Impact of Sonographer Experience, Insonation Angle, and Bladder Filling on Uterine Artery Doppler Measurements in the First Trimester of Pregnancy
Sabrina Einig and Cécile Monod equally contributed to the present manuscript.
This work has been presented as an electronic poster at the ISUOG World Congress 2022 and at the Ultraschall Dreiländertreffen 2022 (Meeting of the Austrian, German, and Swiss Societies for Ultrasound in Medicine) as a short oral presentation.
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Abstract
Objective
To investigate the influence of different measurement conditions and ultrasound training level on uterine artery pulsatility index (UtA-PI) measurements as required for combined first trimester preeclampsia (PE) screening.
Methods
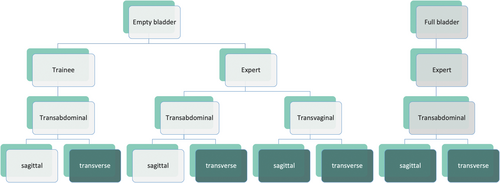
This was a prospective study of consecutive patients with singleton pregnancies presenting for an ultrasound examination between 11 and 14 weeks' gestation. UtA-PI measurements were conducted by residents in training and repeated by experienced sonographers thereafter. UtA-PI measurements were conducted under different examination conditions. First, the trainee sonographers performed transabdominal sagittal and transverse UtA-PI measurements without bladder filling. These measurements were then repeated by the expert sonographers. Additionally, the expert sonographers also performed transvaginal UtA-PI measurements and transabdominal measurements with bladder filling. Statistical analysis was conducted with the statistical software R and included descriptive statistics as well as 2-sided paired t tests.
Results
A total of 100 women were included in the study. Mean age was 31.7 ± 4.92 years and mean gestational week was 12.5 ± 0.53 weeks. A total of 56% were nulliparous and 44% were parous. UtA-PI was significantly lower if performed by a sonographer in training versus an experienced sonographer (P = .031). No significant difference was observed in comparing transverse and sagittal techniques (P = .241). There was also no significant difference in transabominal versus transvaginal measurements (P = .806) and with an empty versus full bladder (P = .444).
Conclusion
Experience of sonographer has a significant impact on UtA-PI. Supervised onsite training is necessary to improve reliability and consistency of UtA-PI measurements and make PE screening reliable for implementation in a universal screening setting.
Abbreviations
-
- BMI
-
- body mass index
-
- CRL
-
- crown-rump length
-
- FMF
-
- Fetal Medicine Foundation
-
- IQR
-
- interquartile range
-
- ISUOG
-
- International Society of Ultrasound in Obstetrics & Gynecology
-
- LDA
-
- low-dose acetylsalicylic acid
-
- PE
-
- preeclampsia
-
- PSV
-
- peek systolic velocity
-
- SD
-
- standard deviation
-
- UtA-PI
-
- uterine artery pulsatility index
Preeclampsia (PE) is a potentially life-threatening pregnancy-associated condition and a major cause of maternal and perinatal morbidity and mortality. Between 2% and 3% of all pregnant women worldwide are described to be affected by this condition.1 Recent data show that a risk prediction, that is, identifying women at high risk of developing PE can already be achieved in the first trimester of pregnancy.2-5 This is especially important because the incidence of preterm PE can be reduced by administration of low-dose acetylsalicylic acid (LDA) starting before the 16th week of gestation.6-10
Currently, the most accurate prediction of PE is achieved by a combined first-trimester screening test. This includes a risk calculation based on prior risks from maternal factors, mean arterial blood pressure, serum levels of placental growth factor, and Doppler-sonography assessing uterine artery pulsatility index (UtA-PI). The sensitivity of this combined test is described to be 75% for PE before 37 weeks of gestation, with a false positive rate of 10%.2 Prophylactic administration of LDA before 16 weeks of gestation reduces the incidence of early PE (before 34 weeks of gestation) by 82% and PE with onset before 37 weeks of gestation by 62% with a number needed to treat of 36.11
As a result of the evidence on the effectiveness of first-trimester PE screening and consecutive administration of LDA in randomized controlled trials,3, 11 screening programs are being built up in many different countries.12-14
One of the major challenges for the broad implementation of first trimester PE screening is the standardized and reliable measurement of UtA-PI. As suggested by the Fetal Medicine Foundation (FMF) London, measurements should be performed transabdominally in a sagittal plane of the uterus by tilting the transducer from side to side and using color Doppler to identify the uterine artery alongside the uterus at the level of the internal os.15
There is limited data on the variability of the Doppler measurements when applied with different examination conditions and by examiners with different levels of training.
The aim of this study was to prospectively investigate the impact of bladder filling, insonation angle, operator experience, as well as intra- and interrater agreement on uterine artery Doppler measurements.
Materials and Methods
We conducted this prospective study at the University Hospital Basel between March 2020 and January 2022. Consecutive patients with singleton pregnancies between 11 + 0 and 13 + 6 weeks of gestation who presented for routine first trimester screening visits were included. All were offered combined first trimester PE risk estimation. Multiple pregnancies, the presence of structural fetal abnormalities including increased nuchal translucencies above the 95th percentile, and women who had already been taking LDA were excluded.
The study was approved by the ethical review board of Northwest- and Central Switzerland (EKNZ) Project-ID 2019-02183. All study participants signed an informed consent.
At recruitment, we collected data on maternal demographics (age, ethnicity, smoking status, history of prior pregnancies and comorbidities, and use of assisted reproductive technologies), and measured the participant's weight and height for the calculation of body mass index (BMI).
Patients with pregnancies at the gestational age from 11 + 0 to 13 + 6 weeks were recruited. Gestational age was confirmed by measurement of the crown-rump length (CRL). Only patients with CRL measurements of 45–84 mm were included.
Each participant was examined by a sonographer in training (trainee) and an experienced sonographer (expert). Trainees were resident doctors with at least 2 years of training in Obstetrics and Gynecology and basic knowledge in scanning techniques that were assigned to a 6-month ultrasound rotation in the specialized unit and thus being new to UtA Doppler sonography in the first trimester of pregnancy. To prepare for the study measurements of UtA-PI, trainees were instructed personally by their supervisor and were required to have completed the FMF online educational course on PE screening. The practical and theoretical training had to be completed after 2 weeks on the rotation and the supervisor needed to check and confirm that the trainee had the skills to participate in the study. Experts were certified level II or III examiners according to the regulations of the Swiss society of ultrasound in medicine specializing in fetal medicine and certified for uterine artery Doppler measurement by the FMF. Further, PE screening has been shown to perform comparable to the FMF data in our center.13 First, measurements were performed according to the guidelines of the FMF16 and the International Society of Ultrasound in Obstetrics & Gynecology (ISUOG)17 transabdominally in a sagittal plane of the uterus by tilting the transducer from side to side and using color Doppler to identify the uterine artery alongside the uterus at the level of the internal os.15
All patients were asked to empty their bladder immediately prior to the examination. For the study UtA Doppler variables were first assessed by a trainee after theoretical training transabdominally in a sagittal and transverse plane. Measurements were then repeated by the expert using both, the sagittal and transverse approaches with the transabdominal probe. As a second step, measurements were repeated by experts with a transvaginal probe in the transverse and sagittal planes. The third step was completed at least 30 minutes after the initial measurements with a filled bladder by an expert with transabdominal measurements in sagittal and transverse planes. So, steps 2 and 3 (transvaginal measurements and transabdominal measurements with filled bladder) were performed only by experts (Figure 1).
The experts ensured that the measurements of the trainees were adequate.
All examinations were performed on the patients right uterine artery with high-quality ultrasound machines (GE Voluson E10, Philips Epic Elite) with high-resolution ultrasound probes (for transabdominal measurements 2D Convex Probe C2-9-D, Frequency: 3–9 MHz or Convex Matrix Array Volume Probe RM6C, Frequency: 2–6 MHz and for transvaginal measurements endocavity Volume Probe RIC6-12-D, Frequency: 5–13 MHz).
Sagittal and Transverse Technique
The transducer was used to display a mid-sagittal view of the uterus and cervix. The transducer was then moved laterally to identify the uterine vessels as aliasing vessels alongside the cervical canal using color Doppler. For the transverse technique, the transducer was rotated by 90° and the uterine artery was located in the same manner (Figure 2, A and B).
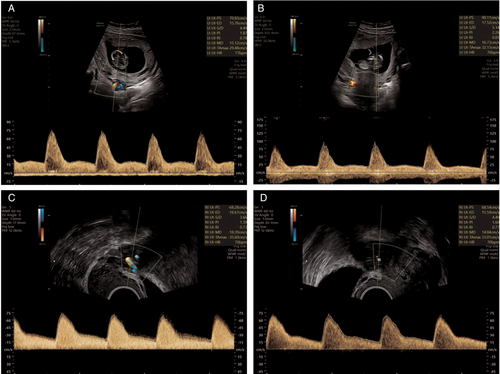
Transvaginal Measurements
The transvaginal examination was performed by the experts. The transvaginal probe was placed in the anterior fornix of the vagina and moved laterally. Paracervical vessels were identified using the color Doppler. The same criteria for the identification of the correct vessels were applied according to FMF and ISUOG Practice guidelines15, 17 (Figure 2, C and D).
Statistical Analysis
Descriptive statistics is presented as counts and frequencies for categorical data and mean ± standard deviation (SD) or median (interquartile range [IQR]) for metric or ordinal variables. Different insonation methods were each compared separately using 2-sided paired t tests.
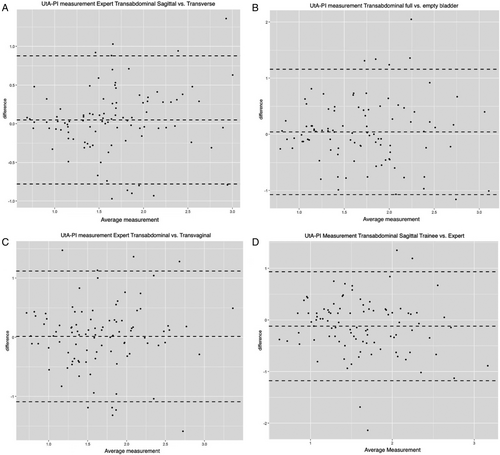
In order to compare intra- and interobserver agreements, Bland–Altmann plots with limits of agreements were calculated and displayed.
A P-value <.05 is considered as significant. All evaluations were done using the statistical software R (versions 4.1.2 and 4.1.3).
Results
A total of 100 women were included in the study between the years 2020 and 2022. The mean age was 31.7 ± 4.92 years. Mean gestational week was 12.5 ± 0.53 weeks. 56% of the study participants were nulliparous and 44% were parous. Mean BMI was 23.6 ± 4.37 kg/m2. Further details on the demographics of our study population can be found in Table 1.
| Maternal characteristics | |
|---|---|
| Age (years), mean (SD) | 31.7 (4.92) |
| BMI (kg/m2), mean (SD) | 23.6 (4.37) |
| Ethnicity, n (%) | |
| Caucasian | 78 (78) |
| Black | 6 (6) |
| East-Asian | 6 (6) |
| South Asian/Indian | 10 (10) |
| Obstetric history | |
| Weeks of gestation, mean (SD) | 12.5 (0.53) |
| Conception, n (%) | |
| Spontaneous | 98 (98) |
| ICSI | 1 (1) |
| IVF | 1 (1) |
| Nulliparous | 56 (56) |
| Parous | 44 (44) |
| PE in previous pregnancy | 0 (0) |
| SGA in previous pregnancy | 2 (4.55) |
| Medical history, n (%) | |
| Smoker | 3 (3) |
| Diabetes mellitus | 0 (0) |
| Chronic hypertension | 1 (1) |
| SLE | 0 (0) |
| APLS | 0 (0) |
| Family history positive for PE, n (%) | |
| No | 98 (98) |
| Unknown | 2 (2) |
- Categorical variables are shown as n (%) and continuous variables are shown as mean (SD).
In total 10 trainee examiners participated in the study. The median number of examinations per trainee was 6.5 (IQR 3.25–13.75). Nine expert examiners participated in the study. The median number of examinations by experts was 9 (IQR 2–21.5). When comparing the different insonation methods, we did not observe any significant intraobserver differences in the measurements of UtA-PI between transabdominal transverse and sagittal approaches (P = .241 for experts and P = .054 for trainees, respectively) (Table 2). There was also no significant difference in UtA-PI measurements with a sagittal insonation angle performed via transabdominal versus transvaginal route (P = .806) and with an empty versus filled bladder in the transabdominal sagittal approach (P = .444) (Table 2 and Figure 3).
| UtA Variable | Sagittal, Mean (SD) | Transverse, Mean (SD) | P | |
|---|---|---|---|---|
| Trainee | UtA-PI | 1.57 (0.54) | 1.65 (0.55) | .054 |
| PSV | 86.16 (20.87) | 83.08 (27.32) | .166 |
| UtA Variable | Sagittal | Transverse | P | |
|---|---|---|---|---|
| Expert | UtA-PI | 1.68 (0,60) | 1.63 (0.55) | .241 |
| PSV | 86.70 (20.84) | 80.55 (23.47) | .025 |
| UtA Variable | Sagittal, Empty Bladder | Sagittal, Full Bladder | P | |
|---|---|---|---|---|
| Different bladder filling | UtA-PI | 1.68 (0.60) | 1.72 (0.60) | .444 |
| PSV | 86.70 (20.84) | 81.98 (23.03) | .18 |
| UtA Variable | Sagittal Transabdominal | Sagittal Transvaginal | P | |
|---|---|---|---|---|
| Transabdominal vs. transvaginal | UtA-PI | 1.68 (0,60) | 1.67 (0.59) | .806 |
| PSV | 86.70 (20.84) | 73.71 (23.92) | <.001 |
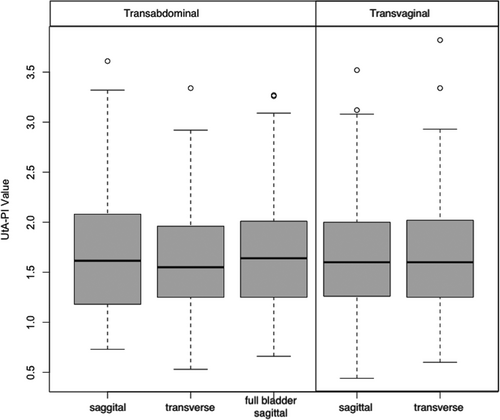
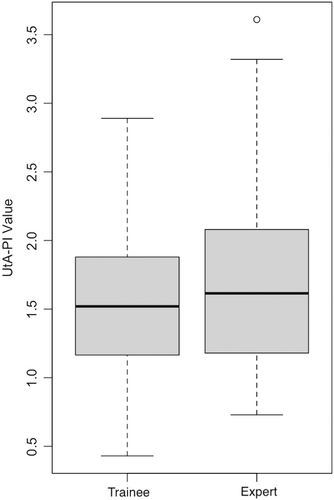
When comparing trainee and expert measurements, there was a significant difference in UtA-PI results if performed by a sonographer in training versus an experienced sonographer (UtA-PI mean 1.57 [± 0.54] for trainees versus 1.68 [±0.60] for experts; P = .031) (Figure 4).
When investigating transvaginal ultrasound with transabdominal sagittal UtA-PSV measurements, the transvaginal approach had a significantly lower peek systolic velocity (PSV) (P < .001) while differences in UtA-PI were not statistically significant (P = .806) (Table 2).
Figure 5 shows the Bland–Altman plots of the intra- and interobserver agreement between trainees and experts and different measurement conditions of UtA-PI measurements. No systematic measurement bias could be found between the measurements since the mean of differences was close to 0 in all cases. Level of agreement showed to be most variable when comparing the differences between measurements performed by trainees versus experts (Figure 5D) and with transabdominal versus transvaginal ultrasound (Figure 5C). The most comparable results were achieved when comparing sagittal versus transverse UtA-PI measurements performed transabdominally (Figure 5A).
Discussion
In our study, the experience of the sonographer is the only parameter investigated with a significant impact on UtA-PI. Other parameters influencing the measurements such as sagittal or transverse approach, transabdominal or transvaginal route, and bladder filling did not have a significant effect.
Other studies investigating intra- and interobserver reproducibility of UtA-PI measurements showed similar results. Marchi et al compared measurements performed via the transabdominal versus transvaginal route by the same examiner and found out that intraobserver reproducibility was sufficient.18 But when comparing measurements by experts versus less experienced sonographers, the level of agreement, thus reproducibility, turned out to be poor.18, 19 These findings are in agreement with the results of our study. Our results also show a significant difference when comparing the measurements performed by trainees versus experts (UtA-PI mean 1.57 [±0.54] for trainees versus 1.68 [±0.60] for experts; P = .031). The discrepancy in mean differences is displayed in the wide limits of agreement in the Bland–Altman plot (Figure 5D), which is most prominent when comparing UtA-PI measurements conducted by trainees with those performed by experts.
Drouin et al showed that the transverse approach is equivalent to the standard sagittal method, with no significant difference in UtA-PI,20 which is in line with our study. The most comparable results in our collective were achieved when comparing sagittal versus transverse UtA-PI measurements performed transabdominally (Figure 5A). In Drouin et al's study, sonographers found the transverse technique subjectively easier. Especially since this method facilitates locating the uterine artery at the level of the internal os of the cervix uteri.20 Other authors were even able to quantify this by demonstrating that time to achieve a correct measurement was significantly lower when using the transverse approach.21
Ridding et al demonstrated that when measuring too far distantly from the internal os, UtA-PI and PSV was significantly lower proving that measurements are sample site dependent.22 Chaemsaithong et al demonstrated a linear relation between the distance from the internal os and the decrease in UtA-PI.23 Furthermore, inexperienced sonographers have a tendency of measuring with more distance to the internal os.23 In our study the mean UtA-PI was lower in measurements conducted by trainees compared to those performed by experts. This could also imply that trainees have difficulties to find the uterine artery close to the internal os.
Another factor influencing distance to the optimal sample site is bladder filling. Kongwattanakul et al suggest that the transverse measurements are only comparable to the sagittal one if the bladder depth is less than 5 cm.21 In our study, we did not see a significant impact of bladder filling on UtA-PI.
When comparing the transabdominal versus transvaginal route, other authors found that UtA-PI was significantly higher measured transvaginally. This approach seems to be especially useful in obese patients.18, 19, 24 Interestingly, in our study, the results did not confirm previous findings. Transvaginal ultrasound had a significantly lower PSV while differences in UtA-PI were not statistically significant. Our findings seem biologically understandable since it is more challenging and sometimes impossible to get a low insonation angle to the vessel when examining via the transvaginal route. Since there was no significant difference in UtA-PI, this measurement seems to be a good and reliable alternative in patients where the transabdominal route is not feasible.
Our study results imply that there is a need to systematically train the examiners on measurement of the uterine artery in the first trimester before introducing PE screening into routine clinical care. Our data show that the single parameter having a significant impact on UtA-PI is the training level of the sonographer.
Limitations of our work include that the time to achieve correct measurements was not quantified. This would have been another useful tool for accelerated supervised onsite training of inexperienced sonographers. One study investigating quality standards in UtA-PI measurements found that feedback to operators led to improved measurement performance thus improving screening accuracy.25 In our study, experts were not blinded to the results of trainees and vice versa.
The main strength of our study is the prospective study design. The conditions were representative of actual clinical situations, and we believe can therefore be considered generalizable. The results of our study show the importance of training of Doppler measurements that should be considered when implementing nationwide screening for PE.
A standardized measurement protocol seems reasonable and important for training. However, in the hands of experienced examiners, it seems possible to use alternative routes and insonation angles as well as different levels of bladder filling without significant impact on UtA-PI values.
Conclusion
Supervised onsite training of inexperienced sonographers could improve reliability and consistency of UtA-PI measurements and is needed for the broad implementation of first-trimester PE screening.
Acknowledgment
Open access funding provided by Universitat Basel.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




