Proton pump inhibitors, antibiotics, and atopy increase the risk of eosinophilic esophagitis in children with esophageal atresia
Tiffany C. Tang
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Search for more papers by this authorSteven T. Leach
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Search for more papers by this authorCorresponding Author
Usha Krishnan
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Department of Pediatric Gastroenterology, Sydney Children's Hospital Randwick, Sydney, Australia
Correspondence Usha Krishnan, Department of Pediatric Gastroenterology, Sydney Children's Hospital Randwick, High St, Randwick, NSW 2031, Australia.
Email: [email protected]
Search for more papers by this authorTiffany C. Tang
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Search for more papers by this authorSteven T. Leach
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Search for more papers by this authorCorresponding Author
Usha Krishnan
School of Clinical Medicine, Discipline of Pediatrics, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Department of Pediatric Gastroenterology, Sydney Children's Hospital Randwick, Sydney, Australia
Correspondence Usha Krishnan, Department of Pediatric Gastroenterology, Sydney Children's Hospital Randwick, High St, Randwick, NSW 2031, Australia.
Email: [email protected]
Search for more papers by this authorAbstract
Objective
To determine whether proton pump inhibitor (PPI) exposure is associated with an increased risk of developing eosinophilic esophagitis (EoE) in children with esophageal atresia (EA).
Study Design
A retrospective chart review of children with EA from January 1, 2005 to December 31, 2020 was undertaken at Sydney Children's Hospital Randwick. Children with EA and EoE (cases) were matched (1:2) to children with only EA (controls) to compare PPI exposure. Other early-life factors such as infantile antibiotic exposure and personal or family history of atopy were also analyzed using simple and multivariable logistic regression.
Results
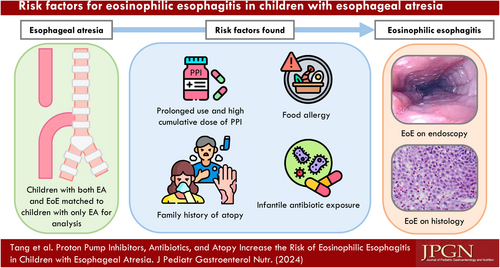
Of 184 children with EA, 46 (25%) developed EoE during this period. Thirty-eight EoE participants were matched to 76 controls. Children with EoE and EA received PPI for significantly higher durations (p = .018) and at significantly higher cumulative doses (p = .017) than controls. Food allergy (adjusted odds ratio [aOR], 7.317; 95% confidence interval [CI], 2.244–23.742), family history of atopy (aOR, 3.504; 95% CI, 1.268–9.682), and infantile antibiotic exposure (aOR, 1.040; 95% CI, 1.006–1.075) were also significantly associated with an increased risk of developing EoE in the EA cohort.
Conclusions
Prolonged duration and high cumulative dose of PPI exposure were significantly associated with subsequent EoE development in children with EA. Food allergy, family history of atopy, and infantile antibiotic exposure in EA were also significantly associated with an increased risk of EoE development.
Graphical Abstract
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES
- 1Stoll C, Alembik Y, Dott B, Roth MP. Associated anomalies in cases with esophageal atresia. Am J Med Genet, Part A. 2017; 173(8): 2139-2157.
- 2Stadil T, Koivusalo A, Pakarinen M, et al. Surgical repair of long-gap esophageal atresia: a retrospective study comparing the management of long-gap esophageal atresia in the Nordic countries. J Pediatr Surg. 2019; 54(3): 423-428.
- 3Krishnan U, Mousa H, Dall'Oglio L, et al. ESPGHAN-NASPGHAN guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with esophageal atresia-tracheoesophageal fistula. J Pediatr Gastroenterol Nutr. 2016; 63(5): 550-570.
- 4van Lennep M, Singendonk MMJ, Dall'Oglio L, et al. Oesophageal atresia. Nat Rev Dis Primers. 2019; 5(1): 26.
- 5Alexander ES, Martin LJ, Collins MH, et al. Twin and family studies reveal strong environmental and weaker genetic cues explaining heritability of eosinophilic esophagitis. J Allergy Clin Immunol. 2014; 134(5): 1084-1092.
- 6Limketkai BN, Shah SC, Hirano I, Bellaguarda E, Colombel JF. Epidemiology and implications of concurrent diagnosis of eosinophilic oesophagitis and IBD based on a prospective population-based analysis. Gut. 2019; 68(12): 2152-2160.
- 7Aceves SS, Newbury RO, Dohil R, Bastian JF, Broide DH. Esophageal remodeling in pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2007; 119(1): 206-212.
- 8Dellon ES, Liacouras CA, Molina-Infante J, et al. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE conference. Gastroenterology. 2018; 155(4): 1022-1033.
- 9Krishnan U, Lijuan C, Andrew GJ, Rothenberg ME, Wen T. Analysis of eosinophilic esophagitis in children with repaired congenital esophageal atresia. J Allergy Clin Immunol. 2019; 143(4): 1455-1464.
- 10Mansoor E, Cooper GS. The 2010-2015 prevalence of eosinophilic esophagitis in the USA: a population-based study. Dig Dis Sci. 2016; 61(10): 2928-2934.
- 11Kottyan LC, Davis BP, Sherrill JD, et al. Genome-wide association analysis of eosinophilic esophagitis provides insight into the tissue specificity of this allergic disease. Nature Genet. 2014; 46(8): 895-900.
- 12Jensen ET, Kappelman MD, Kim HP, Ringel-Kulka T, Dellon ES. Early life exposures as risk factors for pediatric eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2013; 57(1): 67-71.
- 13Gómez Torrijos E, Sánchez Miranda P, Donado Palencia P, et al. Eosinophilic esophagitis: demographic, clinical, endoscopic, histologic, and atopic characteristics of children and teenagers in a region in central Spain. J Investig Allergol Clin Immunol. 2017; 27(2): 104-110.
- 14Dellon ES, Jensen ET, Martin CF, Shaheen NJ, Kappelman MD. Prevalence of eosinophilic esophagitis in the United States. Clin Gastroenterol Hepatol. 2014; 12(4): 589-596.
- 15Dhaliwal J, Tobias V, Sugo E, et al. Eosinophilic esophagitis in children with esophageal atresia. Dis Esophagus. 2014; 27(4): 340-347.
- 16Frazzoni M, Penagini R, Frazzoni L, et al. Role of reflux in the pathogenesis of eosinophilic esophagitis: comprehensive appraisal with off-and on PPI impedance-pH monitoring. Am J Gastroenterol. 2019; 114(10): 1606-1613.
- 17Lardenois E, Michaud L, Schneider A, et al. Prevalence of eosinophilic esophagitis in adolescents with esophageal atresia. J Pediatr Gastroenterol Nutr. 2019; 69(1): 52-56.
- 18Olszak T, An D, Zeissig S, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science. 2012; 336(6080): 489-493.
- 19Carr D, Barnes EH, Gordon A, Isaacs D. Effect of antibiotic use on antimicrobial antibiotic resistance and late-onset neonatal infections over 25 years in an Australian tertiary neonatal unit. Arch Dis Child Fetal Neonatal Ed. 2017; 102(3): F244-F250.
- 20Sherrill JD, Gao P-S, Stucke EM, et al. Variants of thymic stromal lymphopoietin and its receptor associate with eosinophilic esophagitis. J Allergy Clin Immunol. 2010; 126(1): 160-165.
- 21Jensen ET, Kuhl JT, Martin L, Rothenberg ME, Dellon E. 664 Prenatal, antenatal, and early life factors are associated with risk of eosinophilic esophagitis. Gastroenterology. 2016; 150(4): S135-S136.
10.1016/S0016-5085(16)30555-8 Google Scholar
- 22Flatrès C, Aumar M, Ley D, et al. Prevalence of acid gastroesophageal reflux disease in infants with esophageal atresia/tracheoesophageal fistula. Pediatr Res. 2022; 91(4): 977-983.
- 23Witmer CP, Susi A, Min SB, Nylund CM. Early infant risk factors for pediatric eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2018; 67(5): 610-615.
- 24Jensen ET, Kuhl JT, Martin LJ, Rothenberg ME, Dellon ES. Prenatal, intrapartum, and postnatal factors are associated with pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2018; 141(1): 214-222.
- 25Kuhn BR, Young AJ, Justice AE, Chittoor G, Walton NA. Infant acid suppression use is associated with the development of eosinophilic esophagitis. Dis Esophagus. 2020; 33(10):doaa073.
- 26Radano MC, Yuan Q, Katz A, et al. Cesarean section and antibiotic use found to be associated with eosinophilic esophagitis. J Allergy Clin Immunol Pract. 2014; 2(4): 475-477.
- 27Mitre E, Susi A, Kropp LE, Schwartz DJ, Gorman GH, Nylund CM. Association between use of acid-suppressive medications and antibiotics during infancy and allergic diseases in early childhood. JAMA Pediatr. 2018; 172(6):e180315-e.
- 28Orel R, Murch S, Amil Dias J, Vandenplas Y, Homan M. Eosinophilic esophagitis that develops during therapy with proton pump inhibitors: case series and possible mechanisms. Acta Gastro-Enterol Belg. 2016; 79(2): 245-250.
- 29Brusselaers N, Pereira M, Alm J, Engstrand L, Engstrand Lilja H. Effect of proton pump inhibitors in infants with esophageal atresia on the gut microbiome: a pilot cohort. Gut Pathog. 2022; 14(1): 47.
- 30Chen CC, Chen KJ, Kong MS, Chang HJ, Huang JL. Alterations in the gut microbiotas of children with food sensitization in early life. Pediatr Allergy Immunol. 2016; 27(3): 254-262.
- 31Fujimura KE, Sitarik AR, Havstad S, et al. Neonatal gut microbiota associates with childhood multisensitized atopy and T cell differentiation. Nature Med. 2016; 22(10): 1187-1191.
- 32Jackson MA, Goodrich JK, Maxan M-E, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016; 65(5): 749-756.
- 33Righini Grunder F, Petit L-M, Ezri J, et al. Should proton pump inhibitors be systematically prescribed in patients with esophageal atresia after surgical repair? J Pediatr Gastroenterol Nutr. 2019; 69(1): 45-51.
- 34Miyake H, Chen Y, Hock A, Seo S, Koike Y, Pierro A. Are prophylactic anti-reflux medications effective after esophageal atresia repair? Systematic review and meta-analysis. Pediatr Surg Int. 2018; 34(5): 491-497.
- 35Bowder AN, Bence CM, Rymeski BA, et al. Acid suppression duration does not alter anastomotic stricture rates after esophageal atresia with distal tracheoesophageal fistula repair: a prospective multi-institutional cohort study. J Pediatr Surg. 2022; 57: 975-980.
- 36van Lennep M, Gottrand F, Faure C, et al. Management of gastroesophageal reflux disease in esophageal atresia patients: a cross-sectional survey amongst international clinicians. J Pediatr Gastroenterol Nutr. 2022; 75(2): 145-150.
- 37O'Donnell JEM, Purcell M, Mousa H, et al. Clinician knowledge of societal guidelines on management of gastrointestinal complications in Esophageal Atresia. J Pediatr Gastroenterol Nutr. 2021; 72(2): 232-238.
- 38Yasuda JL, Clark SJ, Staffa SJ, et al. Esophagitis in pediatric esophageal atresia: acid may not always be the issue. J Pediatr Gastroenterol Nutr. 2019; 69(2): 163-170.
- 39Capucilli P, Cianferoni A, Grundmeier RW, Spergel JM. Comparison of comorbid diagnoses in children with and without eosinophilic esophagitis in a large population. Ann Allergy Asthma Immunol. 2018; 121(6): 711-716.
- 40Arias Á, González-Cervera J, Tenias JM, Lucendo AJ. Efficacy of dietary interventions for inducing histologic remission in patients with eosinophilic esophagitis: a systematic review and meta-analysis. Gastroenterology. 2014; 146(7): 1639-1648.
- 41Henderson CJ, Abonia JP, King EC, et al. Comparative dietary therapy effectiveness in remission of pediatric eosinophilic esophagitis. J Allergy Clin Immunol. 2012; 129(6): 1570-1578.
- 42Hoofien A, Dias JA, Malamisura M, et al. Pediatric eosinophilic esophagitis: results of the European retrospective pediatric eosinophilic esophagitis registry (RetroPEER). J Pediatr Gastroenterol Nutr. 2019; 68(4): 552-558.
- 43Crnković HT, Bendelja K, Šimić Klarić A, Tomić Rajić M, Drkulec V, Aberle N. Family history and cord blood eosinophil count as predictors for atopic manifestations. Cent Eur J Public Health. 2019; 27(4): 267-271.
- 44Rothenberg ME, Spergel JM, Sherrill JD, et al. Common variants at 5q22 associate with pediatric eosinophilic esophagitis. Nature Genet. 2010; 42(4): 289-291.
- 45Sleiman PMA, Wang ML, Cianferoni A, et al. GWAS identifies four novel eosinophilic esophagitis loci. Nat Commun. 2014; 5: 5593.
- 46Davis BP, Stucke EM, Khorki ME, et al. Eosinophilic esophagitis-linked calpain 14 is an IL-13-induced protease that mediates esophageal epithelial barrier impairment. JCI Insight. 2016; 1(4):e86355-e.
- 47Zwittink RD, Renes IB, van Lingen RA, et al. Association between duration of intravenous antibiotic administration and early-life microbiota development in late-preterm infants. Eur J Clin Microbiol Infect Dis. 2018; 37(3): 475-483.
- 48Holvoet S, Doucet-Ladevèze R, Perrot M, Barretto C, Nutten S, Blanchard C. Beneficial effect of Lactococcus lactis NCC 2287 in a murine model of eosinophilic esophagitis. Allergy. 2016; 71(12): 1753-1761.
- 49Brusilovsky M, Bao R, Rochman M, Kemter AM, Nagler CR, Rothenberg ME. Host-microbiota interactions in the esophagus during homeostasis and allergic inflammation. Gastroenterology. 2022; 162(2): 521-534.
- 50Batres LA, Liacouras C, Schnaufer L, Mascarenhas MR. Eosinophilic esophagitis associated with anastomotic strictures after esophageal atresia repair. J Pediatr Gastroenterol Nutr. 2002; 35(2): 224-226.