Irregular types of proximal tibiofibular joint increase the risk of total knee replacement: Data from the osteoarthritis initiative
Yi Zhao and Zhaohua Zhu contributed equally to this study.
Abstract
The study aimed to determine the associations between the morphological types of proximal tibiofibular joint (PTFJ) and the risk of total knee replacement (TKR) in a cohort of participants with progressive osteoarthritis. A nested case–control design was performed in Osteoarthritis Initiative study. The case knees were those with TKR at 24–60 months follow up (cases), and were 1:1 matched with control knees by age, sex, and Kellgren-Lawrence grade at baseline. The morphological type of each PTFJ was identified according to the coronal and sagittal MR images. Conditional logistic regression models were used to examine the association of the PTFJ types with the risk of TKR at baseline and the time point before TKR (T0). A total of 193 case knees at baseline and 148 case knees at T0 time point had matched controls between 12 and 60 M. Seven types of the PTFJ were identified and classified into three categories: plane, trochoid, and irregular types. The prevalence of the irregular type was higher in case knees than in controls both at baseline (cases vs. controls, 35.8% vs. 26.9%) and at T0 time point (cases vs. controls, 33.1% vs. 27.0%). The irregular type of the PTFJ at baseline (odds ratio: 1.62, 95% confidence interval: 1.01–2.59) rather than at T0 time point was significantly associated with increased odds of TKR. The irregular types of the PTFJ at baseline are associated with increased risk of TKR, suggesting PTFJ may play a role in knee osteoarthritis.
1 INTRODUCTION
Knee osteoarthritis (OA) is one of the most prevalent diseases that affects over 10% of the population.1 Due to the absence of approved disease-modifying therapy, total knee replacement (TKR) is considered to be relatively effective management for end-stage knee OA.2 However, there is no clear consensus on medical indications for TKR. A lot of factors such as severe pain, functional limitation, reduction in quality of life and relevant healthcare expenditure may influence the patients' decision-making for TKR.3 In addition to the above factors, researchers are also seeking for imaging biomarkers that are significantly related to the outcome of knee OA. Recently, using magnetic resonance imaging (MRI), cartilage volume or thickness loss, bone marrow lesions, subchondral bone cysts had been reported to be associated with the increase of TKR,4-6 suggesting these structural changes of the knee joint may be useful for predicting TKR risk.
The proximal tibiofibular joint (PTFJ) is a synovial joint located between lateral tibial condyle and fibular head, which has been regarded as the “fourth compartment” of knee joint because of its anatomical communication with the tibiofemoral joint (TFJ) in 10%–63% of people.7, 8 This communication is clinically important because either joint compartment may be affected when joint pressure is elevated.8 Previous studies have showed that the PTFJ cannot only develop primary OA itself,9 but also be involved in the development of knee OA.10 Moreover, the severity of PTFJ OA correlated strongly with the severity of TFJ OA.11 Özcan et al.12 reported that inflammatory factors passing through anatomical communication between PTFJ and TFJ might contribute to the development of OA in both joints. By studying the human cadaveric knee specimens, Scott et al suggested the geometry of PTFJ could affect the knee varus-valgus loading and the motion for PTFJ and be related to the development of knee OA.13 Additionally, the PTFJ could also be an anatomical source of lateral knee pain,14 especially after TKRs.15 Therefore, more attention should be paid regarding the role of the PTFJ in the development of knee OA.
From the view of anatomy, PTFJ can be classified into different types. Barnett and Napier first described three types of PTFJ (Type I, II, III) according to the shape and inclination of joints.16 Ogden simply classified PTFJ into two types: “horizontal” and “oblique,” depending on the obliquity of the joint surface to the horizontal plane.7 Thereafter, Eichenblat and Nathan developed a classification system from their study of the fibula, tibia, and PTFJ in 489 dry bones, 50 cadaveric knees, and 1 clinical case. The joint was classified into seven types: plane, trochoid, double trochoid, condylar, saddle, trochlear, and ball & socket.17 Recently, we described an association between the morphology of PTFJ and an increased risk of incident radiographic OA and suggested that the MRI morphology of PTFJ could be a useful imaging biomarker for the prediction of progression and prognosis of knee OA.18, 19 Furthermore, we reported that a larger load-bearing area of PTFJ was associated with increased structural changes in medial tibiofemoral compartment in knee OA patients.18 Given that TKR is a common outcome of progressive knee OA and is used as an endpoint of knee OA research frequently, investigating the predictive value of PTFJ types could provide novel prognostic biomarkers for TKR. Therefore, we conducted the present nested case–control study aiming to determine whether the types of the PTFJ are associated with an increased risk of TKR over 5 years of follow-up in the Osteoarthritis Initiative (OAI) study.
2 METHODS
2.1 Study design and participants
Data used for this nested case–control study were obtained from the OAI study, which is an ongoing multi-center longitudinal cohort study of knee OA including 4796 participants aged from 45 to 79 years old from four clinical sites in the United States (http://www.oai.ucsf.edu/). MRI scans were performed for all participants annually between baseline, 1, 2, 3, 4, and 5 years follow-up.20, 21 All participants were examined and interviewed annually about having received a knee replacement in the preceding 12 months, which should be confirmed by radiography, or from hospital records when radiographs were not available. The OAI study was approved by the institutional review boards at each of the sites, and all participants gave informed consents.
For the current study, a case was identified as one who had a record of TKR at 12 months (M), 24, 36, 48, or 60 M follow-up, and MRI acquisitions acceptable for typing analysis had to be available at baseline for baseline analyses or at T0 time point for pre-TKR analyses (the annual MRI examination before TKR occurrence was termed as T0). We only included knees that first underwent TKR among participants who received bilateral TKR. Control knees were selected from those without self-reported TKR and without evidence of TKR on radiographs between baseline and 60 M. Knees would not be identified as controls if the opposite knee received a TKR during the study. Controls also had to have MRIs available at time points of baseline or T0 corresponding to those of the TKR cases. Cases and controls were matched 1:1 by sex, age (±5 years), and radiographic disease stage, documented by central reading at the baseline visit (Kellgren-Lawrence grade strata of 0–1, 2, 3, and 4).20, 22 Additionally, knee injury and surgery history were ascertained by self-report at the enrollment visit (OAI study protocol). Knee injury was defined as a history of injury, causing difficulty walking for at least a week, and surgery was defined as a history of any knee surgery such as meniscal and ligamentous repairs.
2.2 MRI assessment of PTFJ types
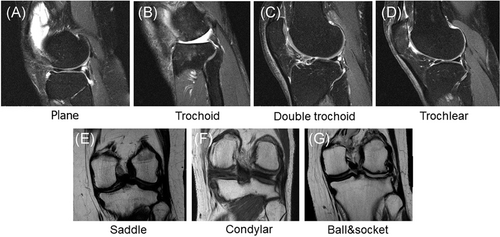
MRI sequences collected in the OAI were described in detail by Peterfy and colleagues and had been available for our previous study.21, 23 For identifying the types of the PTFJ, a coronal intermediate weighted two-dimensional (2D) fast spin-echo sequence and a sagittal intermediate weighted 2D fast spin-echo sequence of knee joint were applied. In accordance with Eichenbalt and Nathan's anatomical classification, we identified seven types of PTFJ according to the MR images using the published method in our previous study.24 Sagittal images were firstly used to identify the plane, trochoid, double trochoid, and trochlear joint types. Coronal images were used for assessment of condylar, saddle, and ball & socket joint types. PTFJ typing measures were repeated by one reader (3 months later) or scored by two readers independently in 50 randomly selected participants to calculate intra-reader and inter-reader reliabilities. The intraclass correlation coefficient (ICC) was 0.90 and the inter-reader reliability was 0.85.
2.3 Statistical analysis
All statistical analyses were performed on Stata V13.0 (Stata Corp.). The type of the PTFJ at baseline was considered as the exposure because it had been described that irregular PTFJ shapes are associated with osteoarthritic changes in the lateral compartment in older adults.20 The PTFJ type at T0 time point was assessed as an exposure, as the PTFJ type before TKR might also contribute to the risk of TKR. Demographic characteristics at baseline were assessed using descriptive statistics (frequencies and mean/standard deviation [SD] values). Group differences between cases and controls were tested by t test, χ2 tests, and Fisher's Exact tests as appropriate for the data type and distribution. Conditional logistic regression models for case–control matched data were developed to examine the association of the PTFJ types with the risk of TKR. Robustness of the results was assessed by performing additional adjustment for the effects of BMI (normal, overweight, obese), self-reported knee injury, and self-reported knee surgery at baseline. 95% confidence interval (CI) not including 1 or p < 0.05 was considered statistically significant.
3 RESULTS
3.1 Sample description
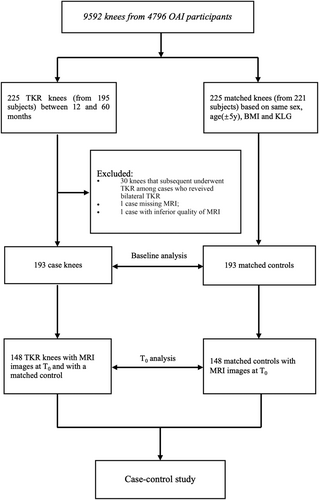
Two hundred and twenty-three knees of 193 participants received a TKR between 12 and 60 M (25 at 12 M, 37 at 24 M, 55 at 36 M, 43 at 48 M, and 63 at 60 M). All case knees and their matched controls had available MRI readings at baseline. A total of 193 case knees at baseline and 148 case knees at T0 time point had matched controls. They were included in our present study (Figure 1). Characteristics of the cases and controls are summarized in Table 1. The age, sex, and KL grades were matched between case and control knees. Moreover, there were no significant differences in the BMI, history of injury, and history of surgery between these two groups.
| Per person | |||
|---|---|---|---|
| Variables | Cases (n = 193) | Controls (n = 193) | p value |
Age, years ( ± SD) ± SD) |
64.6 ± 8.4 | 64.4 ± 8.4 | 0.767 |
| Female, n (%) | 112 (58.0) | 112 (58.0) | 1.000 |
BMI, kg/m2 ( ± SD) ± SD) |
29.6 ± 4.7 | 29.3 ± 4.6 | 0.629 |
| History of injury, n (%) | 86 (45.0) | 82 (42.5) | 0.616 |
| History of surgery, n (%) | 74 (38.3) | 58 (30.2) | 0.093 |
| Family history of TKR, n (%) | 35 (18.2) | 23 (12.0) | 0.091 |
| Per knee | |||
|---|---|---|---|
| Variables | Case knees (n = 193) | Control knees (n = 193) | p value |
| KL grades, n (%) | 0.976 | ||
| 0 | 8 (4.2) | 10 (5.2) | |
| 1 | 9 (4.7) | 7 (3.6) | |
| 2 | 30 (15.5) | 30 (15.5) | |
| 3 | 69 (35.8) | 69 (35.8) | |
| 4 | 77 (39.9) | 77 (39,9) | |
3.2 PTFJ types in cases and controls
Corresponding to the anatomic classification, the PTFJ could be classified into seven types on MR images. They were referred to as plane, trochoid, double trochoid, saddle, condylar, trochlear, and ball & socket type, respectively (Figure 2). The prevalence of different types in case knees and matched controls at baseline and T0 time point is described in Table S1. The distribution of seven PTFJ types were largely unchanged between baseline and T0 time point in both case and control groups. Plane and trochoid types were the most common types in both case knees (64.2% at baseline and 66.9% at T0) and controls (73.1% at baseline and 73.0% at T0). They also had relatively regular shapes on MR images. Other five types presented with less regular shapes than plane or trochoid type and accounted for small percentages in all types. These five uncommon types were collapsed into a single category (irregular) for further analyses. Compared with control groups, the prevalence of plane and trochoid types in case groups was not different statistically at the baseline or T0 time point (both p > 0.1). The prevalence of irregular types was higher in case knees than in controls at baseline, however, no statistical difference was reached (35.8% vs. 26.9%, p = 0.079). Although the prevalence of irregular types was higher in case knees than in controls, there was no statistical difference between case and control group at T0 time point (33.1% vs. 27.0%, p = 0.311).
3.3 Associations of PTFJ types with TKR risk
The plain type of PTFJ was used as the comparator when assessing the association of PTFJ types with TKR risks. Compared to the control knees, the irregular type of PTFJ was more common in case knees at both baseline and T0 time point. In conditional logistic regression analyses, the irregular type of PTFJ was significantly associated with the increase of TKR risk at baseline even though after adjustment for BMI, self-reported knee injury, and self-reported knee surgery (p = 0.043). However, no significant association was observed at T0 time point (p = 0.248) (Table 2).
| Types | Baseline (n = 193 paired knees) | T0 time point (n = 148 paired knees) | ||||
|---|---|---|---|---|---|---|
| Case n (%) | Control n (%) | CCa OR (95% CI) | TKR n (%) | Control n (%) | CCa OR (95% CI) | |
| Plain, n (%) | 83 (43.0) | 98 (50.8) | Reference group | 73 (49.3) | 78 (52.7) | Reference group |
| Trochoid, n (%) | 41 (21.2) | 43 (22.3) | 1.12 (0.66–1.90) | 26 (17.6) | 30 (20.3) | 0.96 (0.50–1.81) |
| Irregular, n (%) | 69 (35.8) | 52 (26.9) | 1.62 (1.01–2.59) | 49 (33.1) | 40 (27.0) | 1.37 (0.80–2.35) |
- Note: CCa, case–control conditional logistic regression adjusted for BMI category, self-reported knee injury, self-reported knee surgery. Significant result is shown in bold.
- Abbreviations: CI, confidence interval; OR, odds ratio; PTFJ, proximal tibiofibular joint; TKR, total knee replacement.
4 DISCUSSION
To our knowledge, this is the first study to describe the association of the PTFJ types with the risk of TKR. We found that irregular types of PTFJ were related to an increased risk of TKR.
The morphology of the PTFJ varies among different individuals. Several classifications of PTFJ shape have been developed according to anatomical and radiological studies.7, 17, 25 The previous study suggested that oblique-type PTFJ was more prone to degenerative changes because the oblique joint surface area was smaller, associated with less rotatory mobility and increased pressure on cartilage per mm2.7, 10, 25 Moreover, the strong association between the arthritic degeneration in PTFJ and the OA severity of tibiofemoral joint was observed in Boya's study, although the relationship between PTFJ types and degree of arthritis was not confirmed because of sample size limitation.11 But the above-mentioned method was quite a broad classification method using plane X-ray imaging, which is known to be relatively insensitive to structural changes, comparing to MRI. Similarly, Eichenblat and Nathan found a statistically significant correlation in their specimens between OA presence of the PTFJ and knee OA, particularly affecting the medial compartment. However, they did not find the correlation between the types and angles of inclination of the PTFJ and OA in the same affected joint, even though they classified the shape of PTFJ into seven anatomical types.17 Actually, whether PTFJ OA is related to the types of PTFJ and whether degeneration of PTFJ involves in the development of knee OA are still unknown.
Using MRI scans, we have first described the association of PTFJ types with knee osteoarthritic changes based on the morphology of PTFJ on MRI, and found that irregular PTFJ types were associated with osteoarthritic changes in lateral tibiofemoral compartment in older patients.24 As TKR is a common outcome of progressive knee OA, the contribution of irregular PTFJ types to knee OA may increase the risk of TKR. The mechanism underling these findings are still unclear, but the present study identified novel biomarkers that could be used for knee OA prognosis. Therefore, using knee joint MRIs to assess the PTFJ types could be a feasible method for clinicians to predict the risk of TKR in the future.
According to our previous study, the plane and trochoid types of PTFJ were considered as regular types because of their relative regular shape. The other five types of PTFJ had not only irregular shape but also had low prevalence compared to the plane and trochoid types. They were collapsed into one single category (irregular type). In this nested case–control study, we found that the irregular type of PTFJ at baseline was correlated to an increased TKR risk. It was consistent with our previous result that the irregular PTFJ joint types were associated with lateral osteoarthritic changes in older patients.24 Notably, according to the study of Espregueira-Mendes, the oblique type seemed to be more frequent in the relatively irregular types.25 Moreover, the oblique type of PTFJ is associated with less rotatory mobility and less joint surface area as compared with the horizontal type. This anatomical feature results in increased pressure on cartilage per mm2 and increases the risk of dislocation or degeneration of PTFJ.7, 25 Specifically, the proportions of Ball & Socket type of PTFJ were significantly different between cases and controls, albeit relatively small number. This was in line with our previous cross-sectional study which found that the Ball & Socket type of PTFJ was consistently associated with reduced cartilage volume and increased structural abnormalities. Therefore, the irregular and oblique type of PTFJ may be prone to arthritic degeneration, contributing to the development of tibiofemoral joint OA, and consequently to the increased risks of TKR. In contrast, we did not confirm the statistical correlation at T0 time point though there was the same trend in the case knees. Power calculation showed that 173 knees cannot meet the statistical power of 80% threshold, suggesting the reduction of paired knees might weaken the differences between cases and controls.
The nested case–control study derived from the OAI study provided the strength for our present study, which could reduce confounding factors as much as possible. There are also several potential limitations in this study. First, the prevalence of PTFJ types may be influenced by ethnicity. The OAI is predominantly a Northern American Caucasian cohort study which means it inevitably has the limitations in differences of ethnicity, geographical distribution, and regional culture. Second, many variables influenced both the timing and the decision to perform TKR. Some factors such as surgical indication depending on willingness, comorbidity, access to health care, socioeconomic status, may impact on our results. Third, as with any observational study, it is impossible to rule out residual bias from unknown or unmeasured confounders. Last, there might have isolated individuals in the control group who were scheduled TKR but had not yet received it. However, we have also analyzed T0 time point which is before TKR, suggesting the impact of this issue is minimal.
In conclusion, irregular types of PTFJ are associated with an increased risk of TKR, suggesting PTFJ may play a role in the progression of knee OA. The biomechanical and functional mechanisms of PTFJ involving in knee OA need to be investigated in future studies.
ACKNOWLEDGMENTS
Special thanks go to the participants who made this study possible, the OAI and POMA investigators, staff and participants. This study and image acquisition were funded by the OAI study and POMA study. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) lead this initiative at the National Institutes of Health (NIH). Private funding partners included GlaxoSmithKline, Merck & Co., Inc., Novartis Pharmaceuticals Corporation, and Pfizer. Private-sector funding for the OAI is being managed by the Foundation for the National Institutes of Health. The POMA study was funded by the NIH's National Heart, Lung, and Blood Institute.
CONFLICT OF INTERESTS
DJH provides consulting advice on advisory boards for Merck Serono, TLC Bio, Lilly, and Pfizer outside of the submitted work. CKK provides consulting advice on advisory boards for Merck Serono, Fidia, Astellas, and Thusane outside of the submitted work. Other authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
Yi Zhao, Zhaohua Zhu, Jun Chang, and Changhai Ding conceived and designed the study, drafted the manuscript, and take responsibility for its integrity. Shuang Zheng, Chian Kent Kwoh, Ming Lu, and David J. Hunter were also involved in the design, measurements, and statistical work. All authors critically appraised the manuscript and agreed to the final submission.
ETHICS STATEMENT
The study protocol, amendments, and informed consent documentation were reviewed and approved by the Institution Review Board at all participating sites.