A tricky singular papular peri-cicatricial mammarian lesion
Abstract
Breast cancer represents the most common malignancy in women worldwide. In most cases, metastasis is the leading cause of mortality. Early diagnosis is still challenging despite standardised, government-led screening programs, but is crucial in achieving improved survival rates. Additionally, a deeper understanding of the metastatic potential of breast cancer is critical for developing therapeutic interventions to combat widespread disease. Cutaneous metastasis from underlying breast carcinoma is uncommon as the first manifestation of visceral malignancies and is commonly observed in advanced-stage malignancies, often associated with poor prognosis, and a prompt, precise tissue diagnosis is mandatory. A high index of suspicion in oncologic patients is required to diagnose these lesions, as they can mimic benign skin manifestations and clinical findings may be subtle and going unnoticed. We report on a case of a 76-year-old female patient presenting to our non-invasive diagnostic outpatient clinic with an unusual cutaneous presentation, as an early sign of locally advanced invasive ductal carcinoma breast cancer recurrence. The aim of our article is to underline the importance of the dermatologist in the multi-disciplinary oncologic diagnostic process, including non-invasive imaging evaluation of cutaneous lesions, especially insidious breast carcinomas. Dynamic optical coherence tomography (D-OCT) is not routinely used due to its cost, therefore lesion's aspect has not been completely described, consequently, the correct evaluation of skin architecture appearance can add important information, especially in cutaneous oncology where it can help in early diagnosis or cancer recurrency. OCT may contribute to the detection of subclinical cutaneous manifestations of cancer or recurrence, in particular, when they are difficult to differentiate clinically from benign lesion. In the case we described, OCT of suspected lesion showed the loss of the DEJ with solid nests and irregular vessels.
Capsule Summary
Breast cancer, a leading cause of mortality in women globally, often metastasizes to distant sites, including the skin. We present a case that underlies the importance of dermatological assessment in the multi-disciplinary diagnostic process of metastatic disease, including non-invasive imaging evaluation of cutaneous lesions. Dynamic optical coherence tomography may contribute to the detection of subclinical cutaneous manifestations of cancer or recurrence, in particular, when they are difficult to differentiate clinically from benign lesion.
INTRODUCTION
Breast cancer represents the most common malignancy in women worldwide, accounting annually for 12.5% of all new cancer diagnoses.1 Invasive ductal carcinoma (IDC) represents the most common histological subtype of invasive breast cancer. Milk ducts are first affected before subsequent lymphatic invasion and metastasis.2 In most cases, metastasis is the leading cause of mortality. The incidence of breast carcinoma cutaneous manifestations (BCCM) is close to 23%. The most common sites include the chest wall and abdomen, extremities, and the head/neck region.3 Nodules are the most common clinical presentation of BCCM. They are multiple, firm and located in the dermis or subcutis, the colour can vary from normal skin to purple or brown.4 In our case, there was just one asymptomatic pinky lesion, easily confusing with sebaceous cyst or dermatofibromas. The peri-cicatricial location allowed us to perform additional evaluation, and the quick scan made by dynamic optical coherence tomography (D-OCT) showed an abnormal skin aspect associated with the presence of serpentine vessels, suspicious for a neoplastic nature of the lesion with the prompt surgical excision.
CASE REPORT
A 76-year-old female patient presented to our non-invasive diagnostic imaging dermatological outpatient clinic, complaining about an enlarging, although asymptomatic papular pink lesion on her right upper-outer breast quadrant. She was otherwise healthy, with no underlying chronic conditions and not taking any medication.
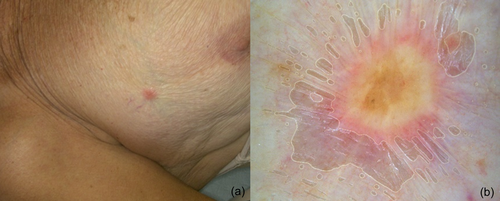
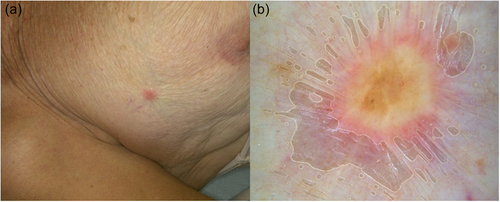
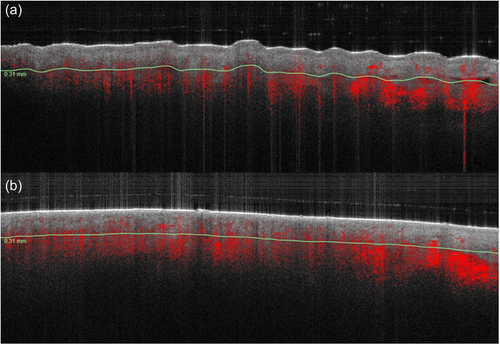
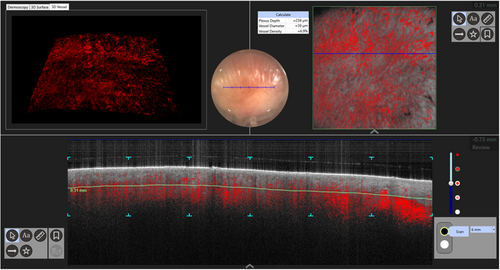
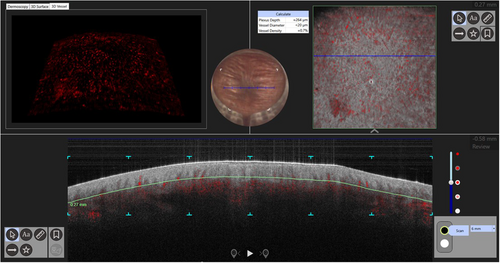
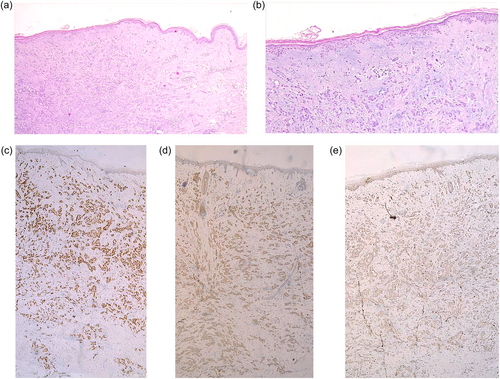
Her personal and family history for cutaneous malignances were negative. Medical history was notable for breast carcinoma on her right side 20 years earlier, histologically defined as Luminal-A (ER-positive and HER2-negative), pT1N1M0, stage IIA. She underwent conservative surgery and lymphadenectomy, followed by radio-chemotherapy and hormone therapy, with complete healing after 5 years. Three years later she had a relapse of the same histopathological entity, again on the right side and upon combined management with surgery and radiotherapy, was declared disease-free. She was recently referred to us by oncologist for the evaluation of the new skin lesion. Clinical examination showed the presence of a 0.5 × 0.5 cm erythematous, infiltrated, firm pink papular lesion on her right upper-outer breast quadrant (Figure 1a). Dermoscopy showed a poorly defined, yellowish, scar-like lesion, with an erythematous halo and short, fine polymorphic aspecific telangiectasias, with some peripheral brown dots yielding a dermatofibroma-like pattern (Figure 1b). According to literature, the classic dermatoscopic features of a benign lesion such as dermatofibroma, is characterised by a central scar-like white patch and a peripheral pigment network which gradually fades into the surrounding skin. In addition, linear vessels (9.2%), hairpin vessels (2.1%), glomerular vessels (1.4%), comma vessels (0.7%) and polymorph vessels (4.2%) can be seen in benign lesions.5 To better characterise it, non-invasive D-OCT imaging was performed as additional diagnostic modality to exploratively see what the lesion would look like. VivoSight Dx1302 by Michelson Diagnostics Ltd produced in Kent UK, was used for imaging. This showed a physiological clear distinction between the dermo-epidermal junction (DEJ), in the peripheral part of the lesion (Figure 2a) whilst centrally, there was a dramatic structure change, the contrast between epidermis and papillary dermis was not visible due to the loss of the DEJ, with solid nests leading to a chaotic imaging pattern (Figure 2b). Enhanced vascularisation of the epidermis and dermis and distorted serpentine vessels (vessel diameter = 39 μm, vessel density = 6.9%) excluded the hypothesis of a benign lesion (Figure 3). D-OCT aspect of dermatofibroma is characterised by well-defined contrast between epidermis and papillary dermis with bright hyper-reflective dermal structures arranged in thick bundles and epidermal hyperplasia, with minimal vasculature or tissue fluid spaces (Figure 4).6 Taking into account the different aspect of our lesion, wide excision was performed due to the high index of suspicion for neoplastic recurrence. The histopathological examination confirmed the presence of dermal localisation of primary IDC Breast Cancer, “no special type”, with moderate differentiation (G2) (Figure 5).
DISCUSSION
Breast carcinoma appears to be the most common cause (69%) of cancerous cutaneous manifestation in women, uncommon in other malignancies.1 These presentations often mimic benign skin lesions, presenting most commonly as localised nodules, cicatricial or fibrotic plaques, neoplastic alopecia, zosteriform eruptions, or bullous lesions.3-7 The diagnosis is often challenging, as clinical findings may be subtle. Cutaneous manifestation of breast carcinoma is reported in up to 23% of female cases, as nodular lesion ranging from 1.5 to 2.0 cm of diameter.7, 8 In contrast, male counterparts typically exhibit thickened erythematous papules.1 Disease recurrence is more frequent in the first 5 years postresection. Our patient presented with a singular, asymptomatic erythematous papular type lesion, whose histology was consistent with locally advanced breast cancer, which is the most potentially curable disease form.9 Therefore, early diagnosis is mandatory but challenging. Research has shown that LABC does not represent a single entity but encompasses a heterogeneous group of breast tumours favoring loco-regional spread instead of distant metastasis. It still causes significant morbidity and mortality.10 This cutaneous presentation of IDC Breast Cancer underlines the importance of dermatological assessment in the multi-disciplinary diagnostic process, including non-invasive imaging evaluation (by optical coherence tomography OCT, an emerging useful tool which allows real-time cross-sectional imaging with high resolutions comparable to histology avoiding tissue destruction), as skin metastasis can represent the first manifestation of malignancy. This leads to earlier diagnosis, improving patient stratification, with potentially streamlined management and improved prognosis.
AUTHOR CONTRIBUTIONS
Carmen Cantisani: Conceptualization. Luca Gargano, Federica Trovato, Antonio Di Guardo, Alexandru Bâja Vasile and Giulia Azzella: Data curation. Carmen Cantisani, Antonio Di Guardo, Federica Trovato, Emanuele Rovaldi, Tiziana Lettera and Giuseppe Soda: Investigation. Antonio Di Guardo and Emanuele Rovaldi: Methodology. Giovanni Pellacani: Supervision. Carmen Cantisani, Iolanda Speranza, Michela Roberto and Giuseppe Soda: Validation. Antonio Di Guardo and Emanuele Rovaldi: Visualisation. Carmen Cantisani, Federica Trovato, Luca Gargano Alexandru Bâja Vasile, Antonio Di Guardo, Giulia Azzella and Emanuele Rovaldi: Writing—original draft preparation. Giuseppe Soda, Michela Roberto, Iolanda Speranza and Giovanni Pellacani: Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
ACKNOWLEDGMENTS
We would like to thank Jon Holmes CEO Michelson Diagnostics Ltd and our nurse Mrs. Sonia Tofani, Dr Noah Musolff. This research received no external funding.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
All patients in this manuscript have given written informed consent for participation in the study and the use of their deidentified, anonymized, aggregated data and their case details (including photographs) for publication. Ethical approval: not applicable.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.