Comment on “The association of sickle cell disorder with adverse outcomes in COVID-19 patients: A meta-analysis”
Liang et al. conducted an important and timely meta-analysis examining the risk of adverse coronavirus disease 2019 (COVID-19) outcomes in patients with sickle cell disease (SCD) and sickle cell trait.1 They synthesized data across 21 studies and found significantly increased risks of mortality, hospitalization, and intensive care unit (ICU) admission among SCD patients with COVID-19.1 Increased risks of mortality and hospitalization were also observed for sickle cell traits. Understanding the impact of hematologic conditions, such as SCD, on COVID-19 outcomes is crucial for informing clinical practice and public health policies. The analysis by Liang et al.1 provided evidence that patients with SCD are particularly vulnerable during the pandemic. The authors should be congratulated for their efforts to characterize the risk and fill the knowledge gaps around COVID-19 and SCD.
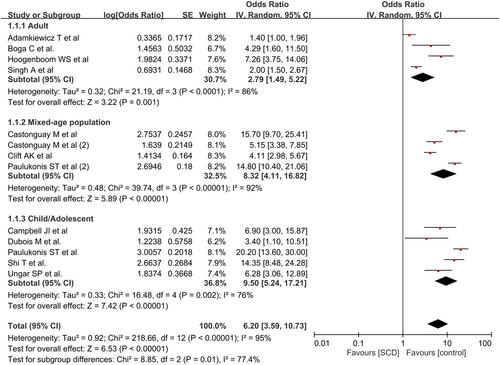
However, we wish to emphasize a significant issue that could enhance the comprehensiveness of the study by Liang et al.1 The authors found that SCD significantly increased the risk of hospitalization (pooled odds ratio: 6.21) compared with other outcomes such as mortality (pooled odds ratio: 1.7) and intensive care unit (ICU) admission (pooled odds ratio: 2.29).1 This highlights that hospitalization is a major burden for patients with SCD and COVID-19. Prevention of hospitalization could greatly reduce healthcare costs and resource utilization in this vulnerable population and should be the top priority in this population. However, there was a significant unexplained heterogeneity (I2 = 94.4%) in the hospitalization analysis. Although the authors1 conducted meta-regression around study characteristics such as location and design, the source of heterogeneity remains unclear. We propose that patient age could be a contributing factor given the inclusion of various age groups (i.e., children, adolescents, and adults) in the original meta-analysis.1 To investigate this, we conducted an additional subgroup analysis, splitting the studies into adults (≥18 years old), mixed-age populations (including both children/adolescents and adults), and children/adolescents (<18 years old). The raw data in the original meta-analysis1 were analyzed using the Cochrane Review Manager (RevMan 5.3; Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). As shown in Figure 1, heterogeneity was reduced within all subgroups, suggesting that age may be another contributing factor to heterogeneity. Interestingly, the children/adolescent subgroup (pooled odds ratio: 9.5, 95% confidence interval: 5.24–17.21) showed a higher risk of hospitalization than the adult subgroup (pooled odds ratio: 2.79, 95% confidence interval: 1.49–5.22), implying that children and adolescents with SCD could be at a greater risk for COVID-19 hospitalization than adults (subgroup difference p = 0.01).
While anthropometric factors may contribute, these factors alone cannot fully explain the poor COVID-19 outcomes in children and adolescents with SCD. Intrinsic abnormalities in innate immune function are likely to play a key role. For example, toll-like receptors (TLRs) are essential for mediating and regulating the body's immune defense, and the involvement of TLRs on the surface of human cells in the inflammatory process triggered by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been reported.2-5 In patients with SCD, there is an increase in TLR4 activity, which may predispose patients to heightened inflammatory reactions to infections.6 This is particularly concerning for children and adolescents with SCD, as their pre-existing inflammatory state may predispose them to amplified TLR4-driven responses, thereby increasing their risk of requiring hospital care.
In conclusion, our analysis underscores the increased hospitalization risk among patients with SCD, particularly in the younger population. Prevention of hospitalization, especially in children and adolescents with SCD, should be prioritized during the COVID-19 pandemic. Further age-stratified research is crucial to understand and mitigate these risks.
AUTHOR CONTRIBUTIONS
I-Wen Chen, Hsiu-Jung Lin, and Kuo-Chuan Hung wrote the main manuscript text. Yao-Tsung Lin prepared Figure 1. All authors read and approved the final version of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.




