Eliminating cervical cancer in China: Opportunities come and challenges remain
Xu Ou-Yang and Yang Cao contributed equally to this study.
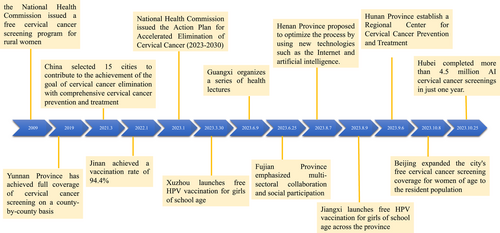
Cervical cancer ranks as the fourth leading cause of cancer incidence and mortality among women globally, accounting for approximately 600 000 new cases and 300 000 deaths annually. Notably, China contributes to nearly 20% of its worldwide burden.1 Between 1990 and 2019, Chinese women experienced 1 145 534 fatalities attributable to this disease.2 In response to this significant public health challenge, China has embarked on an ambitious series of public health interventions aimed at the elimination of cervical cancer (Figure 1).
Persistent infection with high-risk human papillomavirus (HPV) genotypes is the primary etiological factor for the development of precancerous lesions and invasive cervical cancer. The most prevalent high-risk HPV types in descending order of frequency are 16, 18, 45, 31, 33, 52, 58, and 35,3 with HPV16 and 18 as the most common causes, accounting for 39%–78% of all cervical cancer cases.4 HPVs are composed of double-stranded DNA that includes two primary functional genomic domains: (i) the early region, which encodes proteins E1, E2, E4, E5, E6, and E7 responsible for viral replication, transcription, and oncogenesis; and (ii) the late region, which codes for L1 and L2 capsid proteins. Specifically, E1 and E4 play pivotal roles in viral replication and transcription, while E5 enhances the oncogenic functions of E6 and E7.5 Typically, upon disruption of the epithelial barrier, HPVs penetrate the basal layer of the epithelium and may integrate their DNA into the host genome. This integration commonly results in the disruption of the E2 open reading frame, leading to the derepression of oncogenic proteins E6 and E7. Subsequently, E6 and E7 proteins interfere with cell growth regulatory pathways, particularly by inactivating the retinoblastoma protein family and p53, which are crucial for cell cycle regulation and the prevention of unchecked cellular proliferation.6 Persistent HPV infection coupled with unregulated cell cycle progression may lead to genomic instability in host cells. This instability can precipitate genetic mutations and epigenetic alterations, which are contributory factors in oncogenesis.
Additionally, HPVs have evolved various mechanisms to evade host immune responses, thereby facilitating carcinogenic processes.7 HPV can evade innate immune reactions by altering the pathogen recognition receptors of antigen-presenting cells, disrupting the immunological defenses of Langerhans cells, and affecting the maturation pathways of dendritic cells. Specifically, HPV16 can suppress the host's innate immune response by inhibiting the recruitment of macrophages and other immune cells. Both HPV16 and 18 can evade innate immune responses by suppressing the synthesis of interferons. Furthermore, HPV can avoid adaptive immune responses by modulating the level of T regulatory cells, leading to immune suppression.8 In conclusion, the pathogenesis of HPV-induced cervical cancer is a multifaceted and intricate process that involves viral DNA integration, inactivation of tumor suppressor proteins, deregulation of the cell cycle, and subsequent genetic and epigenetic modifications.
Given that persistent HPV infection is the primary etiological factor for cervical cancer, preventive strategies are centered on screening for early detection and prophylactic vaccination against HPV.3 The HPV vaccine effectively prevents infections from targeted HPV types by eliciting the production of neutralizing antibodies, which impede the viral particles' entry into host cells. A plethora of studies have demonstrated that HPV vaccination can significantly prevent or mitigate the incidence of cervical cancer.7, 9 Research has indicated that the combination of one or two primary HPV screenings with vaccination initiatives can accelerate the reduction in cervical cancer incidence compared to programs relying solely on vaccination.10, 11
In November 2020, the World Health Organization promulgated the Global Strategy to accelerate the elimination of cervical cancer, endorsed by 194 member states, including China. This ambitious strategy sets a target for at least 90% of girls to be fully vaccinated against HPV by the age of 15 by the year 2030, as a crucial step toward eradicating cervical cancer as a public health concern.12 Comparison of HPV vaccination policies among China, United States, and European Union was shown in Table 1.
| China | United States | European Union | |
|---|---|---|---|
| HPV vaccination | In 2021, some cities initiated a free HPV vaccination program, with plans to gradually expand the scope. The target demographic includes middle to high school female students, with a regimen of two to three doses.33 | Since 2006, free HPV vaccinations have been offered to all 11–12-year-old girls nationwide. In 2011, the recommendation was extended to adolescent boys.13 | By December 2021, all European Union countries had introduced HPV vaccination into their national plans, with many proposing universal or gender-neutral vaccination strategies.14 |
| Cervical cancer screening | Cervical cancer screening was Initiated in 2009, which was included in basic public health services by 2019.34 | Cervical cancer screening was funded for eligible individuals since 1990.35 | Finland, Luxembourg, and Sweden established national screening programs as early as the 1960s. The “European Guidelines” published in 1993 are followed by all member states to ensure the quality of cervical cancer screening.15 |
| Public education and awareness campaigns | Continuous health education was conducted targeting different social groups through the internet.27, 28 | Educational campaigns such as “Survivor videos” and the “HPV vaccination clearinghouse” project, was implemented.16 | Health authorities and immunization managers utilize social media for enhanced awareness campaigns, along with testing interventions to reduce vaccine hesitancy.17 |
| Expected goals | By 2025, China aims for a 50% cervical cancer screening rate among eligible women and to pilot HPV vaccination services for eligible girls. By 2030, the goal is to reach a 70% screening rate and continue the HPV vaccination pilot for eligible girls.25 | By 2030, US aims to vaccinate 90% of girls against HPV before the age of 15 and conduct cervical cancer screening for 70% of women before the ages of 35 and 45.18 | In September 2019, the European Cancer Organization passed a resolution during the European cancer summit to plan the elimination of all HPV-related cancers.19 |
| Challenges | Public hesitancy towards vaccines, high vaccine costs, and the need to address the demands of low-resource areas like rural regions.30, 31 | Lower vaccination and cervical cancer screening rates among minority ethnic groups, rural residents, those with limited English proficiency, and individuals with specific religious beliefs.18 | Expansion to male vaccination could lead to shortages of the human papillomavirus vaccine; a global shortage of HPV vaccines is expected to continue at least until 2024.14 |
In China's private market for HPV vaccines, coverage among the recommended younger age group of 9–14 years remains under 1% as of 2020, with most vaccinations being administered to adult women.20 Currently, free vaccination programs offer only the bivalent domestic vaccine to females.21 The market has five types of prophylactic vaccines available: the bivalent HPV vaccine (AS04-HPV-16/18), quadrivalent HPV vaccine, 9-valent HPV vaccine, and two domestically produced bivalent vaccines using Escherichia coli and Pichia pastoris.22 These vaccines have undergone clinical trials in China and are recognized for their tolerability and immunogenicity. However, vaccination is not yet extended to males, highlighting a gap in the national HPV prevention strategy.
China has implemented comprehensive measures toward the elimination of cervical cancer (Figure 1). In 2009, the National Health Commission of China incorporated a complimentary cervical cancer screening initiative for rural women into its essential public health services. Following the initiation of this program, Yunnan Province has accomplished complete coverage of cervical cancer screenings on a county-by-county basis.23 In March 2021, China initiated a program in 15 cities to contribute towards the national goal of cervical cancer elimination by integrating comprehensive prevention and treatment strategies. As a part of this initiative, Jinan City in Shandong Province commenced an HPV vaccination campaign in November 2021. By January 2022, the campaign achieved a vaccination rate of 94.4% in Jinan City.24
In January 2023, the National Health Commission of China, in collaboration with 10 other departments, promulgated the Action plan for the accelerated elimination of cervical cancer (2023–2030). This plan sets forth goals to achieve a 70% cervical cancer screening rate among eligible women and a 90% treatment rate for individuals with cervical cancer and precancerous lesions by the year 2030.25 For women aged 21–29, thinprep cytology test (TCT) is used, while women aged 30–65 are screened using a combination of TCT and HPV testing.23 To enhance the execution of this policy, Fujian Province underscored the importance of multisectoral collaboration and social participation on June 25, 2023, actively advocating for the uptake of HPV vaccination.26 On August 7, 2023, Henan Province unveiled a proposal to refine the continuum of cervical cancer services, from screening to diagnosis and treatment, by integrating advanced technologies like the Internet and artificial intelligence.27 On September 6, 2023, Hunan Province announced the establishment of a Regional Center for Cervical Cancer Prevention and Treatment. This center will be tasked with the development of standardized guidelines for the screening and treatment of cervical cancer and will provide specialized training for healthcare professionals involved in these services.28 On October 8, 2023, Beijing extended its free cervical cancer screening program to encompass all resident women within the targeted age demographic.29
As the stipulated policies are progressively enacted, a decline in the incidence of cervical cancer is anticipated, which is expected to alleviate the disease burden of cervical cancer in China. The analysis conducted by the WHO Cervical Cancer Elimination Modeling Consortium, utilizing three distinct transmission dynamic models, offers significant insights into cervical cancer prevention strategies. These models indicate that exclusive HPV vaccination of girls notably lowers cervical cancer incidence in low- and middle-income nations. Enhanced screening programs can contribute to further incidence reduction. Predictions suggest that regions adhering solely to female HPV vaccination could potentially achieve cervical cancer elimination between 2059 and 2102. The integration of biannual cervical cancer screenings could expedite this achievement by 11–31 years, underscoring the profound impact of combined preventive and screening efforts in curtailing cervical cancer incidence.11
Despite this progress, the path forward for cervical cancer elimination in China requires ongoing commitment and focused strategies. Key among these is enhancing HPV vaccination rates, especially in underserved rural areas. Addressing the challenges of health awareness, economic constraints, and vaccine hesitancy in these regions is critical. Government-led initiatives and healthcare campaigns should prioritize HPV vaccination for girls in resource-limited settings, actively countering vaccine hesitancy. In terms of educational efforts, studies indicate a need for improved awareness and knowledge about HPV vaccination and screening among Chinese youth.30, 31 Varying public perceptions and concerns about vaccine confidence and accessibility have impacted uptake. Collaborative educational campaigns, led by governmental, healthcare, and educational institutions, are vital. Incorporating HPV-related health education in school curricula at different levels and leveraging social media platforms like TikTok, WeChat, and Weibo are effective ways to disseminate information widely. In resource-poor areas, misconceptions about cervical cancer prevention and screening can be addressed through targeted media strategies, including television, radio, and social media. Such multipronged educational efforts are essential to foster active participation in cervical cancer prevention and screening. Further, the development and refinement of a data collection and surveillance system for cervical cancer is imperative. This system would enable comprehensive monitoring of incidence and mortality rates, guiding the development of targeted interventions. Lastly, advancing scientific research on cervical cancer and exploring new treatment modalities remain crucial. Current treatments, including radiotherapy, chemotherapy, and surgery, have limitations, especially for advanced stages of cervical cancer. The emergence of immunotherapy, particularly PD1 inhibitors for recurrent or metastatic cases, opens new therapeutic possibilities. Combining immunotherapies, like vaccines or adoptive cell transfer, can enhance the immune response against HPV-positive cancer cells, representing a significant advancement in cervical cancer treatment.32 These concerted efforts are fundamental to achieving the goal of eliminating cervical cancer in China, addressing both the medical and socioeconomic aspects of this public health challenge.
AUTHOR CONTRIBUTIONS
Xu Ou-Yang: Conceptualization; methodology; formal analysis; resources; investigation; writing—original draft. Yang Cao: Conceptualization; methodology; resources; investigation; writing—original draft; writing—review and editing. Qihao Leng: Conceptualization; methodology; data curation. Yan Wang: Conceptualization; methodology; data curation. Hang Yi: Conceptualization; methodology; writing—review and editing. Guochao Zhang: Formal analysis; resources; investigation; formal analysis; resources; investigation.
ACKNOWLEDGMENTS
This work was supported by The Special Research Fund for Central Universities, Peking Union Medical College (2022-I2M-C&T-B-065, 2022-I2M-C&T-B-060); National High-Level Hospital Clinical Research Funding (2022-PUMCH-A-018, 2022-PUMCH-C-043); National Key R&D Program of China (2022YFC2407404); Beijing Municipal Science & Technology Commission (Z211100002921058).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




