Does the use of intraoperative frozen section of bone marrow from the cut end of the mandible help assess the adequacy of bone margins following mandibulectomy for oral cancer?
This study was presented at IFHNOS 2023 (June), Rome Italy.
Abstract
Background
The adequacy of the cut end of the mandible following a segmental mandibulectomy done for oral cancer intraoperatively is at times assessed using a frozen section (FS) of the bone marrow (BM) at the cut ends. The study aimed to assess its utility to guide the intraoperative decision on the adequacy of bony margins.
Materials and Methods
All patients with oral squamous cell carcinoma (OSCC) who underwent segmental mandibulectomy from January 2012 to December 2021 at our institute and for whom intraoperative FS of BM was utilized were included. We analyzed the sensitivity, specificity, and positive and negative predictive value (PPV, NPV) of this in predicting positive bone margins.
Results
A total of 457 patients were included in the study. The majority of the cases were per premium cases (n = 372, 81.4%). The median age of the cohort was 52 years (range: 22–80 years). Most patients had T4 disease (n = 406, 88.8%). On FS, BM was positive in only 18 patients (3.9%) for whom the bone margin was revised. BM biopsy report in the final histopathology was positive in 12 patients (2.2%). The sensitivity, specificity PPV, and NPV were 52.3%, 98.65%, 64.7%, and 97.7% respectively. No factors predicting BM positivity on FS could be identified in this cohort.
Conclusions
The BM FS was positive in only a small percentage of patients, and it helped in reducing the bone margin positivity rate from 3.9% to 2.2% only. Hence the intraoperative BM FS seems to have limited utility as seen from our study.
1 INTRODUCTION
Oral squamous cell carcinoma (OSCC) is a common cancer in India and surgery forms an integral part of management. Achieving negative margins surgically has important prognostic implications, as positive margins have poor survival outcomes.1 The role of intraoperative frozen section (FS) in achieving negative mucosal and soft tissue margins is well established while the same for bony margins is not well known.2, 3 Although various intraoperative methods have been used to assess the bony margin in patients undergoing surgery for OSCC, bone marrow (BM) from the cut end of the mandible for the FS is one of the commonly used methods and a simple procedure that can be replicated.4, 5 Literature on the efficacy of BM FS is sparse with few studies published with small numbers. The cost–benefit ratio for the FS has also been questioned recently.6 The purpose of this study was to assess the usefulness of intraoperative FS assessment of BM to guide the decision on the adequacy of bony margins in patients undergoing segmental mandibulectomy for oral cancers. We hypothesize that there is limited utility for intraoperative FS assessment of BM for adequacy of the bony resection margins in patients undergoing segmental mandibulectomy.
2 METHODOLOGY
We obtained our institute's ethics committee approval to do this retrospective study. We included all oral cavity squamous cell carcinoma (OSCC) patients who underwent segmental mandibulectomy at our center from January 2012 to December 2021 for whom the intraoperative FS was utilized including postneoadjuvant chemotherapy (NACT) and recurrent disease/second primary patients. Benign histopathology and those other than squamous cell carcinoma were excluded. The primary objective of the study was to assess the usefulness of intraoperative FS assessment of BM to guide the adequacy of bone margins. The secondary objectives were to calculate the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of this assessment.
All patients underwent CT scans preoperatively, the findings of which were captured, especially regarding bone erosion. The relevant demographic and clinical details such as age, gender, comorbidities, ECOG status, history of prior treatment, clinical T-stage, and N-stage were captured. Treatment-related details such as details of the surgery, date of surgery, BM frozen if done from one end or both cut ends of the mandible, the positivity of malignancy in the frozen sample, and if the margin was revised and sent again for FS, the final bony margin and other margins were collected along with the pT and pN stage. We took our institute ethics committee's approval for the study to be performed.
2.1 Surgical procedure
The surgical extent was based on clinical and radiological findings. Intraoperatively 1 cm of soft tissue margins were taken and bone resection was performed 2 teeth away or 1–2 cm from suspected bony involvement.1 After resection the whole specimen was sent for FS analysis of the mucosal and soft tissue margins in most cases. The BM curettes were taken from the residual mandibular stump using a curette or a knife and sent for an FS (Figure 1). The BM FS was used in certain cases only and not in all cases. The need for it was based on the individual surgeon's assessment of preoperative imaging (contrast-enhanced CT scan), intraoperative findings and when the concerns of having positive bone margins were higher.
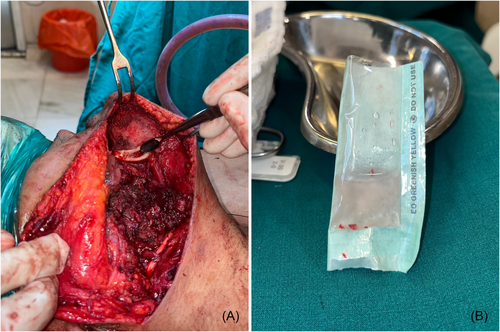
2.2 Histopathology techniques
In the FS room, BM curettes were smeared on glass slides, stained with hematoxylin-eosin (H&E) stain, mounted in histologic grade DPX (dibutyl phthalate xylene), cover-slipped, and examined using bright field microscopy for the presence of malignant epithelial cells. The smears were reported as “negative for tumor/bone margin free of tumor” or “positive for tumor/bone margin involved by tumor” depending on the absence/presence of any malignant epithelial cells on the smeared marrow respectively. (Figure 2) The time taken to process a single BM specimen for frozen is around 10 min and costs around INR (Indian Rupees) 250 in our institute.
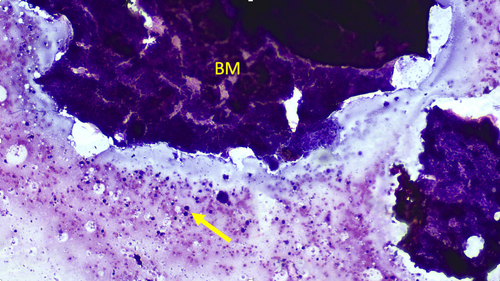
The final interpretation of bone margins was based on the pathologic interpretation of the decalcified mandibular specimens fixed in 10% neutral buffered formalin for 24 h. The bone margins from the fixed specimen were shaved and embedded en-face into section cassettes. The bone sections were decalcified further in 10% formal HNO3 (formaldehyde-nitric acid), with periodic checking for completion of decalcification. On adequate decalcification, the sections were washed in copious amounts of tap water for 4 h, followed by routine automated processing for paraffin embedding. Section (2–4 µm thick) were then taken on glass slides and stained with H&E stain, mounted in DPX, cover-slipped, and examined using bright field microscopy for the presence of malignant epithelial cells within the boundaries of bone. The presence of any tumor within the confines of the bone cortex or the marrow is interpreted as a “positive bone margin.”
2.3 Statistical analysis
The data analysis was conducted using IBM SPSS Statistics version 25 (IBM Corp). Descriptive statistics were calculated to summarize the key characteristics of the data. Sensitivity, specificity, PPV, and NPV were calculated to assess the diagnostic accuracy of the intraoperative FS of BM curettage. A χ2 test was performed to examine whether there were any factors associated with a positive intraoperative FS of BM curettage.
3 RESULTS
The total number of segmental mandibulectomy procedures performed between 2012 and 2021 was 8242. Out of the total number of patients who underwent segmental mandibulectomy, the number of cases in which the BM FS was utilized was 457 (5.5%). The type of mandibular defect following resections as per the classification by Brown et al.7 were as follows, class IIc defect in 74 patients, class Ic defect in 68 patients, and class I/II/IV defect in 315 patients.
The demographic and clinical characteristics of the study population are summarized in Table 1. The median age of the participants was 52 years (range: 22–80 years). The majority of patients were male (n = 368, 80.5%). All patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, except for two patients. Most of the patients treated were treatment naïve (n = 372, 81.4%). Only 95 patients (20.8%) had some form of associated comorbidities. Patients with T4 stage OSCC constituted the majority (n = 406, 88.8%) along with those with N+ disease (n = 294, 64.4%). Bone erosion on CT scans was present in 385 (84.2%) patients.
| Variables | Numbers (%) | p Value (For bone marrow frozen section positivity) |
|---|---|---|
| Age | Median: 52 years (Range: 22–80 years) | 0.273 |
| Gender | 0.771 | |
| Male | 368 (80.5) | |
| Female | 89 (19.5) | |
| Performance status (ECOG) | 0.654 | |
| 0 | 295 (64.6) | |
| 1 | 160 (35) | |
| 2 | 2 (0.4) | |
| Case type | 0.417 | |
| Per primam | 372 (81.4) | |
| Recurrent/second primary | 46 (10.1) | |
| Post NACT | 39 (8.5) | |
| Comorbidities | ||
| Present | 95 (20.8) | |
| Absent | 362 (79.2) | |
| cT-stage | 0.454 | |
| T1-T3 | 51 (11.2) | |
| T4 | 406 (88.8) | |
| cN-stage | 0.491 | |
| N0 | 163 (35.6) | |
| N+ | 294 (64.4) | |
| Bone erosion on CT scan | 0.448 | |
| Present | 385 (84.2) | |
| Absent | 72 (15.8) |
- Abbreviations: CT, computed tomography; ECOG, Eastern Cooperative Oncology Group; NACT, neoadjuvant chemotherapy.
BM was reported to be involved (positive) in the FS in only 18 patients (4%) for whom the bone margin was revised. Among these 18 patients, the final bone cut margin was positive in only 1 patient despite the bony revision. In nine patients the BM FS was reported negative, however in the final histopathology the cut margin was reported positive. The bone margins (cut end) were positive in the final histopathology in 10 patients (2.18%) and would have been positive in 21 patients (4.6%) if margins were not revised. We attempted to analyze the factors that could influence BM positivity to identify such patients when possible so that we can restrict this investigation (BM analysis on the FS) to such patients. However, we could not identify any such significant factors (Tables 1 & 2), which may be due to the small number of BM positivity rates on FS in our study. The sensitivity, specificity, PPV, and NPV were 52.3%, 98.65%, 64.7%, and 97.7% respectively (Table 3).
| Variables | Numbers (%) | p Value (For bone marrow frozen section positivity) |
|---|---|---|
| Bone marrow frozen section results | – | |
| Positive | 18 (3.9) | |
| Negative | 439 (96.1) | |
| Bone revision done (Based on frozen section) | – | |
| Yes | 19 (4.2) | |
| No | 438 (95.8) | |
| Bone marrow final report | – | |
| Positive | 12 (2.6) | |
| Negative | 445 (97.4) | |
| Bone margin status | – | |
| Positive | 10 (2.2) | |
| Negative | 447 (97.8) | |
| pT-stage | 0.93 | |
| T1 | 10 (2.2) | |
| T2 | 54 (11.8) | |
| T3 | 34 (7.4) | |
| T4 | 352 (7.7) | |
| pN-stage | 0.625 | |
| N0 | 254 (55.6) | |
| N+ | 203 (44.4) |
| Bone Final HPR (unrevised) | Total | |||
|---|---|---|---|---|
| Positive | Negative | |||
| Bone marrow frozen section | Positive | 11 | 6 | 17 |
| Negative | 10 | 430 | 440 | |
| Total | 21 | 436 | 457 | |
4 DISCUSSION
In our study, the intraoperative FS analysis of the BM was utilized in only 457 patients (5.5%). The marrow was positive in only 18 out of the 457 patients (3.9%). This investigation had a low sensitivity (52.3%) and PPV (64.7%), but a higher specificity (98.65%) and NPV (97.7%).
Achieving a tumor-free bone margin is an important aspect, the goal of which is to minimize the risk of tumor recurrence and thus improve patient outcomes. Presently there is no widely accepted consensus on the exact measurement that defines an ideal tumor-free bone margin. Clinical inspection, panoramic radiographs, and CT scans are commonly used methods/modalities to assess the extent of bone involvement/invasion by tumor. However, studies have shown that these methods may underestimate the true width of invasive disease by approximately 5 mm for clinical inspection, 13 mm for panoramic radiographs, and 5 mm for CT scans.8 This discrepancy in measurement highlights the importance of considering a sufficient safety bone margin around the tumor during surgical resection.
The recommended clinical bone margins vary from 0.5 to 1.0 cm, and most studies advocate for a 1 cm safety margin to ensure complete tumor removal and reduce the risk of local recurrence.9, 10 An attempt to perform revision of a positive margin can be challenging, particularly in cases where reconstruction has already been done leading to increased morbidity to the patients and a delay in starting adjuvant therapy. Thus, achieving an adequate tumor-free bone margin during the initial surgery is of paramount importance to avoid the need for reoperation and its associated morbidities.
A few studies have addressed the intraoperative histologic evaluation of bone margins. Histologic sampling of cortical bone during FS analysis is difficult due to dense mineralization. Direct comparison of these studies and techniques is limited by the methodologic differences, nature and pathology of the disease, type of surgical procedure performed, and location of the sampled bone margin.
Table 411-17 provides a summary of various studies that have investigated the use of different methods for BM FS analysis to predict the adequacy of resection. In the current study, utilizing the scalpel/curettage method for BM FS analysis, the sensitivity was 52.3%, and the specificity was 98.65%.
| Author/Year | No. of patients | Method of Bone marrow frozen section | Results |
|---|---|---|---|
| Forrest et al. (1995)11 | 16 | Curettage | FS could correctly predict adequacy of resection in 32 of the 33 margins (97%) |
| Forrest et al. (1997)12 | 30 | Curettage | FS could correctly predict adequacy of resection in 60 of the 61 margins |
| Mahamood et al. (2001)13 | 7 | Curettage | Complete concordance with FS. |
| Oxford et al. (2006)14 | 38 | Thin bony sections | Sensitivity of 89% and a specificity of 100% |
| Wysluch et al. (2010)10 | 20 | Trephine drill extraction | Sensitivity of 79% and specificity of 98%. |
| Bilodeau et al. (2011)15 | 27 | Curettage and IAN* | Sensitivity of 50% and specificity of 100%. |
| Nieberler et al. (2015)16 | 28 + 45 | Scalpel versus Scalpel + cytobrush | Sensitivity 95.3% and specificity 96% versus Sensitivity 80% and specificity 98.9% |
| Namin et al. (2015)9 | 51 | Curettage | 100% accuracy |
| Hegde et al. (2022)17 | 35 | Trephine drill | Sensitivity 81.8%, with a specificity of 87.5%, |
| Our study | 457 | Scalpel/curettage | Sensitivity 52.3%, specificity 98.65% |
The strength of our study is its large sample size and focus on a specific technique to prevent positive bony margins in oral cancer surgery. However, the retrospective design of the study and the lack of clear/uniform indications as to when the surgeon chose to get the BM FS analysis done could be considered its weakness. The possible opportunities that arise as a consequence of this study are that these results could be validated in a larger data set across multiple other centers. The only threat that we see is that despite the results showing the limited utility of this investigation it may be difficult to convince surgeons to not use this investigation based on the results that have emerged from the present study.
5 CONCLUSIONS
BM FS was utilized in a small percentage of patients undergoing segmental resections (5.5%). Further, when the BM FS was utilized in a selected few patients, it was positive in only a small percentage of this subset of patients (4%). BM FS was predominantly used for patients in the presence of bone erosion on CT-scan/T4 disease. The BM FS had a low sensitivity and PPV while it had a higher specificity and NPV. This investigation helped in reducing the bone margin positivity rate from 3.9% to 2.2% only. Hence we can conclude that the intraoperative BM FS assessment had limited utility as seen from our study.
ETHICS STATEMENT
Institutional ethics committee approval was taken for this study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
SYNOPSIS
The bone marrow from the cut ends of the mandible was sent for the frozen section in 457 OSCC patients, it was positive in only 18 patients (3.9%) for which revision was done. The bone marrow frozen section had a low sensitivity and positive predictive value, but it had a higher specificity and negative predictive value.