A 13-year-old with dual pancreatic rests
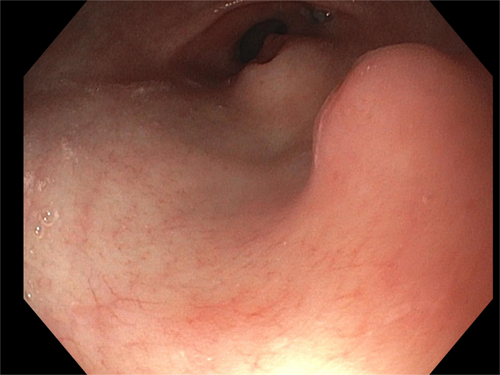
A 13-year-old male underwent an esophagogastroduodenoscopy (EGD) for chronic nausea, and reflux unresponsive to acid suppression. EGD revealed two separate submucosal nodular lesions measuring ~12–15 mm in the gastric antrum (Figure 1). Both lesions had a smooth surface. One with a center umbilication characteristic of pancreatic rest. The mucosal biopsies of the gastric nodules showed antral-type mucosa and minimal superficial gastritis.
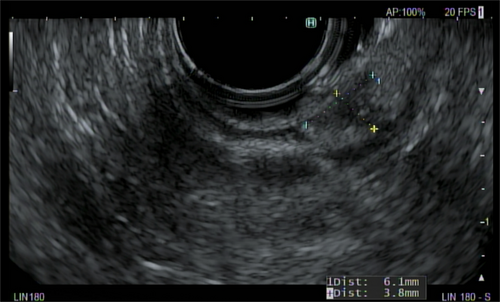
Endoscopic ultrasound (EUS) was performed for further evaluation of the second lesion.1 The EUS demonstrated a round intramural lesion in the antrum of the stomach (Figure 2). The lesion had internal ductal structures and sonographically the lesion appeared to originate from the submucosa. Measuring 7 mm, in maximal thickness, the outer borders were well-defined. The endoscopic and sonographic characteristics were most consistent with pancreatic rests and mucosal biopsies were normal which is suggestive enough for diagnosis of pancreatic rest.1
Heterotopic pancreas is a congenital anomaly in which the abnormal location of pancreatic tissue is anatomically separate from the main gland.2 The heterotopic tissue may cause symptoms related to its location, such as abdominal distension, gastric outlet obstruction, intussusception, umbilical discharge, or gastrointestinal bleeding from surrounding intestinal mucosa.2, 3 One multicenter retrospective analysis shows 25% of patients with pancreatic rest reporting associated symptoms, but the majority of those cases were Meckel's diverticulum with gastric mucosa heterotopia.3 Most commonly, it is not related to symptoms and is discovered incidentally, as was the situation for this patient. The patient was seen 2 months after diagnosis and symptoms had resolved without intervention.
The classical endoscopic appearance is a round, smooth, submucosal mass with central umbilication.4 Diagnosis is achieved through identifying these characteristics in EGD. If these are absent, EUS is useful for diagnosis, as was done for this patient.1 Other imaging modalities may result in incidental discovery and can aid in diagnosis but are not required for diagnosis. Computed tomography is the most common modality of incidental finding and, when able to identify multiple characteristics (i.e., duct-like structure, central umbilicus, and ratio of diameters), has a high specificity for pancreatic rest.5 Upper gastrointestinal contrast studies can identify a central lesion of the mass consistent with “central umbilical sign.” Imaging modalities can identify pancreatic rest but are not required for diagnostic purposes in the presence of classical findings on upper endoscopy. Diagnosis can be difficult to confirm due to being overlooked from low incidence and small size making identifying characteristics not visible on imaging. Missed diagnosis can result in surgical resection or biopsy before definitive diagnosis is achieved through histology.6
There have been reports of higher incidence of pancreatic rests in patients with esophageal atresia, although there does not appear to be other currently known associated congenital malformations.7 To our knowledge, this is the first report on the presence of two pancreatic rests and highlights the utility of EUS in the evaluation of gastrointestinal luminal submucosal lesions.
ACKNOWLEDGMENTS
The authors have nothing to report.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Written informed consent for the case report publication was obtained from the patient's parent before article submission.