Reply to Chan et al.
Abstract
We agree that smoking might be a risk factor for the severity of COVID-19, but in our previous study, smoking was not so robust compared with our conclusion. Also, we strongly agreed that COVID-19 patients with diabetes or other chronic diseases might worsen the situation of the disease. But these factors were out of the scope of our study and we had published other research on this topic related to diabetes. Because of the limited sample size and original medical records, our study could not cover many factors. But we wish our study will be a useful and meaningful pilot study for future studies.
We appreciate the comments from Chan et al. for our study, and agree that many factors may have a significant impact on outcomes in COVID-19 patients, as their comments.
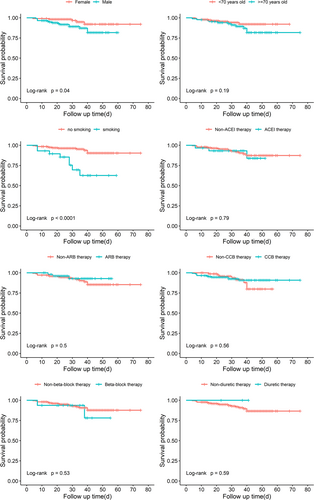
Chan et al. mentioned the negative effects of smoking for the COIVD-19 patients with hypertension. We collected the smoking information in our study. However, 51 patients did not offer clear information about the smoking situation among the total of 278 patients included in our study. As the limited samples, we would like to share the results which take smoking variables only into consideration for the comments. After excluding the patients with uncertain smoking situations, a total of 227 patients are included. Table 1 shows the characteristics of the study samples. Table 2 shows the result of the Cox proportional-hazards model. Compared with the previous result which included a total of 278 patients, we found that age, sex, ARB therapy and CCB therapy are no significant risk factors, and smoking was a significant factor in this small sample. Though the smoking variable is statistically significant, the 95% confidence interval (CI) is wide which exceeds 10, because of the small sample size. Thus, we consider that the result is not so robust. The 95% CI in the previous study (n = 278) is in a smaller range, so we have more confidence convincing that the previous results are more reliable. We also present the Kaplan–Meier curve by sexes, age groups, smoking, and different therapy (n = 227) (Figure 1). And the result is similar to the previous result (n = 278). So, we think the latter result (n = 227) is not so robust compared with the previous result (n = 278) because of the too limited sample sizes. In conclusion, smoking might be a risk factor of the severity of COVID-19 as mentioned by Chan et al., but we may need further studies on this topic.
| Variable | Number (n) | Percent (%) | Number of deaths | Percent (%) |
|---|---|---|---|---|
| Sex | ||||
| Female | 111 | 48.90 | 5 | 4.50 |
| Male | 116 | 51.10 | 14 | 12.07 |
| Age | ||||
| <70 | 142 | 62.56 | 8 | 5.63 |
| ≥70 | 85 | 37.45 | 11 | 12.94 |
| Smoking | ||||
| Yes | 29 | 12.78 | 8 | 27.59 |
| No | 198 | 87.23 | 11 | 5.56 |
| Theraty | ||||
| ACEI | 30 | 13.22 | 3 | 10.00 |
| ARB | 54 | 23.79 | 3 | 5.56 |
| CCB | 148 | 65.20 | 11 | 7.43 |
| Beta-blockers | 16 | 7.05 | 2 | 12.50 |
| Diuretic | 3 | 1.32 | 0 | 0 |
| Nontherapy | 29 | 12.78 | 6 | 20.69 |
| Outcomes | ||||
| Survived | 208 | 91.63 | – | – |
| Death | 19 | 8.37 | – | – |
- Abbreviations: ACEI, angiotensin-converting-enzyme inhibitors; ARB, angiotension II receptor blockers; CCB, calcium channel blockers.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | p value | HR (95% CI) | p value | |
| Sex | ||||
| Female | 1 | 1 | ||
| Male | 2.80 (1.01, 7.77) | 0.048a | 1.73 (0.56, 5.34) | 0.338 |
| Age | ||||
| <70 | 1 | |||
| ≥70 | 1.81 (0.73, 4.58) | 0.078 | ||
| Smoking | ||||
| No | 1 | 1 | ||
| Yes | 5.36 (2.16, 13.3) | <0.01a | 4.24 (1.56, 11.57) | 0.009a |
| Therapy | ||||
| ACEI | 1.18 (0.35, 4.06) | 0.790 | ||
| ARB | 0.65 (0.19, 2.24) | 0.500 | ||
| CCB | 0.76 (0.31, 1.89) | 0.560 | ||
| Beta-blockers | 1.60 (0.37, 6.92) | 0.530 | ||
| Diuretic | NA | NA | ||
- Abbreviations: ACEI, angiotensin-converting-enzyme inhibitors; ARB, angiotension II receptor blockers; CCB, calcium channel blockers; CI, confidence interval.
- a p < 0.05.
Also, we strongly agreed with the opinion of Chan et al. that COVID-19 patients with diabetes or other chronic diseases might worsen the situation of the disease. One of the limitations of our study is that the confounding factor of complications was not considered. Propensity score-matched analysis is a good way to decrease the influence of confounders, but generally it needs a larger sample size. Another published study of us discussed about the relationship between diabetes and COVID-19,1 showing our similar concerns as Chan et al.
As Leishenshan Hospital was an emergency specialty field hospital built in response to the COVID-19 pandemic, the operating duration of the hospital was only 2 months. Because of the limited sample size and original medical records, our study could not cover many factors suggested as Chan et al. But we wish our study will be a useful and meaningful pilot study for the future studies.
AUTHOR CONTRIBUTIONS
Liyang Zhao, and Yusi Li: compiled and analyzed the data. Yusi Li and Ning-Yi Shao: wrote the manuscript. Miao Liu, Sridhar Radhakrishnan, Rui Li, Ruirong Tan, Mengyuan Dai, and Gang Fan: provided the technical and material support. All authors reviewed the manuscript and edited it for intellectual content, and gave final approval for this version to be published.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.




