medical institutions for various reasons. We investigated the referral patterns, by skin disease categories, from a primary dermatological clinic to other medical institutions. The Ueo Dermatology Clinic in Saiki City, Oita, Japan, which is the sole clinic specialising in dermatology in the area (2022 population: 67,126), served as the study site. Using the clinic's medical records, we analysed which skin diseases or disease categories were most frequently referred to other medical institutions. This study aims to identify skin conditions that often require further care when treated at a primary dermatological clinic. Although this survey was conducted in a primary dermatological clinic rather than a general clinic, it would be beneficial for many clinicians to know which skin conditions are not resolved at a primary dermatological clinic.
METHODS
Participants
This study enroled 14,306 patients who had visited the Ueo Dermatology Clinic (Saiki City, Oita prefecture, Japan) from January 2020 to December 2022. The Ueo Dermatology Clinic is the sole primary dermatological clinic in Saiki City, a municipality that had a population of approximately 70,000 at the time of the study. At the Ueo Dermatology Clinic, patients were treated only by Daisuke Ueo, M.D., a dermatologist who is the first author of this manuscript. This study was approved by the ethics committee of the Oita University Faculty of Medicine and was performed in accordance with the principles of the Declaration of Helsinki and its subsequent amendments. This study employed the opt-out method for patient consent.
Study design
In this retrospective cohort study, we analysed the patterns of patients being referred from a primary dermatological clinic, Ueo Dermatology Clinic, to various other medical institutions. These institutions include medical centres, university hospitals, and specialised clinics across different specialties for further secondary or tertiary care. Clinical information was collected using the clinical records of the Ueo Dermatology Clinic; specifically, relevant data included primary diseases, age, sex, and whether the patient had been referred to other medical institutions from the Ueo Dermatology Clinic after the visit. Regarding the primary diseases, one disease that was considered the primary indication by Dr. Daisuke Ueo was selected for each patient, and this designation was used to classify individuals into a disease category. The names of skin diseases and their categories were defined based on Shimizus Dermatology.1 Referrals to other medical institutions were classified as either emergency and general referrals. 'Emergency referrals' were defined as patients needing to visit other medical institutions on the same day or the next day following the visit to the Ueo Dermatology Clinic, and represented the patients who needed emergent treatment, and so forth, at other medical institutions. 'General referrals' represented patients not requiring 'emergency referrals' but needing referrals nonetheless. We further collected information on the reasons for the referral, and classified the reasons for the referrals into seven categories: (i) patients hoping to be referred to another institution (including a second opinion); (ii) exact diagnosis was unclear; (iii) hospitalisation was required for treatment; (iv) consultation was required with doctors in departments other than dermatology; (v) specialised, high-level medical examination and/or treatment were required; (vi) surgical operation was required; and (vii) others. Among these seven categories, the most appropriate reason was selected for each referred patient.
RESULTS
Patient demographic information
The demographics of patients treated at the Ueo Dermatology Clinic from 2020 to 2022 are shown in Supporting Information: Table S1. There was no specific sex bias in the total patient population or between the patients who required general or emergency referrals. The median age of the total patient population was 53 years, while the median ages of the general and emergency referrals were 65 and 71 years, respectively, indicating that patients who required referrals were nominally older than those who did not. Table 1 lists the most frequently occurring disease names for each category, including all patients and those who needed general or emergency referrals. Even if a disease appeared often among the patients, this observation did not mean that the category was frequently the basis for general or emergency referrals, indicating a bias in the number of general and emergency referrals. There also did not appear to be overlap between the names of generally referred diseases and those that were emergently referred, indicating that, depending on the type of disease, some diseases were more likely to lead to general referrals and others to emergency referrals.
| All patients, n = 14,306 (cases) | Patients who needed general referrals, n = 249 (cases) | Patients who needed emergency referrals, n = 76 (cases) |
|---|---|---|
| Atopic dermatitis (1236) | Palmoplantar pustulosis (18) | Herpes zoster (36) |
| Contact dermatitis (946) | Basal cell carcinoma (16) | Drug-induced skin reactions (9) |
| Acute eczema (888) | Subcutaneous tumour (12) | Cellulitis (7) |
| Epidermal cyst (12) | ||
| Acne vulgaris (799) | Bowen's disease (11) | Stevens-Johnson syndrome (4) |
| Squamous cell carcinoma (11) | ||
| Other (11) | ||
| Tinea unguium (705) | Atopic dermatitis (9) | Bullous pemphigoid (2) |
| Urticaria (670) | Adult T-cell leukaemia/lymphoma (7) | Arteriosclerosis obliterans (2) |
| Verruca vulgaris (596) | Injury (2) | |
| Herpes zoster (576) | Melanocytic nevi (7) | Systemic lupus erythematosus (1) |
| Insect bite (504) | Ophthalmological tumour (1) | |
| Seborrhoeic dermatitis (356) | Critical limb ischaemia, (1) etc. |
Referral patterns from a primary dermatological clinic to other medical institutions on patients with certain skin diseases
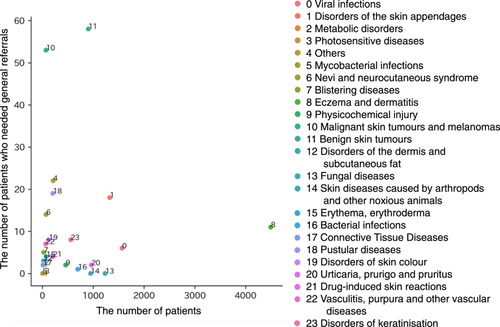
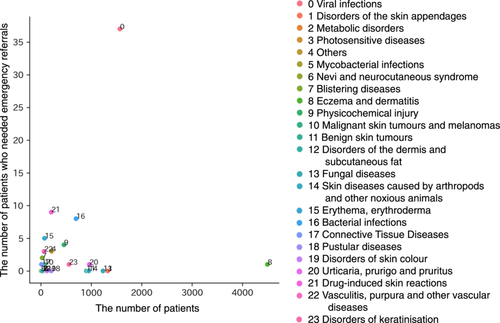
Table 2 summarises the patient numbers and referral rates for each disease category. 'Eczema and dermatitis' was the most frequently seen category (Table 2); indeed, the top-three indications treated in the clinic were 'atopic dermatitis,' 'contact dermatitis' and 'acute eczema' (Table 1). Next, we visualised the critical categories for referrals by generating scatter plots with the numbers of all patients and referrals by disease category (Figures 1 and 2). For general referrals, the categories 'Malignant skin tumours and melanomas' and 'Benign skin tumours' showed high numbers of referrals, even though the combined number of patients in these categories was less than 1000 (Figure 1). For emergency referrals, the number of referrals for the category 'Viral infections' was the highest, followed by those for 'Drug-induced skin reactions' and 'Bacterial infections' (Figure 2). With regard to actual diseases, as shown in Table 1, the number of basal cell carcinoma, squamous cell carcinoma, epidermal cyst and subcutaneous tumour reflected high general referral numbers; the number of herpes zoster, drug-induced skin reactions and cellulitis reflected high emergency referral numbers, in each category. Although low numbers, the rates for general and emergency referrals were high in the categories of 'Blistering Diseases,' 'Connective Tissue Diseases' and 'Vasculitis, Purpura and Other Vascular Diseases' (Table 2). The reasons for the referrals are presented in Supporting Information: Table S2. For both general and emergency referrals, the need for consultation with doctors in departments other than dermatology ranked high among the reasons for referrals. Based on our findings, we provide a summary of the key skin disease categories at a primary dermatological clinic requiring referral to other medical institutions (Supporting Information: Figure S1).
| Category of dermatological disordera | Major diseases included in each categoryb | Cases (n)/general referral rates/emergency referral ratesc |
|---|---|---|
| Eczema and dermatitis | Atopic dermatitis, acute eczema, contact dermatitis and seborrhoeic dermatitis | 4495/0.24%/0.02% |
| Viral infections | Verruca vulgaris, herpes zoster, herpes simplex and molluscum contaginosum | 1567/0.38%/2.36% |
| Disorders of the skin appendages | Acne vulgaris, rosacea and alopecia areata | 1325/1.36%/0.00% |
| Fungal diseases | Tinea pedis, tinea unguium, Candida intertrigo and malassezia folliculitis | 1233/0.00%/0.00% |
| Urticaria, prurigo, and pruritus | Urticaria, acute prurigo and chronic prurigo | 961/0.21%/0.10% |
| Skin diseases caused by arthropods and other noxious animals | Insect bite, tick bite and caterpillar dermatitis | 948/0.00%/0.00% |
| Benign skin tumours | Seborrhoeic keratosis, epidermal cyst, pyogenic granuloma and ganglion | 903/6.31%/0.00% |
| Bacterial infections | Cellulitis, impetigo, folliculitis and furuncle | 697/0.14%/1.15% |
| Disorders of keratinisation | Ichthyosis vulgaris, psoriasis vulgaris, callus and clavus | 557/1.44%/0.18% |
| Physicochemical injury | Burn, traumatic injury, pernio and ulcer | 457/0.44%/0.88% |
| Others | Aphtha, cheilitis, neuropathy and psychiatric disorders | 212/10.85%/1.42% |
| Drug-induced skin reactions | Drug-induced skin reaction and fixed drug eruption | 205/1.95%/4.39% |
| Pustular diseases | Palmoplantar pustulosis | 205/9.27%/0.00% |
| Disorders of skin colour | Vitiligo vulgaris, melasma and senile lentigo | 121/6.61%/0.00% |
| Erythema, erythroderma | Erythema multiforme, eczematous erythroderma, erythema annulare centrifugum and Stevens–Johnson syndrome | 72/5.56%/6.94% |
| Malignant skin tumours and melanomas | Squamous cell carcinoma, basal cell carcinoma, actinic keratosis and Bowen's disease | 70/75.71%/1.43% |
| Nevi and neurocutaneous syndrome | Melanocytic nevi, nevus of Ota and sebaceous nevus | 70/20.00%/0.00% |
| Vasculitis, purpura, and other vascular diseases | IgA vasculitis, pigmented purpuric dermatosis, senile purpura and purpura simplex | 62/11.29%/4.84% |
| Photosensitive diseases | Photosensitivity and sunburn | 51/0.00%/0.00% |
| Metabolic disorders | Lichen amyloidosis and xanthelasma palpebrarum | 39/5.13%/0.00% |
| Blistering diseases | Bullous pemphigoid | 24/20.83%/8.33% |
| Disorders of the dermis and subcutaneous fat | Erythema nodosum and granuloma annulare | 21/14.29%/0.00% |
| Connective tissue diseases | Discoid lupus erythematosus, systemic lupus erythematosus, localised sclerosis and dermatomyositis | 10/20.00%/10.00% |
| Mycobacterial infections | Mycobacterium marinum | 1/0.00%/0.00% |
- a All skin diseases treated in the Ueo Dermatology Clinic were classified into a category. The categories are arranged in descending order of the number of patients.
- b Major diseases from each category, treated at Ueo Dermatology Clinic, are listed, with up to four diseases per category.
- c The number of patients of each category treated in the Ueo Dermatology Clinic, and general and emergency referrals rates (percentages; calculated as referral cases/total cases in each category × 100) are shown.
DISCUSSION
Although several studies have investigated referred patients with skin conditions at hospitals, including urgent consultations at dermatology departments, surveys at primary dermatological clinics like this study are lacking.10-14 The differences between the results at a primary dermatological clinic and those at hospitals are interesting. The results of cutaneous infection, including herpes zoster and cellulitis and cutaneous adverse drug eruptions are shared between a primary dermatological clinic and hospitals. Indeed, multiple severe complications of herpes zoster are known, for example, acute encephalitis, keratitis and motor paralysis, resulting in severe prognoses.15, 16 Moreover, cellulitis is the most common reason for skin-related hospitalisation17; sometimes, urgent drug change or discontinuation should be considered for patients with adverse drug eruptions, requiring hospitalisation or consultation with physicians of departments other than dermatology.18-20 These match the reasons for emergency referrals (Supporting Information: Table S2). On the other hand, eczema occupied a large number of referred patients with skin conditions at hospital analyses,10-14 but not our analysis. Although this discrepancy may be caused by the fact that this survey was conducted at a dermatological clinic, multiple referred patients with eczema were included in our survey (Figure 1); however, more than that, numerous patients with eczema were treated at our clinic. Conversely, skin tumours are inconspicuous in hospital analyses because of their low number.10-14 Analyses at hospitals are precious, but our survey at a primary dermatological clinic highlights skin conditions during primary care. Notably, 'Blistering Diseases,' 'Connective Tissue Diseases,' and 'Vasculitis, Purpura, and Other Vascular Diseases' were very rare in both surveys. However, they showed high rates of referrals from the primary dermatological clinic to other medical institutions. This information allows general primary clinicians to judge smooth referrals to other medical institutions for further secondary or tertiary care.
This study had two limitations, as follows. (i) This study was performed in Japan, and disease epidemiology and the medical system's response will vary by region and country. (ii) The results of the present study were derived from a single institution and dermatologist.
This study identified several skin conditions often requiring additional care when treated at a primary dermatological clinic. Based on these findings, seamless cooperation between primary clinics and specialised medical institutions is anticipated.
AUTHOR CONTRIBUTIONS
Conceptualization: Takashi Sakai. Data curation: Daisuke Ueo. Formal analysis: Erika Ochiai and Jun Sese. Investigation: Daisuke Ueo. Methodology: Takashi Sakai. Project administration: Takashi Sakai. Resources: Daisuke Ueo. Supervision: Takashi Sakai and Yutaka Hatano. Visualisation: Daisuke Ueo, Takashi Sakai, Erika Ochiai, and Jun Sese. Writing—original draft preparation: Daisuke Ueo and Takashi Sakai. Writing—review and editing: All authors.
ACKNOWLEDGEMENTS
We thank Masami Mishiro, a member of the staff of Saiki City Hall, for assistance in determining the population of Saiki City. There were no funders for this research project.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
This study was approved by the ethics committee of the Oita University Faculty of Medicine and was performed in accordance with the principles of the Declaration of Helsinki and its subsequent amendments. This study employed the opt-out method for patient consent.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




