Prevalence and genotype distribution of human papillomavirus in women with cervical cancer or cervical intraepithelial neoplasia in Henan province, central China
Abstract
To evaluate the prevalence of human papillomavirus (HPV) infection and its genotype among women with cervical lesions in Henan Province, central China. A total of 1317 cervical scrapes from patients with cervical intraepithelial neoplasia 1 (CIN1) (n = 91), CIN2/3 (n = 466), and cervical cancer (CC; n = 760) were collected from 2013 to 2018, and then tested for HPV genotypes using polymerase chain reaction followed by flow-through hybridization assay. The prevalence of HPV was 62.64% for patients with CIN1, 86.91% for patients with CIN2/3%, and 89.21% for patients with CC. In total, the HPV prevalence was 86.56%, and the most common HPV type was HPV16 (58.77%) followed by HPV58 (10.33%), 18 (7.67%), 52 (6.61%), and 33 (5.54%). In this study, the high-risk HPV cumulative attribution rate of nine-valent vaccine coverage was markedly higher than that of bivalent or quadrivalent vaccine coverage in each histopathological category or overall (P < .001). Single HPV infection was the main infection category in each histopathological diagnosis, and the total infection rate was 65.83% (867/1317; P < .001). The prevalence of HPV16 or single HPV infection increased with the severity of cervical lesions (P < .001). HPV16, 58, 18, 52, and 33 may be predominant high-risk factors for cervical lesions in Henan Province. The nine-valent prophylactic HPV vaccine is more effective than a bivalent or quadrivalent vaccine for protecting women from CC in the region.
Highlights
-
This was the largest study to analyze the prevalence and genotype distribution of HPV in women with cervical lesions in Henan Province.
-
HPV16 was the most common genotype in each histopathological category, and HPV52 and 58 were also relatively prevalent.
-
Single infection rather than multiple infections constituted the main infection category.
-
The prevalence of HPV16 or single infection increased with the severity of cervical lesions.
1 INTRODUCTION
Cervical cancer (CC) is leading cancer in females worldwide. In 2012, there were about 527 600 new patients with CC and 265 700 deaths due to CC globally.1 Meanwhile, more than 80% of the women diagnosed with CC and nearly 90% of CC deaths occur in developing countries, such as China, the world's most populous country.1, 2 The CC has become an important public health concern in China.
Epidemiology and basic research have confirmed that human papillomavirus (HPV) infection is the etiologic agent of CC, and approximately 99% of CCs are linked to previous persistent infection with one or more subtypes of HPV.3, 4 More than 200 different HPV genotypes have been characterized to date, and about 40 genotypes could infect the mucosal epithelium of the genital tract.5 Of these, 25 genotypes are grouped into two categories, high-risk HPV (HR-HPV) and low-risk HPV (LR-HPV). HR-HPV is known as oncogenic and LR-HPV generally only causes benign lesions.6
The combination of liquid-based cytology and oncogenic HPV testing is a reliable method to screen women with cytological abnormalities. The screened women are diagnosed by cervical biopsy. Cervical histopathology is considered as the gold standard for the diagnosis of CC and precancerous lesions. Surgery and radiotherapy are the main ways for treatment. To some extent, the detection of HR-HPV may reduce the risk of CC occurrence and associated deaths.7 Detection and genotyping of HPV have become an essential tool for screening, diagnosis, and management of HPV-related CC and its precursor lesions. In recent years, different methods have been developed for detecting HPV genotypes, and some of them have been commercialized and introduced into clinical and research laboratories.
In this study, a polymerase chain reaction (PCR) followed by a flow-through hybridization assay that is capable of detecting 21 HPV genotypes simultaneously was employed. The 21 genotypes include 15 HR-HPV types (16, 18, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, and 68) and 6 LR-HPV types (6, 11, 42, 43, 44, and CP8304).6
It was reported that the distribution of HPV genotypes in CC varies geographically, even in different areas of the same country.6, 8 Although a series of epidemiologic studies about CC or precancerous lesions have been performed to evaluate the prevalence of HPV genotypes in China, such as Zhejiang Province, Chengdu, Changchun, Liaoning Province, Hunan Province, Beijing, and Hong Kong,9-15 fewer were referred to Henan Province, which is a largely agricultural and less developed region located in central China. The aim of the present study is, therefore, to illustrate the prevalence and distribution of HPV genotypes among women with CC or its precursors (cervical intraepithelial neoplasia, CIN) in Henan Province, to provide a theoretical basis for prevention and treatment of CC or CIN.
2 MATERIALS AND METHODS
2.1 Patient selection and sample collection
From March 2013 to December 2018, all patients included in this study were newly diagnosed with CC or CIN in Henan Provincial People's Hospital. Cervical histopathology and HPV testing were performed independently to remove potential reporter bias. The histopathological results were reviewed by a second pathologist who was blinded to the results. Those cases in which the diagnosis of CC or CIN was made by one pathologist but not confirmed by the other, or patients who received immunotherapy or antineoplastic therapy, were excluded. In the end, 43 patients were excluded because histopathological results were not confirmed by the second pathologist, and 105 patients were excluded because they had previously received treatment. For patients included, the cervical exfoliated cells for HPV genotyping were collected before treatment by experienced gynecologists at the lesion site using cytobrush (Chaozhou Hybribio Limited Corporation, Chaozhou, China) according to the manufacturer's instructions. The exfoliated cells were immediately placed in a sterile tube containing 3.5 mL sample preservation fluid and stored at 4℃. The HPV genotyping was done within 24 hours.
All the specimens and their corresponding clinical information were obtained under protocols approved by the Ethics Committee of the hospital, and informed consent for the study was granted.
2.2 DNA extraction and PCR amplification
After shaking, 600 μL specimens were moved into a 1.5 mL centrifuge tube. The supernatants were removed by centrifugation at 13 000 rpm for 5 minutes and the pellets were collected for DNA extraction. Genomic DNA was extracted by boiling lysis using a DNA extraction kit (Chaozhou Hybribio Limited Corporation) according to the manufacturer's procedures. The quality of the extracted DNA was confirmed by amplifying the β-globin gene as an internal control. The HPV DNA that was present in the sample was amplified using the PCR kit (Chaozhou Hybribio Limited Corporation), which utilized biotin-labeled consensus PCR primers PGMY09/PGMY11 to amplify the HPV L1 gene. PCR was carried out in 25 μL reaction mixture for each sample by Life Express Thermal Cycler (Hangzhou Bioer Technology Limited Corporation, Hangzhou, China). The PCR parameters as follows: initial denaturation at 95℃ for 9 minutes, followed by 40 cycles at 95℃ for 20 seconds, 55℃ for 30 seconds, and 72℃ for 30 seconds, and a final extension at 72℃ for 5 minutes. Distilled water and HPV18 were presented separately as a negative and positive control.
2.3 HPV hybridization and signal detection
HPV genotyping was detected by flow-through hybridization and gene chip by HybriMax (Chaozhou Hybribio Limited Corporation) according to the manufacturer's instructions. To detect HPV genotype-specific oligonucleotides, microarray hybridization was performed using a nylon membrane on which HPV genotype-specific oligonucleotide probes were immobilized. The denatured PCR products were hybridized at 45℃ for 10 minutes on such chips placed on the platform of a hybridization chamber. After blocking with confining fluid, the chips were incubated at 25℃ for 3.5 minutes by the addition of streptavidin-alkaline phosphatase, which binds to the biotinylated PCR products. After washing four times, the chromogenic substrate nitroblue tetrazolium and 5-bromo-4-chloro-3-indolyl phosphate were added at 36℃ for 5 minutes, followed by four times washing. The final results were detected by colorimetric change on the chip under direct visualization.
2.4 Statistical analysis
Each HPV type was evaluated independently of all others, and thus type-specific HPV prevalence included that in single and multiple infections. SPSS version 23.0 (IBM, Armonk, NY) was used for statistical analysis. The χ2 test was used to compare the prevalence of HPV infection and the percentage of cases in different age groups. The mean age was presented with  ± SD and that in the different histopathological categories was compared by t test. All the P values were two-sided, and a P < .05 was considered statistically significant.
± SD and that in the different histopathological categories was compared by t test. All the P values were two-sided, and a P < .05 was considered statistically significant.
3 RESULTS
3.1 Prevalence of HPV and HR-HPV in patients with CIN or CC
In total, 1317 patients were included in this study from March 2013 to December 2018. Among them, 91 had CIN1, 466 had CIN2/3, and 760 had CC (Table 1). The 760 CC cases included 698 cases of squamous carcinoma, 53 cases of adenocarcinoma, and 9 cases of adenosquamous carcinoma. The total prevalence of HPV and HR-HPV was 86.56% and 86.03%, respectively. The HPV prevalence in patients with CIN1 (62.64%) was lower than that of CIN2/3 (86.91%) or CC (89.21%), whereas the difference was nonsignificant between CIN2/3 and CC (CIN1 vs CIN2/3, χ2 = 31.706, P < .001; CIN1 vs CC, χ2 = 48.745, P < .001; CIN2/3 vs CC, χ2 = 1.484, P = .223). In the same manner, the HR-HPV prevalence in patients with CIN1 (61.54%) was lower than that of CIN2/3 (86.05%) or CC (88.95%), whereas no difference existed between CIN2/3 and CC (CIN1 vs CIN2/3, χ2 = 31.057, P < .001; CIN1 vs CC, χ2 = 50.759, P < .001; CIN2/3 vs CC, χ2 = 2.269, P = .132).
| HPV type | CIN1 (n = 91) | CIN2/3 (n = 466) | CC (n = 760) | Total (n = 1317) | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| High risk | 56 (39 + 17)a | 61.54 | 401 (288 + 113) | 86.05 | 676 (533 + 143) | 88.95 | 1133 (860 + 273) | 86.03 |
| 16 | 12 (8 + 4) | 13.19 | 242 (170 + 72) | 51.93 | 520 (401 + 119) | 68.42 | 774 (579 + 195) | 58.77 |
| 18 | 4 (1 + 3) | 4.40 | 24 (15 + 9) | 5.15 | 73 (55 + 18) | 9.61 | 101 (71 + 30) | 7.67 |
| 31 | 3 (1 + 2) | 3.30 | 28 (15 + 13) | 6.01 | 25 (14 + 11) | 3.29 | 56 (30 + 26) | 4.25 |
| 33 | 4 (2 + 2) | 4.40 | 40 (22 + 18) | 8.58 | 29 (8 + 21) | 3.82 | 73 (32 + 41) | 5.54 |
| 35 | 2 (1 + 1) | 2.20 | 4 (4 + 0) | 0.86 | 3 (1 + 2) | 0.39 | 9 (6 + 3) | 0.68 |
| 39 | 0 | 0 | 13 (1 + 12) | 2.79 | 12 (2 + 10) | 1.58 | 25 (3 + 22) | 1.90 |
| 45 | 1 (0 + 1) | 1.10 | 2 (1 + 1) | 0.43 | 10 (7 + 3) | 1.32 | 13 (8 + 5) | 0.99 |
| 51 | 8 (6 + 2) | 8.79 | 11 (3 + 8) | 2.36 | 2 (0 + 2) | 0.26 | 21 (9 + 12) | 1.59 |
| 52 | 11 (7 + 4) | 12.09 | 40 (14 + 26) | 8.58 | 36 (14 + 22) | 4.74 | 87 (35 + 52) | 6.61 |
| 53 | 7 (2 + 5) | 7.69 | 10 (3 + 7) | 2.15 | 16 (0 + 16) | 2.11 | 33 (5 + 28) | 2.51 |
| 56 | 3 (3 + 0) | 3.30 | 8 (3 + 5) | 1.72 | 4 (1 + 3) | 0.53 | 15 (7 + 8) | 1.14 |
| 58 | 10 (8 + 2) | 10.99 | 69 (34 + 35) | 14.81 | 57 (20 + 37) | 7.50 | 136 (62 + 74) | 10.33 |
| 59 | 0 | 0 | 4 (0 + 4) | 0.86 | 5 (2 + 3) | 0.66 | 9 (2 + 7) | 0.68 |
| 66 | 4 (0 + 4) | 4.40 | 14 (3 + 11) | 3.00 | 15 (6 + 9) | 1.97 | 33 (9 + 24) | 2.51 |
| 68 | 0 | 0 | 4 (0 + 4) | 0.86 | 12 (2 + 10) | 1.58 | 16 (2 + 14) | 1.21 |
| Low risk | 6 (1 + 5) | 6.59 | 32 (4 + 28) | 6.87 | 43 (2 + 41) | 5.66 | 81 (7 + 74) | 6.15 |
| 6 | 1 (0 + 1) | 1.10 | 6 (1 + 5) | 1.29 | 10 (1 + 9) | 1.32 | 17 (2 + 15) | 1.29 |
| 11 | 2 (0 + 2) | 2.20 | 7 (1 + 6) | 1.50 | 15 (1 + 14) | 1.97 | 24 (2 + 22) | 1.82 |
| 42 | 0 | 0 | 1 (0 + 1) | 0.21 | 1 (0 + 1) | 0.13 | 2 (0 + 2) | 0.15 |
| 43 | 0 | 0 | 3 (0 + 3) | 0.64 | 0 | 0 | 3 (0 + 3) | 0.23 |
| 44 | 0 | 0 | 3 (0 + 3) | 0.64 | 0 | 0 | 3 (0 + 3) | 0.23 |
| CP8304 | 3 (1 + 2) | 3.30 | 14 (2 + 12) | 3.00 | 17 (0 + 17) | 2.24 | 34 (3 + 31) | 2.58 |
| Any type | 57 (40 + 17) | 62.64 | 405 (292 + 113) | 86.91 | 678 (535 + 143) | 89.21 | 1140 (867 + 273) | 86.56 |
- Note: The multiple infections of HR-HPV contained HR + HR and HR + LR, whereas the multiple infections of LR-HPV only contained HR + LR because LR + LR did not exist.
- Abbreviations: CC, cervical cancer; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus; HR, high risk; LR, low risk.
- a The total number of cases (number of single infection + number of multiple infections).
3.2 Distribution of HPV genotypes in patients with CIN or CC
Table 1 lists the detection results of HPV genotypes. All of the 21 different HPV genotypes were detected in the samples. HR-HPV genotypes, rather than LR-HPV types, were common in each histopathological diagnosis. In the 91 patients with CIN1, the top five genotypes were HPV16 (13.19%), 52 (12.09%), 58 (10.99%), 51 (8.79%), and 53 (7.69%). The leading genotypes in the 466 patients with CIN2/3 were HPV16 (51.93%), 58 (14.81%), 33/52 (both of which occurred at a rate of 8.58%), 31 (6.01%), and 18 (5.15%); whereas the top five genotypes in the 760 patients with CC were HPV16 (68.42%), 18 (9.61%), 58 (7.50%), 52 (4.74%), and 33 (3.82%). Overall, HPV16 (58.77%) was the most prevalent HPV type, followed by HPV58 (10.33%), 18 (7.67%), 52 (6.61%), and 33 (5.54%). The prevalence of HPV16 was the highest in each histopathological category, and it was positively associated with the severity of cervical lesions ( χ2 = 116.200, P < .001).
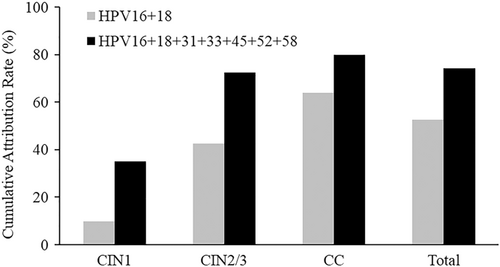
3.3 Cumulative attribution rates of HPV vaccine coverage in patients with CIN or CC
To date, three types of prophylactic HPV vaccines, the bivalent vaccine (which targets HPV16 and 18), the quadrivalent vaccine (which prevents HPV6, 11, 16, and 18), and the nine-valent vaccine (which covers HPV6, 11, 16, 18, 31, 33, 45, 52, and 58), have been developed in other countries and are available in China.
The cumulative attribution rates of HR-HPV types covered by the HPV vaccine are featured in Figure 1. The HR-HPV types targeted by the bivalent or quadrivalent vaccine (HPV16 and 18) attributed to 9.89% of CIN1, 42.49% of CIN2/3, 63.95% of CC, and 52.62% of all cases. In comparison, the HR-HPV types targeted by the nine-valent vaccine (HPV16, 18, 31, 33, 45, 52, and 58) attributed to 35.16% of CIN1, 72.53% of CIN2/3, 80.00% of CC, and 74.26% of all cases. The HR-HPV cumulative attribution rate of nine-valent vaccine coverage was markedly higher than that of bivalent or quadrivalent vaccine coverage in each histopathological category or total (9.89% vs 35.16%, χ2 = 16.654, P < .001; 42.49% vs 72.53%, χ2 = 86.062, P < .001; 63.95% vs 80.00%, χ2 = 48.544, P < .001; 52.62% vs 74.26%, χ2 = 133.000, P < .001).
3.4 Correlation of single or multiple HPV infections with the severity of cervical lesions
Table 2 summarizes the prevalence of single and multiple HPV infections according to histopathological grade. Single infection was the main infection category in each histopathological diagnosis, and the total infection rate was 65.83% (867/1317) (43.96% vs 18.68%, χ2 = 13.513, P < .001; 62.66% vs 24.25%, χ2 = 139.900, P < .001; 70.39% vs 18.82%, χ2 = 409.100, P < .001; 65.83% vs 20.73%, χ2 = 545.700, P < .001). Furthermore, the prevalence of single infection increased with more advanced cervical lesions ( χ2 = 28.478, P < .001). Multiple infections were detected in 273 samples (20.73%, 273/1317), comprising two to five genotypes, and dual infections were predominant (data not listed, P < .05). Our results showed that multiple infections were not associated with the severity of cervical lesions ( χ2 = 5.439, P = .066). Moreover, the prevalence of multiple infections in patients with CC was lower than that of CIN2/3 (CC vs CIN2/3, χ2 = 5.162, P = .023).
| Infection category | CIN1 | CIN2/3 | CC | Total |
|---|---|---|---|---|
| Single infection, n (%) | 40 (43.96%) | 292 (62.66%) | 535 (70.39%) | 867 (65.83%) |
| Multiple infections, n (%) | 17 (18.68%) | 113 (24.25%) | 143 (18.82%) | 273 (20.73%) |
| Total no. | 91 | 466 | 760 | 1317 |
- Abbreviations: CC, cervical cancer; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus.
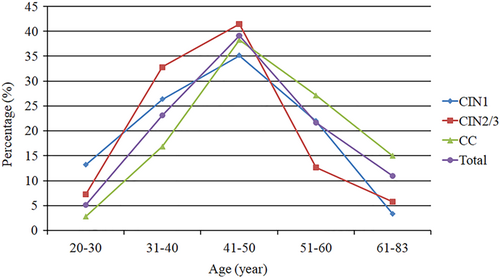
3.5 Distribution of CIN and CC in different age groups and their HPV prevalence
The ages of the 1317 patients with CIN or CC ranged from 20 to 83 years, and the mean age was 46.77 ± 10.70 years. Separately, the mean age was 43.12 ± 10.10 years (range, 20-69 years) in the patients with CIN1, 43.40 ± 9.67 years (range, 20-73 years) in the patients with CIN2/3, and 49.28 ± 10.69 years (range, 21-83 years) in the patients with CC. The mean age of the patients with CC exceeded that of the patients with CIN1 or CIN2/3 (CC vs CIN1, t = 5.225, P < .001; CC vs CIN2/3, t = 9.925, P < .001).
These patients were divided into five age groups (20-30, 31-40, 41-50, 51-60, and 61-83 years). As seen in Table 3 and Figure 2, the 41 to 50 years group was the largest population in each histopathological category or total, with a total number of 516 patients in this group (39.18%, 516/1317). CIN1 or CIN2/3 was least common in the 61 to 83 years group (the oldest); for CC and for the total patient population, the fewest cases were distributed in the 20 to 30 years group (the youngest). The 61 to 83 years group exhibited the lowest HPV-positive rate in each histopathological category or total; the 20 to 30 years group exhibited the highest HPV-positive rate for patients with CIN1, CIN2/3, or total; the 31 to 40 years group exhibited the highest HPV-positive rate of CC.
| Age, y | CIN1 (n = 91) | CIN2/3 (n = 466) | CC (n = 760) | Total (n = 1317) | ||||
|---|---|---|---|---|---|---|---|---|
| n | HPV-positive (%) | n | HPV-positive (%) | n | HPV-positive (%) | n | HPV-positive (%) | |
| 20-30 | 12 | 91.67 (11/12) | 34 | 94.12 (32/34) | 21 | 90.48 (19/21) | 67 | 92.54 (62/67) |
| 31-40 | 24 | 79.17 (19/24) | 153 | 88.24 (135/153) | 128 | 92.97 (119/128) | 305 | 89.51 (273/305) |
| 41-50 | 32 | 46.88 (15/32) | 193 | 84.46 (163/193) | 291 | 90.38 (263/291) | 516 | 85.47 (441/516) |
| 51-60 | 20 | 55.00 (11/20) | 59 | 93.22 (55/59) | 206 | 89.32 (184/206) | 285 | 87.72 (250/285) |
| 61-83 | 3 | 33.33 (1/3) | 27 | 74.07 (20/27) | 114 | 81.58 (93/114) | 144 | 79.17 (114/144) |
- Abbreviations: CC, cervical cancer; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus.
4 DISCUSSION
This study examined the prevalence and genotype distribution of HPV infection in women with CC or precancerous lesions in Henan Province, China, and the results provided HPV epidemiological data concerning cervical lesions in this region. The results showed that HPV prevalence was 62.64% for CIN1, 86.91% for CIN2/3%, and 89.21% for CC. In similar studies, the findings from Zhejiang Province were 73.3% for CIN1, 88.4% for CIN2/3%, and 95.0% for CC9; and from Liaoning Province were 70.56% for CIN1, 89.56% for CIN2/3%, and 82.84% for CC.12 In this study, the HPV prevalence for CIN1 was lower than that in Zhejiang or Liaoning Province, whereas the prevalence for CIN2/3 was similar to that in these two provinces. The HPV prevalence for CC in Henan Province was lower than that in Zhejiang Province but higher than that in Liaoning Province. Our research also showed that HPV prevalence in CC or CIN2/3 was higher than that in CIN1, which was in agreement with that in Zhejiang and Liaoning Province, indicating the known concept: HPV persistent infection plays a key role in the development of CC or CIN2/3.
As shown in this study, the leading genotypes in descending order of prevalence were HPV16, 52, 58, 51, and 53 for CIN1; HPV16, 58, 33/52, 31, and 18 for CIN2/3; and HPV16, 18, 58, 52, and 33 for CC. Reportedly,9, 10, 12, 14, 16, 17 HPV16 was the most common genotype in each histopathological category. This study showed that HPV16 infections were present in over 50% of CIN2/3 cases, CC cases, or all cases. The study furthermore found that the prevalence of HPV16 increased with the severity of cervical lesions, as per the report from Liaoning Province.12 Besides, the results suggested that HPV18 was the second most prevalent HPV type in patients with CC but not common in patients with CIN, and this resembles other findings.9, 12, 15, 18 The reason may be that HPV18 is more likely to cause CC than other high-risk HPV types.19 More attention should be paid to the poorly understood pathogenesis of HPV18. In addition, HPV52 and 58 were prominent in this study, ranking among the top four genotypes in each histopathological category.
Meta-analyses have confirmed that HPV16 and 18 are the two most prevalent HPV types among Asian women with CC, with a higher proportion of HPV52 and 58 among patients with CC from eastern and southeastern Asia compared with other geographical regions.20, 21 In this study, HPV16 and 18 were the top two HPV types among 760 patients with CC, accounting for 68.42% and 9.61% respectively, followed by HPV58 and 52. In many studies in China, the leading two HPV genotypes in patients with CC were HPV16 and 18, with a high prevalence of HPV52 and 58.9, 11, 12, 15, 22 In some regions, however, such as Chengdu, Hunan Province, and Beijing,10, 13, 14 HPV18 ranked third or fourth in descending order of prevalence among patients with CC. The difference can be mainly explained by the geographical variations in the distribution of HPV genotypes.
There were two studies on HPV epidemiology in Henan Province. In a study of 4033 general women,23 PCR and flow-through hybridization assay were used to detect 23 HPV types (6, 11, 16, 18, 31, 33, 35, 39, 42, 43, 45, 51, 52, 53, 56, 58, 59, 66, 68, 73, 82, 83, and CP8304). In this study, the top three genotypes were HPV16, 52, and 58, which was similar to that in CIN1 or CIN2/3 but was different from CC in our study. In another study of 300 women with cervical abnormalities,24 26 HPV types (6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 44, 45, 51, 52, 53, 55, 56, 58, 59, 61, 66, 68, 73, 82, and 83) were tested with Luminex xMAP technology. From this report, the most common HPV genotypes were HPV52, 16, 58, 6, and 39 in low-grade squamous intraepithelial lesions (equivalent to CIN1); HPV16, 33, 58, 18, and 51 in high-grade squamous intraepithelial lesions (including CIN2 and CIN3); and HPV16, 18, 33, 58, and 52 in CC. For precancerous lesions, our results were different from this. But for CC, our results were similar to this except the order of HPV33, 52, and 58. The differences among those studies may be explained by the size and characteristics of the study populations, different methods of HPV genotyping, HPV types detected.
Vaccines against HPV are a promising means of reducing the CC and CIN incidence in a cost-effective manner. This study showed that the HR-HPV cumulative attribution rate of the nine-valent vaccine coverage was markedly higher than that of the bivalent or quadrivalent vaccine coverage in each histopathological category or total. The nine-valent vaccine is more effective than the bivalent or quadrivalent vaccine at protecting women in Henan from CC. In this study, the prevalence of HPV45, targeted by the nine-valent vaccine, was relatively low in CIN1 (1.10%), CIN2/3 (0.43%), or CC (1.32%). According to relevant reports, HPV45 has not been frequently observed in women with CIN or CC in many regions of China, except the Inner Mongolia Autonomous Region.9, 12-14, 22, 25 Among HR-HPV types targeted by the nine-valent vaccine, HPV45 is not as important as the other HR-HPV types in many regions of China.
Herein, this study demonstrated that single HPV genotype infection was the most common infection category, accounting for approximately two thirds (65.83%) of all cases. For CC, single infection affected 70.39% of patients (535/760). Many studies have confirmed a single infection to be the main infection category for patients with cervical lesions.9, 11-15, 24 Our data indicated that the prevalence of single infection rather than multiple infections were associated with the severity of cervical lesions. Currently, consensus is lacking within the literature regarding the association between single or multiple HPV infections and the development of cervical carcinomas. Some studies are consistent with our results.9, 12, 18 By contrast, other studies have reflected the relationship between multiple HPV infections and the severity of cervical lesions.14, 26, 27 In a survey investigating multiple HPV infections in patients with CC, Lee et al28 revealed that individuals infected with multiple HR-HPV types had a 31.8-fold higher risk of CC, whereas patients with a single HPV infection had only a 19.9-fold increased risk. These differences may have been caused by the different populations and methods involved in different studies. Additional studies should be conducted to determine the relationship between multiple HPV infections and the development of cervical lesions.
In this study, the mean age of patients with CC was 49.28 ± 10.69 years, older than that of patients with CIN1 or CIN2/3. This is because the development from CIN to CC takes years. As seen in Figure 2, the distribution of patients for different age groups presented in an inverted “V”; the largest population was in the 41 to 50 years group for each histopathological category or total, and the fewest cases were distributed within the 20 to 30 years range (the youngest) or the 61 to 83 years range (the oldest). Wang et al13 reported that CC was most common between the ages of 41 and 50 years and least common between the ages of 21 and 30 years, in agreement with our study. The reason for this phenomenon may be that it takes 8 to 12 years for young women, who have a higher HPV prevalence because of their more active sex lives, to develop CC.29 Early sex education for young people in Henan Province should, therefore, be enhanced, with CC screening centered on older women. With regard to HPV-positive rates in different age groups, the differences were nonsignificant in all histopathological categories or total.
This study had several limitations. First, the samples were not biopsies but cytological scrapes, in which cells are less concentrated than in histological sections. Second, some HPV types may not have been included in the 21 types and remained undetected. Third, the number of individuals with CIN1 in the study was relatively small, because CIN1 is difficult to screen. This may have resulted in a poor representation of HPV infection status in CIN1. Finally, no further HPV typing was conducted related to the histological subtypes of squamous cell carcinoma, adenocarcinoma, adenosquamous carcinoma, or other rare carcinomas in the cervix, and therefore the associations of type-specific HPV infections with different histological subtypes were not identified.
5 CONCLUSIONS
In summary, this was the largest study to analyze the prevalence and genotype distribution of HPV in women with cervical lesions in Henan Province. HPV prevalence in this region for CIN1, CIN2/3, and CC was 62.64%, 86.91%, and 89.21%, respectively. HPV16 was the most common genotype in each histopathological category, and HPV52 and 58 were also relatively prevalent. Single infection rather than multiple infections constituted the main infection category. The prevalence of HPV16 or single infection increased with the severity of cervical lesions. In addition, the nine-valent vaccine could offer women in Henan greater protection from CC than the bivalent or quadrivalent vaccine could. This study provides basic information concerning the prevalence and genotype of HPV in cervical lesions in Henan Province, Central China.
ACKNOWLEDGMENTS
This study was supported by the National Nature Science Foundation of China (81802094); Medical Science and Technology Research of Henan Province (201602231).
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.




