Esophago-gastric junction findings on high resolution impedance manometry in children with esophageal atresia
Sharman P. Tan Tanny
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorNicholas D. Senior
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorAssia Comella
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Monash Medical School, Monash University, Clayton, Victoria, Australia
Search for more papers by this authorLisa McCall
Department of Human Physiology, Flinders University, Bedford Park, South Australia, Australia
Search for more papers by this authorJohn M. Hutson
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorSue Finch
Melbourne Statistical Consulting Platform, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorMark Safe
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
Search for more papers by this authorWarwick J. Teague
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorTaher I. Omari
Department of Human Physiology, Flinders University, Bedford Park, South Australia, Australia
Search for more papers by this authorCorresponding Author
Sebastian K. King
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Correspondence Sebastian K. King, Department of Paediatric Surgery, The Royal Children's Hospital, 50 Flemington Rd, Parkville, VIC 3052, Australia.
Email: [email protected]
Search for more papers by this authorSharman P. Tan Tanny
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorNicholas D. Senior
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorAssia Comella
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Monash Medical School, Monash University, Clayton, Victoria, Australia
Search for more papers by this authorLisa McCall
Department of Human Physiology, Flinders University, Bedford Park, South Australia, Australia
Search for more papers by this authorJohn M. Hutson
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorSue Finch
Melbourne Statistical Consulting Platform, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorMark Safe
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
Search for more papers by this authorWarwick J. Teague
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Search for more papers by this authorTaher I. Omari
Department of Human Physiology, Flinders University, Bedford Park, South Australia, Australia
Search for more papers by this authorCorresponding Author
Sebastian K. King
Department of Paediatric Surgery, The Royal Children's Hospital, Parkville, Victoria, Australia
F. Douglas Stephens Surgical Research Group, Murdoch Children's Research Institute, Parkville, Victoria, Australia
Department of Paediatrics, The University of Melbourne, Parkville, Victoria, Australia
Correspondence Sebastian K. King, Department of Paediatric Surgery, The Royal Children's Hospital, 50 Flemington Rd, Parkville, VIC 3052, Australia.
Email: [email protected]
Search for more papers by this authorAbstract
Objectives
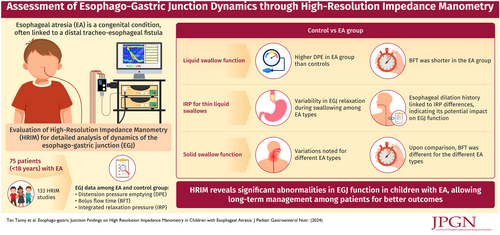
Using high resolution impedance manometry (HRIM), this study characterized the esophago-gastric junction (EGJ) dynamics in children with esophageal atresia (EA).
Method
Esophageal HRIM was performed in patients with EA aged less than 18 years. Objective motility patterns were analyzed, and EGJ data reported. Controls were pediatric patients without EA undergoing investigations for consideration of fundoplication surgery.
Results
Seventy-five patients (M:F = 43:32, median age 1 year 3 months [3 months–17 years 4 months]) completed 133 HRIM studies. The majority (64/75, 85.3%) had EA with distal tracheo-esophageal fistula. Compared with controls, liquid swallows were poorer in patients with EA, as evident by significant differences in distension pressure emptying and bolus flow time (BFT). The integrated relaxation pressure for thin liquid swallows was significantly different between EA types, as well as when comparing patients with EA with and without previous esophageal dilatations. The BFT for solid swallows was significantly different when compared with EA types.
Conclusions
We have utilized HRIM in patients with EA to demonstrate abnormalities in their long-term EGJ function. These abnormalities correlate with poorer esophageal compliance and reduced esophageal peristalsis across the EGJ. Understanding the EGJ function in patients with EA will allow us to tailor long-term management to specific patients.
Graphical Abstract
CONFLICT OF INTEREST STATEMENT
Professor Omari holds inventorship of the international patent family that covers the analytical methods described. The Swallow GatewayTM software service is owned and provided by Flinders University. The remaining authors declare no conflict of interest.
Supporting Information
| Filename | Description |
|---|---|
| jpn312213-sup-0001-Supplemental_content_1.docx18.5 KB | Supporting information. |
| jpn312213-sup-0002-Supplemental_content_2.docx16.6 KB | Supporting information. |
| jpn312213-sup-0003-Supplemental_content_3.docx16.6 KB | Supporting information. |
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
- 1Riley M, Halliday J. Birth defects in Victoria 2005-2006. Victorian Perinatal Data Collection Unit. Victoria Government Department of Human Services; 2008.
- 2Rintala RJ. Fundoplication in patients with esophageal atresia: patient selection, indications, and outcomes. Front Pediatr. 2017; 5: 109.
- 3Pellegrino SA, King SK, McLeod E, et al. Impact of esophageal atresia on the success of fundoplication for gastroesophageal reflux. J Pediatr. 2018; 198: 60-66.
- 4Rogers BD, Gyawali CP. Evaluation of the esophagogastric junction on high resolution manometry. J Clin Gastroenterol. 2021; 55(2): e8-e18.
- 5Bagucka B, Badriul H, Vandemaele K, et al. Normal ranges of continuous pH monitoring in the proximal esophagus. J Pediatr Gastroenterol Nutr. 2000; 31(3): 244-247.
- 6Goldani HAS, Staiano A, Borrelli O, Thapar N, Lindley KJ. Pediatric esophageal high-resolution manometry: utility of a standardized protocol and size-adjusted pressure topography parameters. Am J Gastroenterol. 2010; 105(2): 460-467.
- 7Staiano A, Boccia G, Miele E, Clouse RE. Segmental characteristics of oesophageal peristalsis in paediatric patients. Neurogastroenterol Motil. 2008; 20(1): 19-26.
- 8Dakkak M, Bennett JR. A new dysphagia score with objective validation. J Clin Gastroenterol. 1992; 14(2): 99-100.
- 9Singendonk MMJ, Ferris LF, McCall L, et al. High-resolution esophageal manometry in pediatrics: effect of esophageal length on diagnostic measures. Neurogastroenterol Motil. 2020; 32(1):e13721.
- 10Gross ER. The Surgery of Infancy and Chilhood. Saunders; 1962.
- 11Solomon BD. VACTERL/VATER association. Orphanet J Rare Dis. 2011; 6(1): 56.
- 12Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009; 42(2): 377-381.
- 13Ferris L, King S, McCall L, et al. Piecemeal deglutition and the implications for pressure impedance dysphagia assessment in pediatrics. J Pediatr Gastroenterol Nutr. 2018; 67(6): 713-719.
- 14Wang D, Xu H, Tang T, Wang J, Yu Y, Gyawali CP. Assessment of the esophagogastric junction (EGJ) using the EGJ contractile integral (EGJ-CI) following per-oral endoscopic myotomy (POEM) in achalasia. Rev Esp Enferm Dig. 2018; 110(11): 706-711.
- 15Cock C, Besanko LK, Burgstad CM, et al. Age-related impairment of esophagogastric junction relaxation and bolus flow time. World J Gastroenterol. 2017; 23(15): 2785-2794.
- 16Singendonk MMJ, Omari TI, Rommel N, et al. Novel pressure-impedance parameters for evaluating esophageal function in pediatric achalasia. J Pediatr Gastroenterol Nutr. 2018; 66(1): 37-42.
- 17Rayyan M, Omari T, Debeer A, et al. Characterization of esophageal motility in infants with congenital diaphragmatic hernia using high-resolution manometry. J Pediatr Gastroenterol Nutr. 2019; 69(1): 32-38.
- 18Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021; 33(1):e14058.
- 19Lin Z, Imam H, Nicodème F, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014; 307(2): G158-G163.
- 20Nicodème F, Pipa-Muniz M, Khanna K, Kahrilas PJ, Pandolfino JE. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014; 26(3): 353-360.
- 21Rogers BD, Rengarajan A, Abrahao L, et al. Esophagogastric junction morphology and contractile integral on high-resolution manometry in asymptomatic healthy volunteers: an international multicenter study. Neurogastroenterol Motil. 2021; 33(6):e14009.
- 22Kou W, Carlson DA, Kahrilas PJ, Patankar NA, Pandolfino JE. Normative values of intra-bolus pressure and esophageal compliance based on 4D high-resolution impedance manometry. Neurogastroenterol Motil. 2022; 34(10):e14423.
- 23Kawahara H, Kubota A, Hasegawa T, et al. Lack of distal esophageal contractions is a key determinant of gastroesophageal reflux disease after repair of esophageal atresia. J Pediatr Surg. 2007; 42(12): 2017-2021.
- 24Pedersen RN, Markøw S, Kruse-Andersen S, et al. Esophageal atresia: gastroesophageal functional follow-up in 5-15 year old children. J Pediatr Surg. 2013; 48(12): 2487-2495.
- 25Tambucci R, Thapar N, Saliakellis E, et al. Clinical relevance of esophageal baseline impedance measurement: just an innocent bystander. J Pediatr Gastroenterol Nutr. 2015; 60(6): 776-782.
- 26Tovar JA, Diez Pardo JA, Murcia J, Prieto G, Molina M, Polanco I. Ambulatory 24-hour manometric and pH metric evidence of permanent impairment of clearance capacity in patients with esophageal atresia. J Pediatr Surg. 1995; 30(8): 1224-1231.
- 27Lemoine C, Aspirot A, Le Henaff G, Piloquet H, Lévesque D, Faure C. Characterization of esophageal motility following esophageal atresia repair using high-resolution esophageal manometry. J Pediatr Gastroenterol Nutr. 2013; 56(6): 609-614.
- 28Rommel N, Omari TI, Selleslagh M, et al. High-resolution manometry combined with impedance measurements discriminates the cause of dysphagia in children. Eur J Pediatr. 2015; 174(12): 1629-1637.
- 29Courbette O, Omari T, Aspirot A, Faure C. Characterization of esophageal motility in children with operated esophageal atresia using high-resolution impedance manometry and pressure flow analysis. J Pediatr Gastroenterol Nutr. 2020; 71(3): 304-309.
- 30Tovar J, Fragoso A. Gastroesophageal reflux after repair of esophageal atresia. Eur J Pediatr Surg. 2013; 23(3): 175-181.
- 31Lin Z, Carlson DA, Dykstra K, et al. High-resolution impedance manometry measurement of bolus flow time in achalasia and its correlation with dysphagia. Neurogastroenterol Motil. 2015; 27(9): 1232-1238.
- 32Rommel N, Rayyan M, Scheerens C, Omari T. The potential benefits of applying recent advances in esophageal motility testing in patients with esophageal atresia. Front Pediatr. 2017; 5: 137.