Hand-assisted laparoscopic left hepatectomy: how I do it
Abstract
Laparoscopic liver resection has been adopted slowly due to concerns for bleeding and oncologic outcomes. Currently, over 9,500 laparoscopic liver resections have been performed and reported worldwide. Numerous studies have shown the safety and oncologic equivalence of laparoscopic liver resection when compared to open resection. Pure laparoscopic and hand-assisted laparoscopic liver resection are the two most commonly used techniques for minimally invasive liver resection surgery. Advantages of the hand-port include tactile feedback, facilitation of liver mobilization, and ease of ability to control bleeding. We present a case report with video of a hand-assisted laparoscopic left liver resection for a hepatocellular carcinoma in a non-cirrhotic patient.
Introduction
Laparoscopic surgery has become the standard approach in many surgical fields. Laparoscopic liver resection has been adopted slowly due to concerns for bleeding and oncologic outcomes. Currently, over 9,500 laparoscopic liver resections have been performed and reported worldwide 1. Numerous studies have shown the safety and oncologic equivalence of laparoscopic liver resection when compared to open resection 2-9. Pure laparoscopic and hand-assisted laparoscopic liver resection are the two most commonly used techniques for minimally invasive liver resection surgery. Advantages of the hand-port include tactile feedback, facilitation of liver mobilization, and ease of ability to control bleeding. Also, when doing a large parenchymal resection, the hand-port can be comparable in size to the extraction port used in the purely laparoscopic approach. The hand-assisted approach can be ideal for surgeons beginning the transition to laparoscopic liver resection and for more experienced laparoscopic HPB surgeons doing laparoscopic major hepatectomies or as an alternative to conversion to open surgery 10, 11. In the associated video (Video S1), we show our technique for hand-assisted laparoscopic left hepatectomy.
Case report
A 72-year-old, otherwise health female, presented with persistent epigastric and right upper quadrant pain that radiated to her back. Four months earlier the patient had complained of the same pain and was found to have gallstones on ultrasound. She underwent an uneventful laparoscopic cholecystectomy, however, the pain persisted. She underwent a CT scan that revealed a 10 × 8 cm heterogeneous, hypervascular mass in the left hepatic lobe. The mass was compressing, but not invading the left portal vein. The mass was also abutting the left hepatic artery, pancreas and stomach without any evidence of invasion. The patient underwent a percutaneous biopsy that showed moderately differentiated hepatocellular carcinoma (HCC). The patient had no history of hepatitis, jaundice, cirrhosis or morbid obesity. There was no evidence of cirrhosis or portal hypertension on imaging. The diagnosis was felt to be cryptogenic HCC. She underwent a hand-assisted laparoscopic left hepatectomy and was discharged home on POD 3. The final pathology revealed a 14 cm hepatocellular carcinoma with areas of focal necrosis and vascular invasion. The margins were negative for tumor and the background liver was normal without signs of fibrosis or cirrhosis (Fig. 1).

Operative technique
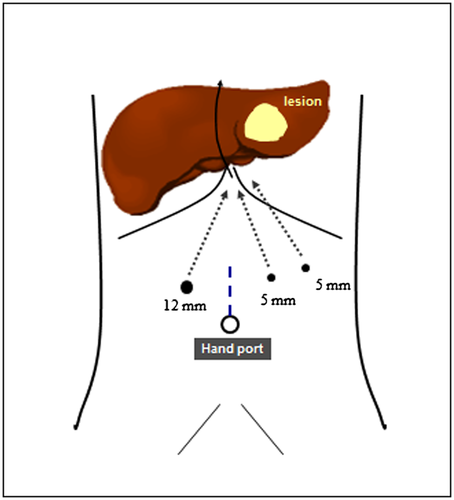
The patient was placed supine with both arms out at 60 degrees. A 5 cm midline incision was made just above the umbilicus and a gel hand port was placed. A 12 mm trocar was inserted through the gel port and used for insufflation. Then a right upper quadrant 12 mm trocar and two left upper quadrant 5 mm trocars were placed (Fig. 2). The large left-sided tumor is stuck to the omentum and this is first taken down. Adhesiolysis was performed to free the left lobe tumor from the abdominal wall. The falciform and left coronary ligaments were then divided to allow for mobilization of the left hemiliver. The left liver was then freed from the caudate lobe by opening up Arantius ligament. Hilar dissection was begun with isolation of the left hepatic artery. This was clipped with a combination of hemolock and metal clips and then divided sharply. The left portal vein was then isolated. Normally the left portal vein would be transected with a vascular stapler load at this point. However, this was a difficult angle and the left hepatic artery was taken after parenchymal transection. In order to minimize bleeding during parenchymal transection, a bulldog clamp was placed around the left portal vein. Next, rigid laparoscopic ultrasound was used to confirm flow in the right portal vein. Ultrasound was also used to scan the right liver for any other tumors. When this was found to be negative, attention was turned to delineating the transection plane. The liver parenchyma was scored with electrocautery to divide the parenchyma. The first few centimeters of the parenchymal transection were accomplished with ultrasonic energy device. The tissue link device was used to obtain hemostasis. Vascular staple loads were then used to take the remainder of the parenchyma including the left hepatic vein branches and the left portal vein (not shown in the video). The left hepatic duct was taken within the parenchyma. The gel hand port was opened to deliver the hepatic lobe. The specimen was sectioned on the back table to confirm gross negative margins. On final pathology, all margins were negative with the closest distance to tumor being 2 cm from the tumor. The underlying liver was not cirrhotic or fibrotic.
Conflict of interest
None declared.