COVID-19 is associated with bystander polyclonal autoreactive B cell activation as reflected by a broad autoantibody production, but none is linked to disease severity
Abstract
Coronavirus disease 2019 (COVID-19) is associated with autoimmune features and autoantibody production in a small subset of the population. Pre-existing neutralizing antitype I interferons (IFNs) autoantibodies are related to the severity of COVID-19. Plasma levels of IgG and IgM against 12 viral antigens and 103 self-antigens were evaluated using an antibody protein array in patients with severe/critical or mild/moderate COVID-19 disease and uninfected controls. Patients exhibited increased IgGs against Severe acute respiratory syndrome coronavirus-2 proteins compared to controls, but no difference was observed in the two patient groups. 78% autoreactive IgGs and 93% autoreactive IgMs were increased in patients versus controls. There was no difference in the plasma levels of anti-type I IFN autoantibodies or neutralizing anti-type I IFN activity of plasma samples from the two patient groups. Increased anti-type I IFN IgGs were correlated with higher lymphocyte accounts, suggesting a role of nonpathogenic autoantibodies. Notably, among the 115 antibodies tested, only plasma levels of IgGs against human coronavirus (HCOV)-229E and HCOV-NL63 spike proteins were associated with mild disease outcome. COVID-19 was associated with a bystander polyclonal autoreactive B cell activation, but none of the autoantibody levels were linked to disease severity. Long-term humoral immunity against HCOV-22E and HCOV-NL63 spike protein was associated with mild disease outcome. Understanding the mechanism of life-threatening COVID-19 is critical to reducing mortality and morbidity.
Highlights
-
Coronavirus disease 2019 was associated with a bystander polyclonal autoreactive B cell activation reflected by an increased number of plasma autoantibody levels.
-
However, none of the autoantibody levels were associated with disease severity, including anti-type I interferons.
1 INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is the virus that causes the coronavirus disease 2019 (COVID-19). Lymphopenia is associated with disease severity and is commonly observed in SARS-CoV-2-infected patients with severe/critical disease (60%−80%).1-3 Importantly, SARS-CoV-2 infected patients with severe illness were associated with increased levels of SARS-CoV-2-specific IgG during 7−14 days of symptom onset, B cell hyperactivation, and more substantially reduced peripheral lymphocytes compared to patients without severe illness.4-7 However, the mechanism leading to lymphopenia in severe COVID-19 is not entirely understood.
Approximately 18% of healthy women and 11% of healthy men have detectable IgG autoantibodies (IgG antinuclear antibodies or other autoantibodies), and the majority will never develop a clinical autoimmune disease (a significant gender difference).8 Among the positive IgG autoantibodies in healthy individuals, most are naturally occurring and nonpathogenic. Autoantibodies targeting traditional autoantigens or cytokines have been reported following SARS-CoV-2 infection.9 Neutralizing autoantibodies against type I interferon (IFN) have been identified as a risk factor for life-threatening COVID-19, but only shown in approximately 4% of the general population.10-14
In this study, we have conducted an antibody protein array and evaluated antibody levels against 12 viral antigens and 103 host self-antigens in a cross-sectional cohort in healthy controls and two COVID-19-infected patient groups, including severe/critical and mild/moderate clinical course.
2 MATERIALS AND METHODS
2.1 Human subjects
A total of 23 participants were included in the current study, including 8 healthy controls, 5 patients with mild/moderate COVID-19 disease, and 10 patients with severe/critical COVID-19 disease. The definition of patient groups was followed by the WHO Clinical Progression Scale.15 Severe/critical disease included hospitalized patients needing high flow nasal oxygen or mechanical ventilator; mild/moderate disease included symptomatic ambulatory without oxygen need and hospitalized patients receiving oxygen therapy by mask or nasal cannula.16 Patients with severe/critical disease presented with lymphopenia (lymphocyte account below 1.1 × 109/L within 12 days postinfection); patients with mild/moderate disease had lymphocyte account above 1.1 × 109/L within 12 days postinfection. Age-matched individuals were included as controls (healthcare workers recruited locally).
All participants were recruited from the Department of Infectious Diseases, Sahlgrenska University Hospital, Gothenburg, Sweden, between April 21, 2020 and July 17, 2020. This study was approved by the Swedish Ethical Review Authority (Registration number 2020–01771) with informed content obtained from all subjects.16 Table 1 shows the clinical background features of the participants.
| COVID19/severe (n = 10) | COVID19/non-severe (n = 5) | Healthy control (n = 8) | p Value (two patient groups) | |
|---|---|---|---|---|
| Age (years) | 51 (46−66) | 59 (46−68) | 44 (38−55) | 0.74 |
| Sex ratio, male: female | 3:7 | 3:2 | 3:5 | 0.58 |
| Lymphocyte counts | 0.65 (0.60–0.83) | 1.4 (1.30−2.30) | 0.0007 | |
| Approx duration of symptoms until sampling | 8.5 (7.8−10.3) | 8.0 (8.0−10.0) | 0.998 |
- Note: Data are median (25th percentile, 75th percentile);
- Lymphocyte count: ×109/L;
- Severe/lymphopenia: lymphocyte counts below 1.1 × 109/L within 12 days postinfection;
- Nonsevere/normal lymphocyte counts: above 1.1 × 109/L within 12 days postinfection.
2.2 Plasma sample collection
Plasma samples were isolated from fresh blood in EDTA–containing blood collection tubes, aliquoted, and stored at −80°C before use, as previously described.17 The median (interquartile range) days from symptom to sampling were 8.5 (7.8−10.3) and 8.0 (8.0−10.0) for patients with severe/critical COVID-19 disease and patients with mild/moderate disease, respectively.
2.3 Autoantigen microarray
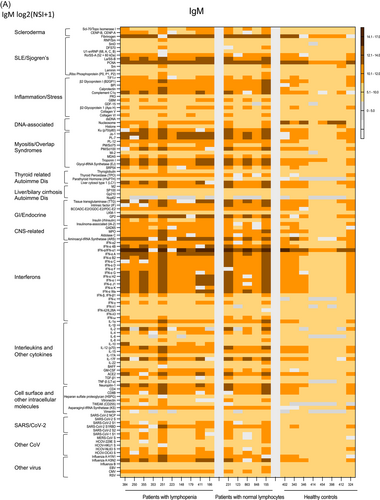
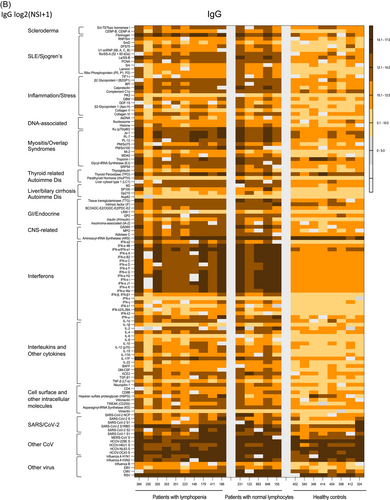
Plasma levels of IgM and IgG antibodies against 12 viral antigens, including SARS-CoV-2, and 103 autoantigens were evaluated by the OmicsArray™ autoantigen protein microarray chip (GeneCopoeia). Each autoantigen is listed in Figure 1. The viral proteins tested for antibody levels included SARS-CoV-2 related antigens, other viral antigens (influenza, EBV, CMV, and RSV) and human coronavirus (HCOV)-229E and HCOV-NL63 antigens. The autoantigens tested for autoantibody levels included autoantibodies associated with scleroderma, SLE, Sjogren's, myositis, thyroid-related autoimmune diseases, liver or biliary cirrhosis autoimmune diseases, GI or endocrine or central nervous system autoimmune diseases, and intercellular or surface self-antigens (i.e., cytokines including IFNs, CD4, and CD8).
Plasma samples were treated with DNase I, diluted to 1:50 and incubated with autoantigens on OmicsArray™ Antigen Microarrays (GeneCopoeia Inc.). Cy3-labeled anti-human IgG (Jackson ImmunoResearch Lab; 1:1000) was used to detect IgG autoantibodies, and the arrays were scanned with a GenePix® 4000B Microarray Scanner (Molecular Device). The images were analyzed using GenePix 7.0 software. The averaged net fluorescent intensity of each autoantigen was normalized to internal Ig controls, and scaling and centering (x—mean[x]) were performed after log2 transformation.
2.4 Neutralizing activity against type I IFN using plasma samples
PBMCs from 4 healthy individuals were cultured with media containing 10% plasma samples obtained from patients with severe disease (n = 4) or mild disease (n = 4) and stimulated with 100 ng/ml of IFN-α-2a (100 ng/ml; Miltenyi Biotec) for 15min. Cells were lysed, and STAT1 protein expression was evaluated by ELISA (RAB0441; Sigma).
2.5 Statistical analysis
The nonparametric Mann−Whitney U tests were applied to compare the differences in continuous measurements in the two groups. In the prespecified hypothesis, we were interested in the comparing of patients versus controls or severe patients versus nonsevere patients; therefore, p values from comparing were not adjusted for multiple comparisons. Spearman correlation tests were applied to explore associations between pairs of continuous variables. All tests were 2-sided, and p values of ≤0.05 were considered statistical significance.
3 RESULTS
3.1 A number of autoantibody productions were increased in COVID-19 patients compared to controls, but none of the autoantibody levels was related to disease severity
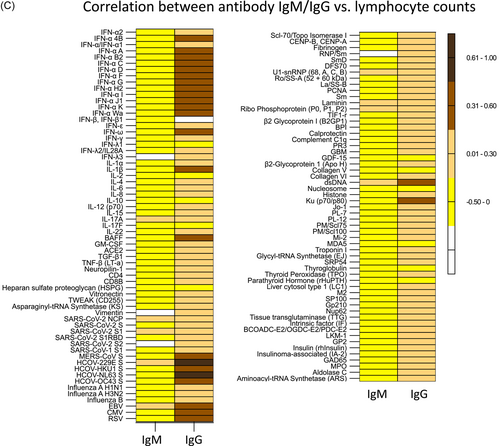
To investigate the associations of autoantibodies and COVID-19 disease severity, we conducted plasma levels of IgG and IgM autoantibodies against 103 self-antigens in humans using an antibody protein array. Although all patient samples were collected 12 days postinfection, IgGs were the main responses but not IgMs (Figure 1A,B). Among the 103 autoantibody IgGs tested, most were increased in patients compared to controls (80/103); none of the autoantibody levels tested differed between patients with severe disease and nonsevere disease (Figure 1B). The low to undetectable plasma levels of IgG in all three groups were IgGs against PR3, parathyroid hormone (rHuPTH), LKM-1, IL-6, and vimentin, and high and similar plasma levels of IgG in the three study groups were IgGs against thyroid peroxidase and aminoacyl-transfer RNA synthetase (Figure 1B).
3.2 Elevated plasma IgG levels against IFNs in COVID-19 patients compared to uninfected controls, but no difference was observed between the two patient groups
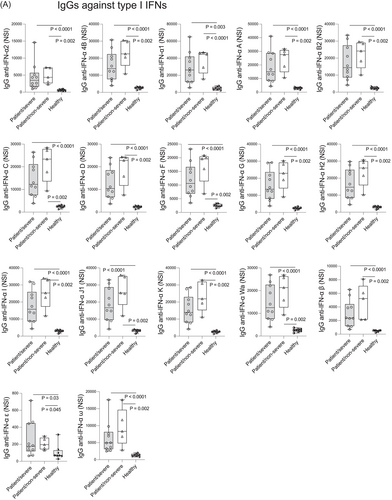
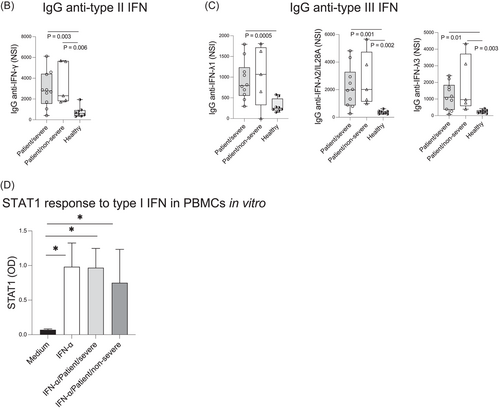
Previous studies showed that pre-existing autoantibodies against type I IFNs were associated with severe COVID-19 disease.10-14 In this cross-sectional study, we evaluated 19 autoantibody IgGs against type I IFNs (IFN-α, IFN-α1, IFN-α2, IFN-α 4B, IFN-α A, IFN-α B2, IFN-α C, IFN-α D, IFN-α F, IFN-α G, IFN-α H2, IFN-α I, IFN-α J1, IFN-α K, IFN-α Wa, IFN-β1, IFN-β, IFN-ε, and IFN-ω, Figures 2A), 1 IgG against type II IFN (IFN-γ, Figure 2B), and 3 IgGs against type III IFNs (IFN-λ1-3, Figure 2C) in the three study groups, patients with severe/critical COVID-19 disease, patients with mild/moderate COVID-19 disease, and uninfected healthy individuals (Figure 2). We found that plasma levels of IgGs against type I, II, and III IFNs tested were increased in patients compared to controls regardless of patient disease severity (Figure 2A−C). Again, similar plasma levels of all anti-IFN IgGs were found between the two patient groups (Figure 2). We evaluated neutralizing activity against type I IFN using plasma samples from patients with or without severe disease outcome in PBMC in vitro, but no significant difference was detected (Figure 2D).
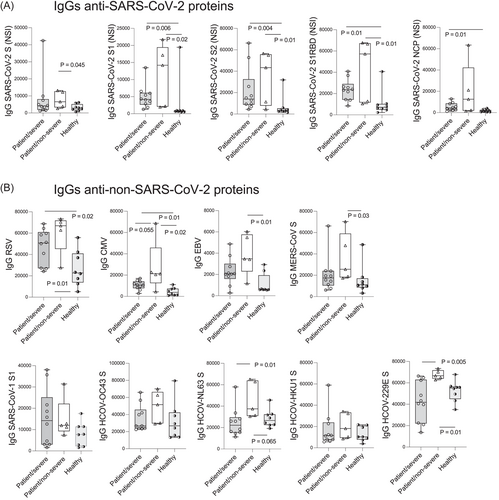
3.3 Plasma levels of IgGs against non-SARS-CoV-2 coronavirus viral protein HCOV-229E S and HCOV-NL63 S, as well as against CMV, were associated with disease severity, whereas IgGs against SARS-CoV-2 viral antigens were not demonstrable to the COVID-19 disease outcome
Consistent with previous studies,4-6, 18 the plasma levels of lgG against SARS-CoV-2 NCP and spike proteins were higher in all patients compared to controls, but they were not associated with disease severity (Figure 3A). We next evaluated the association of disease severity with plasma levels of IgGs against 12 viral antigens. Intriguingly, IgGs against SARS-CoV-2 did not differ in the two-patient group. However, IgGs against other coronavirus proteins HCOV-229E S (p < 0.05) and HCOV-NL63 S (p < 0.05) were higher in patients with mild disease compared with patients with severe disease (Figure 3B). IgGs against CMV were marginally higher in patients with mild disease than patients with severe disease (p = 0.055). Furthermore, we evaluated the correlation between plasma levels of 115 IgMs and IgGs tested and lymphocyte counts in patients. We found that IgGs against HCOV-229E S and HCOV-NL63 S were positively correlated with lymphocyte counts (Figure 3C). These results suggest anti-SARS-CoV-2 antibody levels in plasma samples were not associated with disease outcome, whereas plasma IgG levels against HCOV-229E S and HCOV-NL63 S were negatively associated with disease severity.
4 DISCUSSION
Infectious diseases have long been considered one of the triggers for autoimmune and autoinflammatory diseases. Self-antigen mimicry is the primary mechanism that accounts for infectious disease-mediated autoimmunity.19 Evidence shows that the flare of autoimmune disease or autoimmune features presents following COVID-19 infection.19 Among the autoantibodies reported in COVID-19, pre-existing autoantibodies neutralizing type I IFN are strong determinants of life-threatening COVID-19.10, 13, 14 Consistently, a highly impaired IFN type I response was associated with poor COVID-19 disease outcome.11-14 Among uninfected individuals, ~4% of people above the age of 70 present autoantibodies neutralizing type I IFNs, accounting for ~20% of COVID-19 deaths.12 In agreement with these findings, we also found elevated levels of plasma IgG to type I IFNs in COVID-19 patients compared to uninfected controls. However, we failed to detect a difference in IgGs anti-type I IFN in the two patient groups. The different results between ours and previously published studies may be explained by: (1) the antibody protein array detects antibodies with both high and low affinities, which may account for the different results from ours and previously published results.14 We speculate that the neutralizing IgGs against type I IFN, but not total IgGs against type I IFN, in patient-derived samples may be a critical factor for evaluating its contribution to COVID-19 disease severity. (2) Different patient populations with neutralizing antitype I IFN autoantibodies (~4% uninfected aging population accounts for ~20% of COVID-19 deaths12), different genetic backgrounds (e.g., autoimmune disease genetic background) and susceptibility to generate pathogenic autoantibodies, and (3) pre-existing or infection-induced neutralizing autoantibodies against type I IFN. Nonetheless, the increased plasma levels of IgGs against type I IFNs were correlated with higher lymphocyte counts (Figure 3C), suggesting a role of nonpathogenic autoantibodies.
Because only 4% of people above the age of 70 present neutralizing autoantibodies against type I IFN,12 it seems difficult to conclude that only pre-existing but not infection-induced neutralizing autoantibodies against type I IFN contribute to disease outcomes. Notably, there is no data on the comparison between pre-existing and infection-induced autoantibody neutralizing activity and impact on disease severity. Others and we found that the number of autoantibody productions were increased in patients following COVID-19 compared to uninfected controls (not limited to anti-IFN autoantibodies),9 suggesting that COVID-19 triggers bystander autoreactive B cell activation and various autoantibody production. This is consistent with the reports on infection-mediated polyclonal B cell activation and autoantibody production through breaking self-tolerance and cross-reactivity with host cells. Still, those autoantibodies are present with low affinity and are generally believed nonfunctional. Innate immunity and inflammation can promote autoantibody production nonspecifically.20 Previous studies show that low-affinity nonfunctional autoantibodies can be induced under chronic inflammation conditions.21-24 The development of a pathogenic autoantibody may take many years and undergoes disordered B cell immunoregulation, somatic hypermutation, and class switching with high antigen specificity and affinity, similar to those in autoimmune diseases.25 Notably, no study has revealed a molecular mechanism on COVID-19-induced neutralizing anti-type I IFN antibodies. It remains unknown if the elevated autoimmune disease-associated autoantibodies, besides neutralizing anti-type I IFN antibodies, are determinants for life-threatening COVID-19. Although a recent study reported that plasma exchange treatment efficiently reduced titers of autoantibody against type I IFN and rescued patients with life-threatening COVID-19 pneumonia26; only four patients were in the study, and treatment of dexamethasone and extracorporeal membrane oxygenation may also affect autoantibody levels. It is well known that women are better at producing autoantibodies than men and are at higher risk for most autoimmune diseases. However, there is a sex difference in COVID-19 severity that men tend to be more severe compared to women,27, 28 which may not be explained by autoantibody-mediated COVID-19 severity.
In the current study, the levels of SARS-CoV-2 IgGs did not differ in the two patient groups, nor the 105 autoantibody levels. Previous studies report SARS-CoV-2 specific IgGs do not predict disease protection.4-6 Here, we found that the increased plasma IgG levels against HCOV-229E S and HCOV-NL63 S were associated with protection from severe disease.29 Whether humoral immunity from previous infections of HCOV 229E and NL63 can cross-protect against COVID-19 disease severity deserves further investigations.
Our study has several limitations. The first is the small sample size, preventing us from drawing further conclusions. Second, we utilized the protein array assay to evaluate 115 antibodies which has a limitation that detects antibodies with both high and low affinities. However, neutralizing activity against type I IFN still showed no difference using plasma samples from patients with severe and mild disease outcome. The conflicting results of anti-type I IFN antibodies may stem from differences in neutralizing assays, sample size, and population studied. Nonetheless, we found that broad autoantibody responses were observed in patients with COVID-19 but not in uninfected controls, reflecting polyclonal autoreactive B cell activation; plasma levels of IgGs against HCOV-229E S and HCOV-NL63 S were associated with lower risk of severe disease. Understanding the mechanisms of autoantibodies or viral-specific antibodies attributing to life-threatening COVID-19 will provide potential therapeutic strategies to reduce mortality and morbidity.
AUTHOR CONTRIBUTION
Wanli Xu performed experiments. Wei Jiang wrote the manuscript. Douglas Johnson, Adekunle, Ruth, Hughes Heather, Xiaomei Cong, Xueling Wu, Hongkuan Fan, Lars-Magnus Andersson, Josefina Robertson, Magnus Gisslén, and Wei Jiang were involved in the study design and critically revising the manuscript.
ACKNOWLEDGMENTS
This study was supported by funding from National Institute of Allergy and Infectious Diseases R01 AI128864 (Jiang), National Institutes of Health National Institute of Nursing Research R01NR016928 (Cong), NIH National Institute of General Medical Sciences R25GM072643 (Wright) and R01GM130653 (Fan), R03DA057164 (Jiang), and National Institutes of Health/National Center for Advancing Translational Sciences NIH/NCATS grant UL1TR001450, TL1TR002382 (Adekunle), and UL1TR002378 (TL1 grant, Adekunle), and by the Ralph H. Johnson VA Medical Center Merit Review Award Number CX002422 (Jiang) from the United States (US) Department of Veterans Affairs Office of Research and Development (CSR&D) Service, the VA Southeast Network 7 Research Development Award (RDA, Adekunle), the UConn InCHIP Faculty Seed Grant (Xu), and Oncology Nursing Foundation Research Grant (Xu), as well as the Swedish government and the county councils (ALF agreement ALFGBG-965885, Gisslen), the Swedish Research Council (#2021-06545, Gisslen), and by SciLifeLab from the Knut and Alice Wallenberg Foundation (2020.0182 & 2020.0241, Gisslen).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
Data will be available upon request.




