Global and regional estimates of cervical cancer burden associated with human immunodeficiency virus infection from 1990 to 2019
Zhengwei Wan and Jianhui Zhao shares first authorship.
Abstract
Previous studies reported human immunodeficiency virus (HIV) could enhance human papillomavirus (HPV)-induced cervical cancer. Therefore, the burden of cervical cancer associated with HIV across different regions and time periods need to be assessed. We aim to investigate the global burden of cervical cancer associated with HIV infection. Age standardized rates (ASRs) of cervical cancer disability-adjusted life-years (DALYs) in females (≥15 years old) were calculated by standardization, according the age-specific DALYs numbers extracted from GBD data set 2019. Population attributable fractions was calculated by combining the published risk ratio, with the HIV prevalence (≥15 years old) from Joint United Nations Programme on HIV and AIDS (UNAIDS), and transferred to estimate the HIV-associated cervical cancer burden. Expected annual percentage changes (EAPCs) was calculated to describe the temporal trend of ASR from 1990 to 2019. Pearson correlation analysis were conducted to assess the correlation between the ASR or EAPCs and the socio-demographic index. The worldwide DALYs ASR caused by HIV-associated cervical cancer rose from 3.78 (95% confidence interval [CI]: 2.19–5.56) in 1990 to 9.50 (95% CI: 5.66–13.79) in 2019 per 100k population. In 2019, the region with the greatest burden was Eastern and Southern Africa, with the highest DALYs of 273 900 (95% CI: 149 100–476 400) and ASR of 254.44 per 100k population (95% CI: 168.86–329.28). Notably, the Eastern Europe and Central Asia regions had the highest EAPC (14.07%) of HIV-associated DALYs ASR. Women in Eastern and Southern Africa experience the greatest burden of HIV-associated cervical cancer, while the Eastern Europe and Central Asia regions had witnessed the largest increase over the last 30 years. Prioritize the promotion of HPV vaccination and cervical cancer screening for women living with HIV were crucial in these regions.
1 INTRODUCTION
Cervical cancer is the fourth most commonly diagnosed cancer among women globally,1 and it is the leading cause of cancer-related mortality among women in sub-Saharan Africa.2 Women living with human immunodeficiency virus (HIV) are reported to have a sixfold higher risk of cervical cancer than those without HIV.3 The burden of cervical cancer associated with HIV has become a significant concern and requires a global assessment.
The disease burden of cervical cancer is featured with geographical disparities. Previous studies have shown that 9 out of 10 cervical cancer deaths occur in low- and middle-income countries (LMICs),2 and the inequality in burden continues to rise.3 Of note, in 2020, about 15.4 million women living with HIV in sub-Saharan Africa where is lack of medical resources.4 The high prevalence of HIV infection might result in heavy burden of cervical cancer associated with HIV. Although high-income countries are on track to eliminate cervical cancer in the coming decades, the incidence of cervical cancer kept rising or remained in regions such as some sub-Saharan African, eastern European and western Asian countries.3, 5, 6 Therefore, understanding the regional patterns in cervical cancer burden attributable to HIV infection from 1990 to 2019 is crucial to reduce the geographical disparities in the burden of cervical cancer.
In recent decades, there has been a declining trend in the mortality of cervical cancer in women. This phenomenon is largely attributed to the development of early detection and treatment technologies,7 as well as the application of a human papillomavirus (HPV) vaccine. Cervical cancer is the most prevalent malignancy among HIV-positive women, and HIV-positive women were more likely to develop invasive cervical cancer.8 Meanwhile, antiretroviral therapy (ART) has increased the life expectancy of people living with HIV, which accompanied by an increased risk of cancer related to HIV/AIDS.9 Therefore, prevention, early detection, and treatment of cervical neoplasia are essential components of the care of HIV-infected women.
Currently, the contribution of HIV to the disease burden of cervical cancer across times and regions has yet to be comprehensively reported and quantified. In this study, we aim to use the reported relative risk (RR) for cervical cancer among women living with HIV, HIV prevalence from Joint United Nations Programme on HIV and AIDS (UNAIDS), and epidemic data of cervical cancer from GBD, to estimate the global and regional disease burden and relative change of cervical cancer attributed to HIV/AIDS from 1990 to 2019. This study has a contribution to policy development on the prevention of cervical cancer and HIV worldwide, and to reducing the disease burden of cervical cancer associated with HIV.
2 MATERIALS AND METHODS
2.1 Data source
To perform the population attributable fraction (PAF) analysis, we obtained HIV prevalence data for women (aged ≥15 years) from UNAIDS for the years 1990–2019, at the global, regional, and national levels (https://aidsinfo.UNAIDS.org). The UNAIDS categorized the world into eight regions, including the Asia and the Pacific, the Eastern Europe and Central Asia, the Middle East and North Africa, the East and Southern Africa, the Caribbean, the West and Central Africa, the Latin America and the Western and Central Europe and North America (Supporting Information: Table 1). National HIV prevalence was available for 170 of 194 UN member countries. We downloaded the number of disability-adjusted life-years (DALYs) for individuals aged 15 years and above, in 5-year intervals, from 1990 to 2019 by the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool) for 204 countries. The socio-demographic index (SDI) was estimated based on the country development, and composite of the country's total fertility rate for women younger than 25 years, educational attainment, and lag-distributed income per capita, by the Institute for Health Metrics and Evaluation (IHME) for 204 countries. While UNAIDS models the prevalence of HIV infection for 170 countries, the prevalence data of 36 countries (China, USA, Russia, et al.) was not made publicly available. Therefore, the population attribution estimates at the national level in our study were limited to the remaining 134 countries.
2.2 Estimation of PAFs and HIV-associated DALYs
2.3 Estimates of age standardized rates (ASR) and expected annual percentage changes (EAPCs)
We calculated ASR of DALYs and corresponding 95% confidence intervals by standardization (Supporting Information: Appendix 1), based on the world standard population reported in the GBD 2019, by global, regional, and national.13 HIV-attributed ASRs of DALYs (per 100k population) were also calculated using multiplying the ASRs of DALYs cervical cancer (per 100k population) by the PAF each year.
Where the EAPC values and their 95% CI > 0 were defined as significant increase. In contrast, a significant decreasing was defined when the EAPC values and their 95% CI < 0.
2.4 Estimates the association between ASRs/EAPCs with SDI
In this study, Pearson correlation analysis was further performed to assess the correlation between the ASRs (2019)/EAPCs with the SDI (2019) at the country levels. A general linear model and local weighted regression were used to fit the correlation curves. All the statistical analyses and choropleth maps in this study were finished using the R 4.0.3 (Lucent Technologies). A two-sided p value less than 0.05 was considered statistically significant.
3 RESULTS
In 2019, the UNAIDS estimated the global prevalence of HIV infection in young and adult female was 0.67% (95% CI: 0.53–0.80) (Table 1). By utilizing the HIV prevalence rate, combined RR of 6.07 for HIV and cervical cancer, and epidemic data of cervical cancer, our analysis yielded a global PAF of 3.22% (95% CI: 1.92–4.68) for cervical cancer DALYs attributed to HIV infection. Furthermore, we estimated a global age-standardized DALYs rate of cervical cancer associated with HIV of 9.50 (95% CI: 5.66–13.79) per 100k population in 2019 (Table 1). At the regional level, in 2019, the highest PAFs were observed in the Eastern and Southern Africa region (PAF: 29.28%, 95% CI: 19.45–37.88), followed by the Western and Central Africa (PAF: 7.88%, 95% CI: 4.79–11.26) (Table 1). Our findings indicate that among all the regions examined (Table 1), the Eastern and Southern Africa region had the highest ASR of cervical cancer associated with HIV (254.44 per 100k population, 95% CI: 168.86–329.28), while the Middle East and North Africa had the lowest ASR (0.4 per 100k population, 95% CI: 0.23–0.61) (Table 1). Out of the 170 countries covered by UNAIDS, HIV prevalence data were available for 134 countries (Supporting Information: Table 1). The Eastern and Southern Africa region had the highest PAFs, with Swaziland (62.90%, 95% CI: 60.84–64.79), Lesotho (57.34%, 95% CI: 54.77–59.74), and Botswana (56.67%, 95% CI: 54.70–58.54) showing the highest rates (Figure 1A and Supporting Information: Table 2). Regarding absolute numbers, the highest DALYs of cervical cancer associated with HIV were recorded in South Africa (71 238, 95% CI: 47 937–103 408), with Mozambique (30 535) and Tanzania (28 934) following behind (Figure 1B and Supporting Information: Table 3). Lesotho had the highest ASR of cervical cancer associated with HIV-related DALYs, with 872.15 per 100k population (95% CI: 682.03–995.10) (Figure 1C and Supporting Information: Table 3).
| UNAIDS regions | Year | HIV prevalence (%) | PAF (%) | All-cause DALYs (×1000) | HIV-associated DALYs (×1000) | All-cause DALYs ASR (per 100k population) | HIV-associated DALYs ASR (per 100k population) |
|---|---|---|---|---|---|---|---|
| Global | 1990 | 0.20 (0.16, 0.24) | 0.98 (0.57, 1.44) | 6176.25 (5410.77, 7410.74) | 60.46 (34.83, 92.39) | 384.83 (384.53, 385.14) | 3.78 (2.19, 5.56) |
| 2019 | 0.67 (0.53, 0.80) | 3.22 (1.92, 4.68) | 8955.01 (7595.43, 10140.16) | 288.37 (168.31, 430.8) | 294.7 (294.51, 294.90) | 9.50 (5.66, 13.79) | |
| Asia and the Pacific | 1990 | 0.02 (0.02, 0.03) | 0.10 (0.06, 0.16) | 2886.32 (2068.63, 4218.83) | 2.98 (1.51, 5.23) | 352.16 (351.75, 352.58) | 0.37 (0.21, 0.55) |
| 2019 | 0.13 (0.1, 0.16) | 0.64 (0.36, 0.96) | 4508.84 (2904.76, 6276.44) | 28.61 (14.53, 49.94) | 263.39 (263.14, 263.63) | 1.67 (0.95, 2.52) | |
| Caribbean | 1990 | 0.53 (0.45, 0.62) | 2.63 (1.58, 3.74) | 71.39 (44.84, 98.41) | 1.86 (0.98, 3.21) | 819.00 (812.93, 825.13) | 21.57 (12.89, 30.57) |
| 2019 | 1.09 (0.94, 1.29) | 5.30 (3.22, 7.49) | 107.28 (60.71, 163.62) | 5.60 (2.81, 10.33) | 665.31 (661.33, 669.31) | 35.29 (21.43, 49.87) | |
| Eastern and southern Africa | 1990 | 3.42 (2.76, 4.07) | 14.6 (9.11, 20.04) | 543.1 (318.33, 833.75) | 78.36 (40.72, 139.74) | 1107.45 (1104.4, 1110.52) | 161.76 (100.85, 221.83) |
| 2019 | 8.28 (6.67, 9.85) | 29.28 (19.45, 37.88) | 946.56 (580.29, 1498.49) | 273.74 (150.23, 476.92) | 868.94 (867.12, 870.77) | 254.44 (168.86, 329.28) | |
| Eastern Europe and central Asia | 1990 | 0.00 (0.00, 0.00) | 0.00 (0.00, 0.01) | 446.27 (365.04, 514.39) | 0.02 (0.01, 0.03) | 333.84 (332.84, 334.85) | 0.01 (0.01, 0.02) |
| 2019 | 0.50 (0.45, 0.56) | 2.50 (1.52, 3.49) | 421.59 (306.14, 555.58) | 10.42 (5.9, 16.46) | 274.86 (274.01, 275.71) | 6.86 (4.17, 9.58) | |
| Latin America | 1990 | 0.06 (0.04, 0.08) | 0.29 (0.16, 0.47) | 767.46 (653.31, 908.04) | 2.20 (1.17, 3.71) | 720.06 (718.42, 721.71) | 2.07 (1.12, 3.39) |
| 2019 | 0.26 (0.17, 0.35) | 1.21 (0.66, 1.98) | 1059.27 (822.96, 1400.01) | 12.8 (6.58, 22.4) | 438.24 (437.41, 439.08) | 5.31 (2.88, 8.67) | |
| Middle East and North Africa | 1990 | 0.01 (0.00, 0.01) | 0.03 (0.02, 0.05) | 118.42 (68.86, 179.52) | 0.04 (0.02, 0.07) | 208.67 (207.44, 209.92) | 0.06 (0.04, 0.09) |
| 2019 | 0.05 (0.04, 0.06) | 0.26 (0.15, 0.39) | 224.2 (130.97, 349.6) | 0.57 (0.28, 1.09) | 155.07 (154.41, 155.75) | 0.40 (0.23, 0.61) | |
| Western and central Africa | 1990 | 1.14 (0.95, 1.40) | 5.53 (3.31, 7.95) | 457.74 (287.3, 695.14) | 25.02 (12.98, 45.17) | 954.92 (952.07, 957.79) | 52.86 (31.55, 75.99) |
| 2019 | 1.67 (1.38, 2.04) | 7.88 (4.79, 11.26) | 905.82 (546.35, 1416.35) | 70.56 (35.68, 129.03) | 765.57 (763.9, 767.24) | 60.34 (36.68, 86.16) | |
| Western and central Europe and North America | 1990 | 0.07 (0.06, 0.08) | 0.33 (0.20, 0.48) | 841.69 (701.78, 953.96) | 2.81 (1.62, 4.20) | 225.13 (224.64, 225.62) | 0.75 (0.44, 1.09) |
| 2019 | 0.13 (0.1, 0.15) | 0.62 (0.37, 0.90) | 740.27 (576.86, 898.34) | 4.60 (2.63, 7.09) | 139.74 (139.4, 140.07) | 0.87 (0.52, 1.26) |
- Abbreviations: ASR, age-standardized rate; DALY, disability-adjusted life-years; PAF, population attributable fraction; UNAIDS, Joint United Nations Programme on HIV and AIDS.
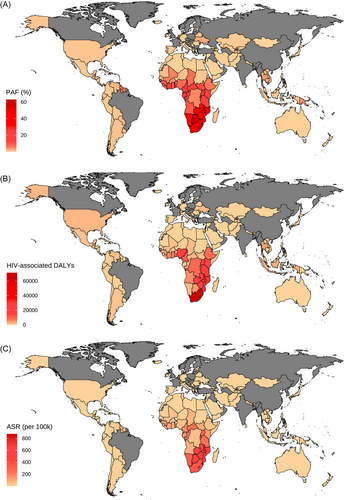
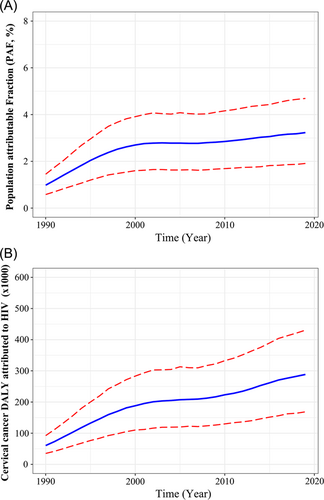
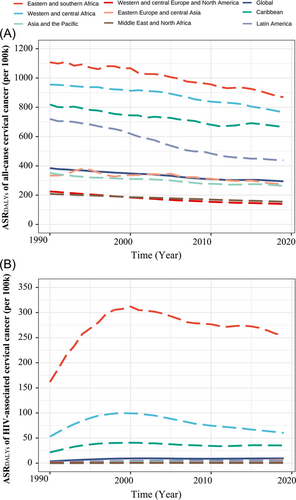
From 1990 to 2019, there was an increase in the global PAF of cervical cancer associated with HIV infection from 0.98% to 3.22% (Table 1 and Figure 2A). The number of DALYs caused by HIV-associated cervical cancer increased by over four times during this period (Table 1 and Figure 2B). the global ASR of all-cause cervical cancer DALYs showed a moderate decline from 384.83 per 100k population in 1990 to 294.7 per 100k population in 2019 (Table 1 and Figure 3A). However, there was an increase in the ASR of HIV-associated cervical cancer DALYs from 3.78 per 100k population in 1990 to 9.50 per 100k population in 2019 (Table 1, Figure 3B and Supporting Information: Figure 1). Over the past three decades, the regions of Eastern and Southern Africa had the highest ASRs of HIV-associated cervical cancer DALYs among the eight regions under the UNAIDS purview (Figure 3A,B). The ASRs of cervical cancer DALYs showed a slight decline in all regions (Figure 3A and Supporting Information: Figure 2). But there was notable regional inequality in the ASRs of HIV-associated cervical cancer DALYs. The Eastern and Southern Africa region, with the highest ASR of HIV-associated DALYs, encountered a sharp rise from 1990 to 2000, followed by a slight reduction in the succeeding two decades (Figure 3B). From 1990 to 2019, Eastern Europe and Central Asia showed a low ASR of HIV-associated DALYs; however, it had the highest increasing trend (EAPC: 14.07%) (Figure 3B and Supporting Information: Figures 1 and 2). We estimated the all-cause and HIV-associated cervical cancer DALYs ASRs and calculated the EAPC over the past 30 years in 134 countries (Figure 4 and Supporting Information: Table 3). Of note, we observed a significant annual increase trend in the HIV-associated cervical cancer DALYs rate in 107 countries, with Tajikistan (EAPC: 32.56%), Pakistan (EAPC: 29.96%), and Georgia (EAPC: 27.16%) having the highest trends (Figure 4 and Supporting Information: Table 3).

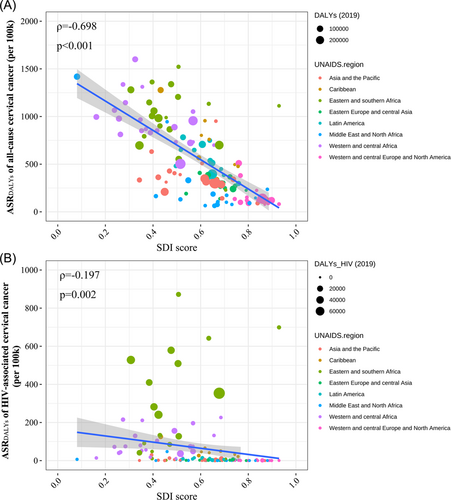
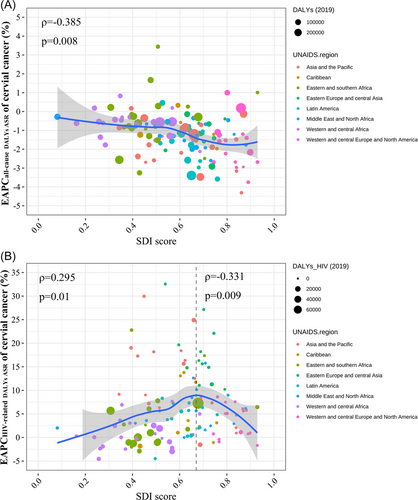
In addition, a significant decrease trend in both all-cause DALYs (ρ = −0.698, p < 0.001) and HIV-associated DALYs (ρ = −0.179, p = 0.002) was observed in correlation with SDI (Figure 5). We utilized Gaussian process regression to investigate the nonlinear relationship between EAPCs and SDI. Our analysis showed a significant negative correlation between EAPCs and SDI (in 2019) for all-cause DALYs (ρ = −0.385, p = 0.008) (Figure 6A). Additionally, we observed an inverted V-shaped correlation between SDI and EAPCs for HIV-associated DALYs. When the SDI was below 0.68, there was a significant positive correlation (ρ = 0.295, p = 0.01), while when the SDI was above 0.68, there was a significant negative correlation (ρ = −0.331, p = 0.009) (Figure 6B).
4 DISCUSSION
This study evaluated the global and regional burden of cervical cancer attributed to HIV/AIDS between 1990 and 2019, based on the RR of cervical cancer in women living with HIV and epidemic data on HIV and cervical cancer provided by the UNAIDS and GBD. Our study estimated a 288 370 (95% CI: 168 310–430 800) DALYs lost in women (≥15 years old) living with HIV in 2019, and a more than fourfold increase during the past 30 years. However, the global HIV-associated cervical cancer burden has large regional differences, with the highest burden observed in the Eastern and southern Africa. Meanwhile, our findings revealed that, from 1990 to 2019, the middle or high-middle SDI countries in the Eastern Europe and Central Asia region experienced the most significant increase in trends.
The epidemics of cervical cancer and AIDS intersect with each other.15 Although not the primary cause of cervical cancer, being HIV-positive increases the risk of acquiring HPV.3, 16, 17 Multiple factors may contribute to the accelerated progression from HPV to cervical cancer as a result of the interaction between HIV and HPV, as suggested by studies.18, 19 For example, HIV infection can promote the acquisition of HPV and hinder its clearance, leading to the persistence of HPV in the cervix and a decreased likelihood of regression of precancerous lesions.20, 21 Furthermore, HIV-induced immunosuppression weakens the immune function, making individuals more vulnerable to HPV and opportunistic infections. This is corroborated by the inverse relationship between markers of HIV control/immune status and the risk of HPV infection.15, 21 Additionally, HIV infection has an impact on the outcomes of cervical cancer. Cohort studies have demonstrated higher rates of recurrence and mortality among cervical cancer patients who are also HIV-positive.22 Despite having good access to ART, HIV lowers the survival rates and worsens the disease burden in regions where HIV and HPV are prevalent.23 Our study found noteworthy variations in the burden of cervical cancer across different regions, with the highest HIV-related DALYs recorded in Eastern and Southern Africa. This is consistent with the findings of Stelzle et al., who reported that women accounted for the majority of cervical cancer cases associated with HIV in Eastern and Southern Africa in 2018.3 Cervical cancer is categorized as an AIDS-defining illness, and it is more prevalent in women living with HIV, particularly in South Africa.24 Studies has reported that more than half of women infected with HIV live in the East and South Africa,25 and a maximum HPV prevalence ~20% in Africa females.26 As a result, the Eastern and Southern Africa region was responsible for nearly 30% of all DALYs related to cervical cancer and attributable to HIV. Both HIV and HPV are significant public health challenges in Africa, and their high prevalence has led to a significant burden of cervical cancer. Cervical cancer can be managed effectively through early prevention and prompt treatment. However, as an inequitable disease, the unequal access to healthcare has resulted in a disproportionate burden of cervical cancer in countries with limited health resources, particularly in low- and middle-income nations.2, 27, 28 Our findings have highlighted an increasingly pressing issue for healthcare policies, guidelines, and resource distribution in the region of Eastern and Southern Africa.
As the most routine preventive measures recommended by the World Health Organization, cervical cancer screening and HPV vaccination are currently progressing step by step.29, 30 Many countries are working to increase the level of screening and vaccine coverage,31 while there are still fewer resources and capacities available to directly address the problem in LMICs with a heavy burden of cervical cancer.1, 32 HPV vaccination as an important tool to prevent cervical cancer, only 96 countries, mainly developed or high-income countries, had introduced the vaccine according to the statistical data by mid-2019.33 Undouble, this has further widened regional inequalities in the burden of cervical cancer associated with HIV. Furthermore, according to the 2019 estimates,32 HPV vaccine program performance was found to be suboptimal in numerous countries, including those with high-income and ample resources. This was evident from the global average, where last dose coverage of the vaccine was only 53% in countries where it was introduced.32 When expressed as coverage of the global population of eligible girls, the estimated final dose HPV coverage was only 15%.32 The variations in the introduction of HPV vaccination across different regions and income levels highlight the persistent disparities in cervical cancer prevention worldwide. Countries with the highest burden of the disease not only face limitations in secondary prevention but also have lower rates of vaccination accessibility,32, 34 leading to an increased imbalance in this global burden. Consequently, further efforts to expand the coverage and vaccination rates in LMICs with a high cervical cancer burden, particularly in Africa, are therefore key priorities. Meanwhile, considering the gradual extension of HIV survival, integrating HIV care with cervical cancer prevention and control help address the global burden of cervical cancer in women living with HPV, particularly in high-burden regions.
Our study made a significant contribution by reporting on the trend of HIV-associated cervical burden over the past three decades. Notably, we found that the Eastern Europe and Central Asia region experienced the most significant increase in this burden. This outcome could be attributed to the rapid rise in HIV infections in the area. According to UNAIDs, there has been a 72% increase in the number of new HIV infections reported between 2010 and 2019, with 1.7 million people living with HIV in the Eastern Europe and Central Asia region.35 Despite the implementation of the UNAIDS “90-90-90” strategy by countries in the Eastern Europe and Central Asia region with the goal of eradicating the AIDS epidemic by 2030, there are numerous factors that could impede its success. These may include a substantial number of people living with HIV, suboptimal adherence to ART, inadequate supply of ART medications and inadequate routine viral load monitoring systems.36, 37 Furthermore, a growing concern in recent years has been the emergence, transmission, and dissemination of drug-resistant (DR) HIV variants, which could contribute to an increase in HIV incidence, mortality rates, and overall expenses related to HIV-associated diseases.38, 39 Nonetheless, data on the prevalence of HIV DR strains is scarce in the countries of the Eastern Europe and Central Asia region due to limited DR testing.40 At present, the majority of countries in the Eastern Europe and Central Asia region are categorized as middle SDI regions and are in the midst of their development stage. These countries are facing a range of significant epidemiological risk factors, low levels of disease awareness, inadequate healthcare funding, and other related challenges.41 Hence, our findings recommend that countries in the Eastern Europe and Central Asia region should remain vigilant and devise efficient strategies to prevent the mounting burden of HIV-related cervical cancer.
5 LIMITATION
We calculated the global, regional, and national burden of HIV-associated cervical cancer, using a traditional epidemiological PAF formula, as previously described.10-12 However, there were several factors that may have impacted the estimated outcomes and are worth discussing.
First, although the overall RR used in this study was based on the latest meta-research by Stelzle et al.,3 it is important to note that there was considerable statistical, regional, and demographic heterogeneity among the included studies. Meanwhile, as the paucity of data from different regions, we make an assumption that the estimated RR was suitable for regions and countries like others studies performed.10-12 Indeed, the estimated RRs may vary for females living with HIV in LMICs compared with high-income countries, based on different potential confounding factors such as CD4 counts, viral loads, lifestyle behaviors, access to healthcare facilities, and socioeconomic factors. For instance, while Bedimo et al. reported a 12.80-fold higher risk, Sekirime et al. found only a 1.26-fold higher risk of cervical cancer in HIV-infected populations in the United States and Uganda, respectively.42, 43 Consequently, our study, which utilized a pooled RR value of 6.07, may have led to an underestimation of the burden of HIV-associated cervical cancer in the United States and an overestimation in Uganda. Additionally, despite Stelzle et al. reporting no significant regional discrepancies in pooled RR values, we observed that the RR in Asia (RR: 16.47; 95% CI: 3.48–77.97) appeared higher compared with other regions (Americas, 8.23; Europe, 5.01; Africa, 3.70). Moreover, it should be noted that we made the assumption that the pooled RR value was applicable for the past 30 years, which led to a conservative interpretation of the estimated trend results. Although Stelzle et al. conducted a sensitivity analysis and discovered no notable variation in pooled RR values between studies included before 2013 (RR: 5.57, 95% CI: 3.42–9.66) and those included in 2013 or later (6.34, 4.19–9.59).3 Unfortunately, due to the very limited or even nonexistent number of literatures on HIV-associated cervical cancer risk in each region, calculating PAF based on the RR values for each region separately faces greater difficulties and heterogeneity.
The second limitation is related to the data sources we used. Specifically, we relied on HIV prevalence data from the UNAIDS HIV estimates and disease burden data from the GBD data set. While these data sets represent the most reliable sources of data available, they may not be entirely accurate for countries with inadequate surveillance systems. Additionally, since the GBD also provides its own estimates for HIV prevalence, we compared the HIV prevalence rates from GBD and UNAIDS in 2019, and found a high degree of consistency between the two sources, with a correlation coefficient of 0.996 (Supporting Information: Figure 3). However, there are still some countries where differences exist between the HIV prevalence rates from GBD and UNAIDS, by longitudinal calendar years (Supporting Information: Figure 4). Therefore, given that UNAIDS HIV prevalence rates are based on real data reported by each country, while GBD estimates are based on modeling, we used UNAIDS as the data source for HIV prevalence rates in this study, consistent with previous research.10, 11, 44
Thirdly, there may be differences in the risk of cervical cancer in patients with advanced HIV disease compared with those with early HIV disease. In our study, the original studies included in our analysis did not report relative HIV stage information. As a result, we were unable to obtain precise RR values for early and advanced stages of HIV, respectively. On the other hand, with the widespread use of HIV ART, the life expectancy of HIV patients has been extended, and their risk of developing cervical cancer has also increased relatively. Therefore, we may have overestimated the association between HIV and cervical cancer.
6 CONCLUSION
This analysis estimated the global burden of HIV-associated cervical cancer in females (≥15 years old). We reported that 3.22% of all cervical cancer cases worldwide were attributable to HIV infection in 2019, and the attributable fractions were increasing from 1990 to 2019. The region of Eastern and Southern Africa was experiencing the greatest burden of HIV-associated cervical cancer, whereas the Eastern Europe and Central Asia region had shown the highest increase trend over the last 30 years. Integrating cervical cancer prevention and HIV prevention would contribute to eliminate the cervical cancer burden and contain the regional disparities.
AUTHOR CONTRIBUTIONS
Zhengwei Wan, Jianhui Zhao, Xue Li, and Yuping Liu designed this analysis and drafted the manuscript. Jianhui Zhao and Zhengwei Wan finished the data extraction, synthesis, and analysis. All authors reviewed the results, commented on the manuscript drafts, and approved the manuscript.
ACKNOWLEDGMENTS
The authors express their gratitude to Wei Guo, the Strategic Information Officer at the UNAIDS Office in China, for providing us with valuable advice on the global AIDS strategy. The authors also extend their appreciation to Keith Sabin, a colleague at the Joint United Nations Programme on HIV/AIDS (UNAIDS) in Geneva, Switzerland, for his assistance in obtaining the global HIV prevalence data. This study was supported by the Science Foundation for Young Scholars of Sichuan Provincial People's Hospital (NO. 2022QN18); the Subject Founds of Health Care for Cadres of Sichuan Province (NO. 2022-220).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the finding of this study are opening available in Joint United Nations Programme on HIV and AIDS (UNAIDS) at https://aidsinfo.UNAIDS.org, and GBD at http://ghdx.healthdata.org/gbd-results-tool.




