Median nerve deformation in differential finger motions: Ultrasonographic comparison of carpal tunnel syndrome patients and healthy controls
Abstract
We investigated the median nerve deformation in the carpal tunnel in patients with carpal tunnel syndrome and controls during thumb, index finger, middle finger, and a four finger motion, using ultrasound. Both wrists of 29 asymptomatic volunteers and 29 patients with idiopathic carpal tunnel syndrome were evaluated by ultrasound. Cross-sectional images during motion from full extension to flexion were recorded. Median nerve cross-sectional area, perimeter, aspect ratio of the minimal enclosing rectangle, and circularity in extension and flexion positions were calculated. Additionally, a deformation index was calculated. We also calculated the intra-rater reliability. In both controls and patients, the median nerve cross-sectional area became significantly smaller from extension to flexion in all finger motions (p < 0.05). In flexion and extension, regardless of the specific finger motion, the median nerve deformation, circularity and the change in perimeter were all significantly greater in CTS patients than in controls (p < 0.05). We found excellent intra-rater reliability for all measurements (ICC > 0.84). With this study we have shown that it is possible to assess the deformation of the median nerve in carpal tunnel syndrome with ultrasonography and that there is more deformation of the median nerve in carpal tunnel syndrome patients during active finger motion. These parameters might be useful in the evaluation of kinematics within the carpal tunnel, and in furthering our understanding of the biomechanics of carpal tunnel syndrome in the future. © 2011 Orthopaedic Research Society. © 2011 Orthopaedic Research Society Published by Wiley Periodicals, Inc. J Orthop Res 30:643–648, 2012
Carpal tunnel syndrome is a compression neuropathy of the median nerve in the wrist. Patients with carpal tunnel syndrome (CTS) experience pain and weakness in the hand, and numbness and paresthesias in the first three digits. These symptoms were first described by Sir James Paget in 1854, although widespread recognition of the condition only happened in the 1950s because of the work of Phalen.1 However, the etiology of CTS remains idiopathic in most cases. Various anatomic, systemic, and occupational factors such as repetitive use of the wrist and digits have all been described as potential causative factors.2, 3 In other studies, the focus has been on biomechanical factors that might influence the development of CTS.4-6 The carpal tunnel contains nine different tendons and the median nerve, bound by the carpal bones on the dorsal side and the transverse carpal ligament on the volar side. Recent studies have demonstrated that even in healthy people, the median nerve gets compressed between the flexor retinaculum and the tendons during active finger motion.3, 7 In addition, several studies have shown that there is reduced longitudinal gliding of the median nerve in CTS patients.8, 9 This suggests that monitoring the motion and deformation of the median nerve by ultrasound may offer new insights into the mechanics within the carpal tunnel, and potentially serve as a new means by which CTS can be better understood, or perhaps even diagnosed. It is therefore important to characterize the deformation of the median nerve during finger motion in both CTS patients and normal controls. We hypothesized that there are detectable differences in deformation and motion of the median nerve in individuals with CTS, compared to healthy controls. If our hypothesis is supported, then these parameters would potentially be useful to use ultrasound as a noninvasive tool to study the genesis of CTS, and to monitor at risk individuals.
METHODS
Image Acquisition
 (1)
(1)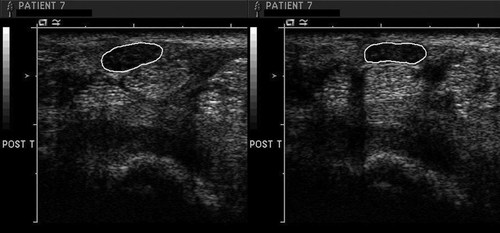
Example of outlining of the median nerve in middle finger motion from extension (left) to flexion (right) where the median nerve becomes smaller and squarer.
 (2)
(2)Statistical Analysis
All results were expressed in mean ± standard deviation (SD). Since we evaluated flexion and extension in both left and right wrist of healthy participants and patients with bilateral CTS, we used SAS procedure MIXED model approach for statistical analyses where participants were treated as repeated factor, wrists (left and right) as random effect factor, and fingers (four fingers, middle finger, index finger, and thumb) or motion direction (flexion/extension) as fixed effect factor. An overall p-value of <0.05 was considered significant for finger and motion differences. The post hoc comparisons were checked by the LSD rule. The reliability of five measurements was estimated by intra-class correlation coefficient (ICC). ICC had adopted the interpretation of Kappa statistics and an ICC > 0.75 was rated excellent. All statistical analyses were performed by SAS version 9.2 software (SAS Institute, Inc., Cary, NC).
RESULTS
The results of the absolute parameter measurements of the median nerve for all finger motions are shown in Table 1 and the deformation indices in Table 2.
| Indiparameters | Four Finger Motion | Middle Finger | Index Finger | Thumb | ||||
|---|---|---|---|---|---|---|---|---|
| Extension | Flexion | Extension | Flexion | Extension | Flexion | Extension | Flexion | |
| Area, mm2 (SD), (range) | ||||||||
| Control | 9.76 (2.42), (6.73–14.56) | 9.20 (2.46), (6.29–14.12) | 9.85 (2.35), (6.13–13.50) | 9.31 (2.50), (6.12–13.91) | 9.57 (1.99), (5.49–11.98) | 8.95 (1.91), (5.08–12.07) | 9.44 (2.00), (6.43–12.39) | 8.90 (1.86), (5.80–12.04) |
| Patient | 11.26 (4.05)*, (7.15–22.37) | 10.24 (3.59)*, (6.34–19.59) | 11.16 (3.86)*, (7.09–21.03) | 10.29 (3.69)*, (6.82–20.87) | 10.75 (3.65)*, (7.09–20.72) | 9.82 (3.42)*, (6.52–20.00) | 10.77 (3.97)*, (6.92–23.10) | 9.94 (3.72)*, (6.53–22.22) |
| Perimeter, mm (SD), (range) | ||||||||
| Control | 14.41 (2.68), (10.93–20.14) | 14.30 (2.66), (10.79–19.79) | 14.52 (2.73), (11.10–18.35) | 14.77 (2.83), (11.30–19.36) | 14.46 (2.12), (10.88–18.46) | 14.19 (2.15), (10.62–18.96) | 14.56 (2.00), (11.15–18.09) | 14.22 (1.89), (10.76–17.52) |
| Patient | 14.59 (4.06), (10.77–20.09) | 14.19 (3.87), (10.57–19.42) | 14.50 (3.97), (10.99–19.02) | 14.11(3.86), (10.92–20.10) | 14.38 (3.93), (10.85–18.53) | 14.09 (3.87), (10.48–19.52) | 14.22 (3.97), (11.22–21.29) | 14.05 (3.92), (11.00–20.55) |
| Aspect ratio of MER (SD), (range) | ||||||||
| Control | 0.37 (0.11), (0.22–0.62) | 0.34 (0.08), (0.22–0.49) | 0.35 (0.10), (0.21–0.56) | 0.32 (0.09), (0.20–0.51) | 0.37 (0.09), (0.21–0.54) | 0.37 (0.12), (0.23–0.74) | 0.35 (0.09), (0.21–0.55) | 0.35 (0.10), (0.19–0.54) |
| Patient | 0.38 (0.14), (0.23–0.73) | 0.36 (0.12)*, (0.24–0.68) | 0.38 (0.14)*, (0.24–0.75) | 0.36 (0.13)*, (0.24–0.69) | 0.37 (0.13), (0.23–0.63) | 0.34 (0.12)*, (0.23–0.57) | 0.38 (0.13)*, (0.25–0.65) | 0.36 (0.13), (0.25–0.67) |
| Circularity (SD), (range) | ||||||||
| Control | 1.72 (0.36), (1.29–2.51) | 1.81 (0.35), (1.36–2.53) | 1.74 (0.37), (1.26–2.52) | 1.90 (0.40), (1.38–2.63) | 1.71 (0.41), (1.29–2.49) | 1.77 (0.44), (1.26–2.49) | 1.81 (0.30), (1.43–2.70) | 1.84 (0.33), (1.35–2.97) |
| Patient | 1.54 (0.43)*, (1.19–2.22) | 1.59 (0.44)*, (1.22–2.20) | 1.53 (0.43)*, (1.20–2.15) | 1.57 (0.43)*, (1.18–2.12) | 1.56 (0.44)*, (1.24–2.32) | 1.64 (0.47)*, (1.30–2.39) | 1.52 (0.44)*, (1.21–2.24) | 1.62 (0.48)*, (1.24–2.46) |
- SD, standard deviation.
- * p < 0.05 between controls and patients.
| Deformation Index | Four Finger Motion | Middle Finger | Index Finger | Thumb |
|---|---|---|---|---|
| Area (SD), (range) | ||||
| Control | 0.94 (0.08), (0.74–1.12) | 0.95 (0.09), (0.75–1.17) | 0.94 (0.05), (0.80–1.05) | 0.94 (0.06), (0.81–1.11) |
| Patient | 0.91 (0.05)*, (0.75–1.02) | 0.92 (0.06)*, (0.78–1.07) | 0.91 (0.05)*, (0.76–1.04) | 0.92 (0.05)*, (0.80–1.07) |
| Perimeter (SD), (range) | ||||
| Control | 1.00 (0.06), (0.88–1.18) | 1.02 (0.07), (0.84–1.16) | 0.98 (0.04), (0.88–1.06) | 0.98 (0.04), (0.89–1.06) |
| Patient | 0.97 (0.03)*, (0.90–1.07) | 0.97 (0.05)*, (0.88–1.09) | 0.98 (0.04)*, (0.84–1.09) | 0.99 (0.03)*, (0.90–1.08) |
| Aspect ratio of MER (SD), (range) | ||||
| Control | 0.94 (0.19), (1.56–1.55) | 0.94 (0.24), (0.55–1.79) | 1.01 (0.18), (0.74–1.59) | 1.00 (0.10), (0.83–1.26) |
| Patient | 0.97 (0.11), (0.71–1.21) | 0.96 (0.17), (0.64–1.64) | 0.94 (0.12)*, (0.75–1.23) | 0.95 (0.08)*, (0.78–1.18) |
| Circularity (SD), (range) | ||||
| Control | 1.06 (0.11), (0.81–1.48) | 1.10 (0.14), (0.79–1.62) | 1.03 (0.09), (0.84–1.27) | 1.01 (0.06), (0.90–1.15) |
| Patient | 1.04 (0.06)*, (0.86–1.18) | 1.03 (0.085)*, (0.82–1.20) | 1.05 (0.06), (0.91–1.17) | 1.06 (0.05), (0.94–1.19) |
- SD, standard deviation.
- * p < 0.05 between controls and patients.
Four Finger Motion
The cross-sectional area of the median nerve was greater in CTS patients in both extension and flexion positions than in controls (p < 0.0001), but the perimeter, however, was not different between the two groups. For the deformation index, there was a significant difference for both area and perimeter (p = 0.0004 and p = 0.0009, respectively), showing that there is a change in shape between extension and flexion. The circularity was less in patients than in controls, as was the DI for circularity (p < 0.0001 and p = 0.0063, respectively), meaning that the shape of the median nerve is closer to a perfect circle in patients. The aspect ratio of the minimal enclosing rectangle was 0.34 in controls and 0.36 in patients (p = 0.002).
Middle Finger Motion
The area of the median nerve was greater in patients than in controls in both flexion and extension (p < 0.0001), with a significant difference in deformation index (p = 0.002). There were no significant differences in absolute perimeter measurement, although the DI was smaller in patients (p < 0.0001). Circularity measurements were greater in controls than in patients in both flexion and extension (p < 0.0001), as was the DI (p < 0.0001). The aspect of the minimal enclosing rectangle was higher in patients (p > 0.05).
Index Finger Motion
The cross-sectional area of the median nerve was smaller in controls than in patients (p < 0.0001) in both flexion and extension. The deformation indices for both the area and the perimeter were significantly different between both groups, with p-values of <0.0001 and 0.0009. The circularity of the median nerve was greater in controls than in patients (p < 0.0001 in extension and p = 0.0065 in flexion), showing that the nerve in patients is closer to a perfect circle than in controls. For the aspect ratio of the MER, there was a difference between the groups in flexion (p = 0.0045), while the deformation index was smaller in patients (p < 0.0001).
Thumb Motion
In thumb motion, the cross-sectional area of the median nerve was smaller in controls than in patients, in both flexion and extension (p < 0.0001). There was no difference in perimeter, but the deformation index for both area measurements as well as for perimeter were significantly different between the two groups. The median nerve was more circular in patients than in controls in both flexion and extension (p < 0.0001). For the aspect ratio of the MER, there was only a difference in extension (p = 0.001) and in DI (p < 0.0001).
Reliability
For all measurements the ICC was excellent with values ranging from 0.84 to 0.98.
DISCUSSION
In this study we have shown that in flexion and extension, regardless of the specific finger motion, the median nerve cross-sectional area and deformation of the median nerve are greater in CTS patients than in controls. We believe that these are important observations for several reasons.
The tendons and median nerve move in a three-dimensional plane during finger motion.3, 7 Because the carpal tunnel is a closed space, the median nerve cannot move away from the tendons and thus gets compressed causing a change in shape and area. As noted by others, these parameters may be useful as a tool for diagnosing CTS with ultrasound.8-12 Our results show that the best parameters seem to be the cross-sectional area and the area deformation index (Tables 1 and 2). While circularity measurements were also different in all finger motions, this deformation index was only significantly different in four finger and middle finger motion, so this measure would probably not be useful for clinical purposes. As shown in Tables 1 and 2, the results of perimeter and MER measurements are also too inconsistent for clinical use. Other investigators have studied median nerve cross-sectional area in CTS, with reported values ranging from an average cross-sectional area of the median nerve at the distal wrist crease of 7–9 mm2 in asymptomatic volunteers to 13.7–16.8 mm2 in CTS patients.10, 12-14 Klauser et al. compared the cross-sectional area of the median nerve (CSA) at two different levels. They found an average CSA of 16.8 mm2 in patients and 9.0 mm2 at the carpal tunnel level, and 9.5 mm2 in patients and 8.7 mm2 in controls at a more proximal level.12 They also calculated the difference between those two measurements and found a 99% sensitivity and 100% specificity for these measurements. However, absolute value measurements in the carpal tunnel may also be dependent on confounders such as gender and wrist size. We believe that the amount of compression is therefore best shown by a deformation index, as calculated in this study, since it is unaffected by absolute size. Since the measurements for the median nerve area were different both in normal measurements as well as in deformation index, we believe this would be the best potential parameter to distinguish between patients and healthy individuals in supporting a clinical diagnosis of CTS. Sernik et al.14 showed the median nerve cross-sectional area was increased compared to their control group and they suggest a cut off point of 10 mm2, but the reliability, specificity, and sensitivity of such measures were not rigorously compared to other diagnostic measures, such as electrodiagnosis, clinical findings, or differences between flexion and extension values. Other studies suggest cut-off values of 9–11 mm2, with high sensitivity and specificity levels.10, 13 Based on our results we would suggest using a cut-off value of 10 mm2, measuring the area with middle finger motion since we noticed during image acquisition that the third superficial flexor digitorum tendon is the easiest tendon to recognize compared to the other tendons.
Finally, and most importantly, we believe the measures described here may be useful in noninvasive study of mechanical behavior related to the median nerve in health and disease. A combination of longitudinal and cross-sectional data could generate three-dimensional images of the carpal tunnel contents; the dynamic aspect imparts a fourth dimension, that of movement over time. Such imaging could be used to investigate, and even monitor, the mechanical behavior of the nerve and tendons within the carpal tunnel, not only for simple motions, as described here, but also for more task-related activities, such as pinching, gripping, or keyboarding. Such investigations may shed further light on activities likely to deform the median nerve.
Our study has some short comings. As shown in Tables 1 and 2, differences in healthy volunteers are very small between flexion and extension, and one finding was different from the general trend in results: the perimeter in middle finger motion was higher at flexion than in extension in controls.
Ultrasound is known to have measurement errors due to operator-differences like experience, but also technical differences like the angle of the transducer to the wrist. Even though fixed the transducer in a special holder, motion of the patient may have influenced the results. The angle in which the transducer is placed on the patients' wrist is also important: in case of a smaller angle (than 90°, like ours) the cross-section of the median nerve might become bigger, for example. Another cause could be the level of the carpal tunnel at which the measurement is taken: our measurements were taken at the wrist crease level, just proximal to the tunnel. If images were taken more distally, within the tunnel, the median nerve might be more compressed. Also, during finger motion, the tendons move towards the median nerve, thereby compressing it. This happens in both healthy controls and in CTS patients, as shown with this study. It is logical to think that the median nerve might flatten with finger flexion, as the tendons press against the nerve from below. For a given cross-section, a circular shape will have a smaller perimeter than an elliptical shape. This means that even in healthy subjects, due to the change in shape, the perimeter might change as well, but this effect might differ between different locations along the course of the nerve.
Secondly, our results are not categorized by severity of CTS. We do believe it would be useful to study the relation between duration of symptoms, severity of the electrophysiological changes, and deformation of the median nerve. This would be a useful next step towards using ultrasound parameters for diagnosing CTS in an early stage. There was a statistically significant age difference between our patient and control groups which may have caused bias in our results, since theoretically the difference in shape may have been caused by a normal aging process rather than disease.
The intra-rater reliability was calculated from five repetitions within each finger motion measurement, all done by one not-blinded investigator within the same session. Ideally, a more true representation of the intra-rater reliability would have been to compare multiple repetitions within more than one session. Also, even though it is known that ultrasound is a highly operator-dependent tool, we did not calculate inter-observer reliability. This remains for future studies.
We conclude that it is possible to investigate the deformation of the median nerve in CTS by ultrasonography and that there is more deformation of the median nerve in CTS patients during active finger motion. These parameters might be useful in the future as an additional tool for diagnosing or assessing the biomechanics of CTS.
Acknowledgements
The project described was supported by Grant Number AR49823 from NIH/NIAMS, and was performed in our Clinical Research Unit, which is supported by NIH grant RR024150.




