Outcomes after resection of occupational cholangiocarcinoma
Abstract
Background
Cholangiocarcinoma caused by exposure to 1,2-dichloropropane and/or dichloromethane is recognized as occupational cholangiocarcinoma. The aim of this study was to investigate the outcomes after resection of occupational cholangiocarcinoma to establish a treatment strategy for this disease.
Methods
Clinicopathological findings and outcomes after surgical intervention in 20 patients with occupational cholangiocarcinoma were investigated.
Results
Of 20 the patients, curative resection was performed in 16 patients. Three patients underwent radiation at the stump of the bile ducts. Adjuvant chemotherapy was performed in 12 patients. Biliary intraepithelial neoplasia, intraductal papillary neoplasm of the bile duct, and/or chronic bile duct injury was detected in most subjects. Intraabdominal infection developed after surgery in nine patients. Cholangiocarcinoma recurred in 12 of the 20 patients. The recurrent tumors in five patients developed at a different part of the bile duct from the primary tumor and a second resection was performed in four of these five patients.
Conclusions
The incidence of postoperative complications including intraabdominal infection was high in patients with occupational cholangiocarcinoma. Multicentric recurrence occurred not infrequently after surgery because the bile ducts had a high potential for the development of carcinoma. The aggressive treatment including second resection for the multicentric recurrence appeared to be effective.
Introduction
An outbreak of cholangiocarcinoma among workers at a printing company was recently reported 1, 2. Although the mechanism underlying the development of cholangiocarcinoma is still unclear, long-term exposure to high concentrations of dichloromethane (DCM) and/or 1,2-dichloropropane (DCP) is strongly suspected to be a cause 1-3. The Ministry of Health, Labour and Welfare of Japan classified this type of cholangiocarcinoma as “occupational cholangiocarcinoma” on 1 October 2013 3. Thirty-seven patients in all, some of whom have been described in previous reports 1, 2, 4, 5, have been recognized as having occupational cholangiocarcinoma in Japan as of January 2016.
Our previous studies showed that in addition to the main tumor, chronic bile duct injury such as fibrosis of the bile duct wall and periductal tissue, precancerous lesions such as biliary intraepithelial neoplasia (BilIN) and intraductal papillary neoplasm of the bile duct (IPNB) were observed at various sites of the large bile ducts 2, 4, 5. In addition, neoplastic and non-neoplastic biliary lining epithelia at various sites of the bile ducts were found to be immunochemically positive for γ-H2AX, suggesting DNA damages 5, 6. These results indicate (1) the cholangiocarcinoma might have developed from chronic bile duct injuries with DNA injuries into precancerous or early cancerous lesions, and eventually developed into invasive cholangiocarcinoma, and (2) the patients with occupational cholangiocarcinoma are at high risk for development of cholangiocarcinoma at various sites of the bile ducts. However, the outcome of these patients after surgical treatment for occupational cholangiocarcinoma is still unknown. The aim of this study was to investigate the clinicopathological findings and outcomes after surgical intervention for occupational cholangiocarcinoma to establish a treatment strategy for this disease.
Patients and methods
Of the 37 patients with occupational cholangiocarcinoma experienced in Japan, 22 patients underwent surgical treatment. One patient was excluded from this study owing to a lack of information regarding clinicopathological data and another patient was excluded because the carcinoma was suspected to have originated in the pancreas, although the common bile duct was secondarily involved. Thus, the subjects in this study were 20 patients who underwent surgical treatment for occupational cholangiocarcinoma (Table 1). Nineteen (patient no. 1–17, 19, 20) of the 20 patients were former or current workers at eight printing companies in Hokkaido, Miyagi, Saitama, Tokyo, Shizuoka, Osaka, and Fukuoka. These 19 patients were exposed to high concentrations of 1,1,1-trichloroethane (TCE), DCP, and/or DCM over a long period of time 7-9. These chlorinated organic solvents were used to remove ink residues. Another patient (patient no. 18) was exposed to high concentrations of DCP and 1,1-dichloro-1-fluoroethane by removing the dirt from cleaning rolls of coating machines at a company manufacturing IC cards in Kyoto 9. We investigated the clinical findings, laboratory test results, operative methods, pathological findings of the operative specimens, postoperative complications, and the postoperative outcomes.
| Patient no. | Age | Clinical findings | Laboratory tests | Diagnosis of cholangiocarcinoma | Precancerous and early cancerous lesion | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Symptom or health examination | γ-GTP (U/L) | CEA (ng/ml) | CA19-9 (U/ml) | Location | Type | BilIN | IPNB/invasive IPNB | Chronic bile duct injury | ||
| 1 | 34 | DCP, DCM, TCE | Epigastralgia, back pain | 830 | 35.9 | 15200 | Intrahepatic | MF + PI | Yes | Yes | Yes |
| 2 | 34 | DCP, DCM, TCE | Rt. hypochondragia | 785 | 38 | 114 | Intrahepatic | MF + PI | Yes | Yes | Yes |
| 3 | 29 | DCP, DCM, TCE | Jaundice, appetite loss | 264 | 2 | 505 | Distal | Papillary | ND | ND | ND |
| 4 | 35 | DCP, DCM, TCE | Liver dysfunction | 2457 | 1.6 | 119.2 | Perihilar | Papillary | Yes | Yes | Yes |
| 5 | 40 | DCP, DCM | Liver dysfunction | 1049 | 1 | 34 | Intrahepatic+distal | MF + papillary | Yes | Yes | Yes |
| 6 | 38 | DCP, DCM, TCE | Liver tumor | 208 | 2.9 | 2288 | Intrahepatic | MF | Yes | ND | Yes |
| 7 | 40 | DCP, DCM, TCE | Liver dysfunctiona | 1037 | 5.5 | 446 | Intrahepatic | IG | Yes | Yes | Yes |
| 8 | 31 | DCP | Liver dysfunction | 1196 | 5.1 | 1084 | Perihilar | Papillary | Yes | Yes | Yes |
| 9 | 39 | DCP | Liver dysfunction | 486 | 5.4 | 20.6 | Intrahepatic+perihilar | IG + papillary | Yes | Yes | Yes |
| 10 | 39 | DCP | Liver dysfunction | 347 | 1.5 | 105 | Intrahepatic | IG | Yes | Yes | Yes |
| 11 | 31 | DCP | Liver dysfunction | 75 | 2.1 | 501 | Intrahepatic | MF | Yes | Yes | Yes |
| 12 | 34 | DCP | Liver dysfunction | 205 | 5 | 54 | Intrahepatic | IG | Yes | Yes | Yes |
| 13 | 42 | DCP, DCMb | Jaundice | 1404 | 3.1 | 23253 | Perihilar | Scirrhous constricting | Yes | No | Yes |
| 14 | 57 | DCP, DCM | Jaundice | 105 | 1.4 | 1283 | Intrahepatic | MF | Yes | No | Yes |
| 15 | 47 | DCP, DCM | Abdominal pain, back pain | 346 | 11.2 | 3.3 | Intrahepatic | MF | Yes | No | Yes |
| 16 | 46 | DCP, DCM | Epigastralgia, nausea | 1120 | 1.4 | 8.6 | Perihilar | Diffusely infiltrating | Yes | No | Yes |
| 17 | 37 | DCP, DCM | General fatigue | 271 | 2.5 | <2 | Intrahepatic | Papillary | No | Yes | No |
| 18 | 51 | DCP, DCFE | Fever | 1334 | 1.9 | 6 | Distal | Papillary | ND | ND | ND |
| 19 | 54 | DCP, DCM | Jaundice, rt. hypochondralgia | 2122 | 2.4 | 9.1 | Distal | Nodular | ND | ND | ND |
| 20 | 48 | DCP, DCM | Liver dysfunction | 65 | 3.2 | 16 | Distal | Diffusely infiltrating | ND | ND | ND |
- DCFE 1,1-dichloro-1-fluoroethane, DCM dichloromethane, DCP 1,2-Dichloropropane, IG intraductal growth, MF mass-forming, PI periductal infiltration, TCE 1,1,1-trichloroethane
- ND, Pathological examination could not be performed because of the large bile ducts were not available
- a Liver dysfunction was detected during treatment for paranasal sinusitis
- b The amount of DCM exposure was small
Patient data and clinical findings were obtained from the medical records from each hospital and/or interviews with the patients or their family members. The operative specimens of one patient (patient no. 3) were not available in the study because the specimens had been discarded.
The pathological findings were recorded and described according to the World Health Organization Classification of Tumors of the Digestive System 10. Intrahepatic cholangiocarcinoma was grossly classified as a mass-forming, periductal infiltrating, or intraductal growth. Extrahepatic cholangiocarcinoma (perihilar and distal cholangiocarcinoma) was grossly classified as a papillary, nodular, scirrhous constricting, or diffusely infiltrating tumor. Preneoplastic or early preinvasive neoplastic lesions of the biliary tracts were classified as flat dysplastic epithelial tumors (BilIN) or grossly visible papillary tumors (IPNB) 2, 4, 5, 10-14. BilIN lesions were histologically classified according to their cellular and structural features as BilIN-1 (mild atypia), BilIN-2 (moderate atypia), or BilIN-3 (severe atypia corresponding to in situ carcinoma). BilIN-1 lesions presented with mild atypical cellular and nuclear features, such as nuclear membrane irregularities or nuclear enlargements with only minimal disturbances to cellular polarity. BilIN-2 lesions had evident aberrant cellular and nuclear features not sufficient to suggest overt carcinoma; these lesions also had focal disturbances in cellular polarity. BilIN-3 lesions presented with diffuse disturbances in cellular polarity with or without distinct atypical cellular and nuclear features that corresponded to carcinoma in situ. In this study, primary BilIN-2 and BilIN-3 lesions were examined. IPNB was characterized by dilated intrahepatic and extrahepatic bile ducts filled with a papillary or villous biliary neoplasm that covers delicate fibrovascular stalks. The dilated bile ducts were fusiform or cystic (unilobular or multilocular), and the height of such lesions usually exceeds 10 mm, but papillary lesions < 10 mm but > 5 mm showing similar histologies were also occasionally encountered. IPNB was not infrequently associated with focal and minimal invasion (IPNBs with an associated invasive carcinoma). Other pathological terms used in this study were characterized or defined as follows 2, 4, 5. “Chronic bile duct injury” was used as a collective term to describe duct injuries such as epithelial damage, fibrosis of the duct wall and periductal tissue, and chronic inflammatory cell infiltration, in various combinations. Pathological examination for BilIN, IPNB, and chronic bile duct injury were performed mainly at the large bile ducts (the common hepatic duct, the left and right hepatic ducts or to the first to third branches of the intrahepatic bile duct). Pathological examination of the large bile ducts could not be performed in three patients (patient no. 18–20) because these patients underwent pancreaticoduodenectomy.
The cumulative recurrence-free and overall survival curves were calculated using the Kaplan–Meier method.
This study was approved by the ethics committee of Osaka City University, and all of the subjects or their legally authorized representatives (for deceased patients) provided written informed consent. This multicenter occupational cholangiocarcinoma study group consisted of investigators at 19 institutions.
Results
Clinical findings
The ages of the 20 patients at diagnosis were between 29 and 57 years, and all patients were men (Table 1). Five patients (patient no. 8–12) were exposed to high concentrations of DCP; eight patients (patient no. 5, 13–17, 19, 20) were exposed to DCP and DCM (the amount of DCM exposure was small in patient no. 13); six patients (patient no. 1–4, 6, 7) were exposed to DCP, DCM, and TCE; and one patient (patient no. 18) was exposed to DCP and 1,1-dichloro-1-fluoloethane. The period of the exposure to chlorinated organic solvents ranged from 6 years and 1 month to 19 years. One patient (patient no. 13) was a habitual alcohol user (≥80 g of ethanol consumed daily), and 13 patients (patient no. 1–5, 7, 8, 10, 13, 15–17, 20) were smokers. Ten patients (patient no. 1–3, 13–19) visited the hospital because of abdominal pain, jaundice, and/or general fatigue. Ten patients visited the hospital following abnormal results of liver function tests or a liver tumor had been noted during a regular health examinations.
Laboratory test results
At the time of diagnosis of cholangiocarcinoma, the serum concentrations of total bilirubin were elevated in 11 patients. Serum aspartate aminotransferase activity was elevated in 13 patients, and alanine aminotransferase activity was elevated in 15 patients. Serum γ-glutamyl transpeptidase activity was elevated in all 20 patients (Table 1). The serum concentration of carcinoembryonic antigen was elevated in six patients, and the serum concentration of carbohydrate antigen 19-9 (CA 19-9) was elevated in 12 patients. All 20 patients were negative for serum hepatitis B surface antigen and anti-hepatitis C virus antibodies.
Diagnosis of cholangiocarcinoma
Of the 20 patients, 10 were diagnosed with intrahepatic cholangiocarcinoma, four patients were diagnosed with perihilar cholangiocarcinoma, four patients were diagnosed with distal cholangiocarcinoma, one patient was diagnosed with intrahepatic and perihilar cholangiocarcinomas, and one patient was diagnosed with intrahepatic and distal cholangiocarcinomas. The intrahepatic cholangiocarcinomas in seven patients were classified as the mass-forming or mass-forming plus periductal infiltration type, and the intrahepatic cholangiocarcinomas in four patients were classified as the intraductal growth type. Of five patients with perihilar cholangiocarcinoma and five patients with distal cholangiocarcinoma, the carcinoma was classified as the papillary type in six patients, nodular type in one patient, scirrhous constricting in one patient, and diffusely infiltrating type in two patients.
Treatments
Liver resection alone was performed in six patients, liver resection with resection of the extrahepatic bile duct and the reconstruction of biliary tract (hepatico-jejunostomy) in nine patients, liver resection and pancreaticoduodenectomy in one patient, pancreaticoduodenectomy in three patients, and resection of extrahepatic bile duct in one patient (Table 2). Curative resection could not be performed in four patients because of the detection of cancer cells in the resected stumps of the bile ducts. In 18 patients in whom dissection or sampling of the lymph nodes was performed, six patients exhibited metastases to the lymph nodes around the common bile duct, the common hepatic artery and/or peripancreatic lesions.
| Patient no. | Treatments | Recurrence | Prognosis | ||
|---|---|---|---|---|---|
| Operative procedure | Site | Treatment | |||
| 1 | Extended rt. hepatectomy, resection of extrahepatic bile duct | Adjuvant chemotherapy | Chemotherapy | 7 years, 3 months, dead | |
| 2 | Rt. trisegmentectomy | None | Resection margin | Conservative | 1 year, 2 months, dead |
| 3 | Resection of extrahepatic bile duct | None | Intrahepatic (multiple) | Chemotherapy | 1 year, 7 months, dead |
| 4 | Rt. hepatectomy, resection of extrahepatic bile ducta | Adjuvant chemotherapy and radiation for the stump of the bile duct positive for cancer cells | Resection margin (stump of the bile duct positive for cancer cells) | Conservative | 2 years, 3 months, dead |
| 5 | Rt. hepatectomy, pancreaticoduodenectomy | None | None | 8 years, 6 months, alive | |
| 6 | Segmentectomy 8 | None | Intrahepatic (solitary) | RFA, resection | 7 years, 9 months, alive |
| 7 | Extended lt. hepatectomya | Adjuvant chemotherapy and radiation for the stump of the bile ducts positive for cancer cells | None | 3 years, 1 month, dead | |
| 8 | Extended lt. hepatectomy, resection of extrahepatic bile ducta | Adjuvant chemotherapy | None | 5 years, 5 months, alive | |
| 9 | Extended lt. hepatectomy, resection of extrahepatic ducta | Adjuvant chemotherapy and radiation for the stump of the bile ducts positive for cancer cells | Intrahepatic (solitary) | Chemotherapy | 5 years, 3 months, alive |
| 10 | Lt. hepatectomy, segmentectomy 7 | Adjuvant chemotherapy | None | 3 years, 3 months, alive | |
| 11 | Rt. Hepatectomy, resection of extrahepatic bile duct | Adjuvant chemotherapy | None | 3 years, 2 months, alive | |
| 12 | Extended lt. hepatectomy | Adjuvant chemotherapy | Distal common bile duct (solitary) | Resection | 3 years, alive |
| 13 | Extended rt. hepatectomy, resection of extrahepatic bile duct and portal vein | Neoadjuvant chemoradiotherapy + adjuvant chemotherapy | Distal common bile duct (solitary) | Resection | 4 years, alive |
| 14 | Extended lt. hepatectomy, resection of extrahepatic bile duct | None | Resection margin | Radiation | 1 year, dead |
| 15 | Rt. trisegmentectomy | None | Intrahepatic (solitary) | Resection | 1 year, 10 months, dead |
| 16 | Extended rt. hepatectomy, resection of extrahepatic bile duct and portal vein | None | Resection margin | Chemotherapy | 4 years, 5 months, dead |
| 17 | Rt. hepatectomy, resection of extrahepatic bile duct | None | None | 7 years, alive | |
| 18 | Pancreaticoduodenectomyb | Adjuvant chemotherapy | Resection margin (anastomosis of hepatico-jejunostomy) | Chemotherapy | 3 years, 3 months, dead |
| 19 | Pancreaticoduodenectomy | Adjuvant chemotherapy | None | 4 years, 7 months, alive | |
| 20 | Pancreaticoduodenectomy | Adjuvant chemotherapy | None | 9 months, alive | |
- BilIN biliary intraepithelial neoplasia, IPNB intraductal papillary neoplasm of the bile duct
- ND, not determined because of small noncancerous hepatic tissue
- a Non-curative operation because of the detection of cancer cells in the resected stumps of the bile ducts
- b Colectomy for simultaneous colon cancer was performed
Scheduled chemoradiotherapy before surgery was performed in one patient. Three patients underwent radiation therapy at the stump of the bile duct and chemotherapy because the stump of the bile duct was positive for cancer cells. Adjuvant chemotherapy using fluorouracil, gemcitabine, and/or S-1 (tegafur/gimeracil/oteracil potassium) after surgery was administered in 12 patients.
Pathological findings
Mass-forming type of intrahepatic cholangiocarcinoma showed well, moderately, or poorly differentiated adenocarcinoma. Intraductal growth type intrahepatic cholangiocarcinoma and/or papillary-type extrahepatic cholangiocarcinoma exhibited well-differentiated papillary carcinoma (invasive IPNB). BilIN-2/3 lesions were detected in various sites of the large bile ducts and the peribiliary glands in 15 of 16 patients examined. IPNB lesions including invasive IPNB were detected in the various sites of the resected specimens in 11 of 15 patients examined. Chronic bile duct injury was observed at the large bile ducts in 15 of 16 patients examined. BilIN-2/3, IPNB, and chronic bile duct injury were rarely observed in the small bile ducts in the liver.
No cirrhotic changes or other hepatobiliary diseases were detected in the noncancerous hepatic tissues.
Postoperative complications
Postoperatively, intraabdominal infection developed in nine patients (patient no. 1, 2, 4, 5, 9, 12, 14, 19, 20), anastomotic leakage of the hepaticojejunostomy in three patients (patient no. 5, 11, 20), bile leakage developed in one patient (patient no. 9), pancreatic fistula in three patients (patient no. 5, 19, 20), chylous ascites in two patients (patient no. 8, 16), and refractory ascites in one patient (patient no. 13). Cholangitis developed in two patients (patient no. 13, 16) and liver abscess developed in one of these patients. In two patients who underwent pancreaticoduodenectomy, transcatheter arterial embolization was performed for bleeding from the gastroduodenal artery in one patient (patient no. 18) and from the common hepatic artery in one patient (patient no. 19). In one patient, re-operation and stenting was performed for portal vein thrombosis (patient no. 17). Transient hyperbilirubinemia developed in one patient (patient no. 7).
Outcomes
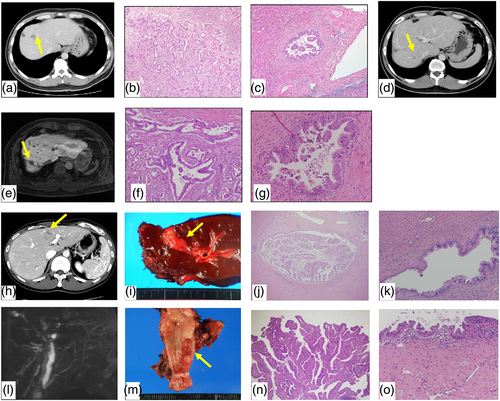
Cholangiocarcinoma recurred in 12 of the 20 patients. The recurrence-free survival rate is shown in Figure 1. In two patients (patient no. 1, 3), multiple intrahepatic metastasis with or without multiple lymph node metastasis occurred after the operation. In five patients (patient no. 2, 4, 14, 16, 18), recurrence occurred at the resection margin including the bile duct stump. In five patients (patient no. 6, 9, 12, 13, 15), solitary recurrent tumors, distant from the primary tumor, were detected after the operation. In one patient (patient no. 6), solitary intrahepatic recurrence (segment 7) developed 10 months after the first operation (segment 8) and radiofrequency ablation therapy (RFA) was performed. The second solitary intrahepatic recurrence (segment 8, the tumor is distant from the first cholangiocarcinoma) occurred 5 years and 10 months after the first operation and the tumor was resected (Fig. 2A–G). The patient is now alive (at 6 years and 10 months after the RFA and 2 years 3 months after the second liver resection) although the patient has tumor recurrence. In one patient (patient no. 9), solitary intrahepatic recurrence distant from the primary tumor occurred 4 years and 4 months after the first operation. The patient was treated with chemotherapy (gemcitabine and S-1) according to the patient's decision. In one patient (patient no. 12), the protruding tumor was detected at the common bile duct 9 months after the first operation (extended left hepatectomy for intrahepatic cholangiocarcinoma) and the tumor gradually enlarged. The extrahepatic bile duct with the tumor was resected at 1 year and 3 months after the first operation, and the pathological examination showed papillary type of the distal cholangiocarcinoma (intraductal papillary neoplasia, high grade), with BilIN lesions around the tumor (Fig. 2H–O). The invasion from the primary cholangiocarcinoma was not detected at the hepatic side stump of the bile duct. The patient is now alive without tumor recurrence (at 1 year and 1 month after the second operation). In one patient (patient no. 13), recurrence occurred at the distal side of the common bile duct 3 years after resection of hilar cholangiocarcinoma (the stump of the bile duct was negative for cancer). The recurrent tumors were distant from the primary cholangiocarcinomas and the pancreaticoduodenectomy was performed. The patient is now alive without tumor recurrence (at 1 year and 3 months after the second operation). In one patient (patient no. 15), a solitary intrahepatic recurrent tumor distant from the original tumors was resected 6 months after the first operation. The patient survived for 1 year and 4 months after the second operation. The recurrent tumors in five patients (patient no. 6, 9, 12, 13, 15) developed at different parts of the bile duct from the primary tumor, and consecutive invasion was not found between the primary lesion and recurrent tumor in the resected specimens obtained from four patients (patient no. 6, 12, 13, 15). Although one (patient no. 15) died 684 days after the first operation, the other four patients survived between 1224 to 2978 days after the first operation.
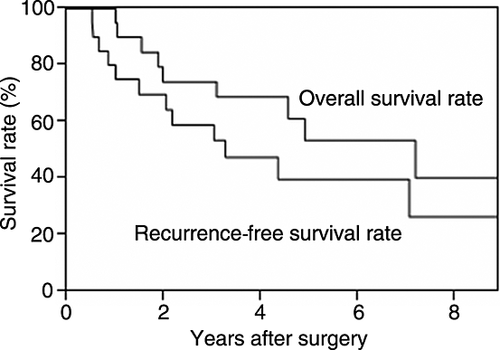
The cumulative recurrence-free and overall survival rates are shown in Figure 1. Eight of the 20 patients died of cholangiocarcinoma recurrence. One patient died of hepatic failure owing to progression of hepatic fibrosis, especially fibrosis of the bile duct wall and periductal tissue, without cancer recurrence 15. The survival time from the first operation to death or the end of this study (April 2016) ranged from 404 to 3241 days (median 1462 days).
Discussion
Our previous studies 2, 4, 16, 17 showed that elevated serum γ-glutamyl transpeptidase activities had increased several years before the diagnosis of cholangiocarcinoma. Regional dilated intrahepatic bile duct without tumor-induced obstruction and primary sclerosing cholangitis-like appearance such as multiple strictures of the bile ducts with or without fusiform dilatation on diagnostic imaging are characteristics of occupational cholangiocarcinoma. On pathological examination, chronic bile duct injuries, such as fibrosis, precancerous or early cancerous lesions, such as BilIN and IPNB, have been observed at the various sites of the large bile ducts 2, 4-6. These characteristics were also observed in most subjects in this study.
In this series, intraabdominal infection developed in nine of the 20 patients. The high incidence of intraabdominal infection might be related to the damage of the bile ducts such as chronic bile duct injuries and precancerous or early cancerous lesions. Innate immunity inherent in the biliary tree might have been disturbed in these patients, and this disturbance may be responsible for frequent intraabdominal infection 18.
Surgical resection is a curative treatment for cholangiocarcinoma 19, 20. However, surgical treatments have been performed in only 22 of the 37 patients with occupational cholangiocarcinoma because the stage of the cholangiocarcinoma was too advanced at the diagnosis in the other 15 patients. These findings indicate that screening and surveillance are important for detecting occupational cholangiocarcinoma at an early stage 16. Of the 20 patients in this study, curative operation could not be performed in four patients because the stump of the bile duct was positive for cancer cells. In this study, BilIN lesions were observed in 15 of 16 patients examined. In patients with the stump of the bile duct positive for cancer cells, invasive carcinoma or BilIN-3 lesion (early cancerous lesion), that involved various sites of the bile ducts, was observed at the stump. Therefore, it is sometimes difficult to perform curative resection for occupational cholangiocarcinoma.
After resection, local recurrence (recurrence at the resection stump including the bile duct stump and adjacent tissue) occurred in five patients and multiple intrahepatic metastasis with or without multiple lymph node metastasis occurred in two patients. In the other five patients, solitary intrahepatic recurrence distant from the primary carcinoma occurred in three patients and solitary recurrence occurred at the distal common bile duct in the other two patients. Consecutive invasion was not observed between the primary tumor and the recurrent tumor. In patients with occupational cholangiocarcinoma, chronic bile duct injuries with DNA injuries and precancerous or early cancerous lesions such as BilIN and IPNB were observed at the various sites of the bile ducts 5, 6, which indicate that the bile ducts have high potential for malignant transformation. Therefore, the recurrent tumors in the five patients might have originated from other sites of the bile ducts; the recurrence occurred in multicentric origin. In the patients with occupational cholangiocarcinoma, it is important to pay attention to not only metastasis from the primary tumor but also multicentric recurrence after the operation.
Recently, the usefulness of aggressive treatments for recurrent cholangiocarcinoma, such as resection or RFA for select patients such as patients with isolated intrahepatic recurrence has been reported 21, 22. In this series, repeated resection or RFA was performed in four patients with solitary recurrent tumors in the intrahepatic or extrahepatic bile duct. It is difficult to evaluate the usefulness of such treatments because the duration after repeated resection or RFA was short. However, if the recurrent tumors are originated from the other site in the bile duct (multicentric origin), as described above, aggressive treatment such as second resection and RFA must be effective because relatively long survival can be expected from the curative treatment for a recurrent tumor of multicentric origin.
In this series, one patient underwent scheduled chemoradiotherapy before surgery, three patients underwent radiation therapy at the stump of the bile duct, and 12 patients underwent adjuvant chemotherapy. However, the clinical significance of such therapies is still unclear because the contents of anticancer agents and radiotherapy were different in each patient.
The extensive fibrotic changes in the bile duct wall and periductal area are also characteristics of patients with occupational cholangiocarcinoma 2, 4, 5, 20. In one patient (patient no. 7), hepatic fibrosis progressed gradually after the operation and eventually hepatic failure developed although the exposure to chlorinated organic solvents had ended 3 years and 2 months before the operation 15. The clinical course of the patient indicated that chlorinated organic solvents caused the progression of fibrosis even after the end of the exposure. The mechanism of such progress of fibrosis should be clarified.
In conclusion, it is sometimes difficult to perform curative resection for occupational cholangiocarcinoma because of extensive tumor invasion and the presence of precancerous or early cancerous lesions such as BilIN and IPNB at the various sites of the large bile ducts. The incidence of postoperative complications such as intraabdominal infection seemed to be high. The recurrence from multicentric origin occurred after surgery in some patients because the bile ducts have a high potential for carcinogenesis due to the presence of precancerous or early cancerous lesions such as BilIN and IPNB at the various sites of the bile ducts. The aggressive treatment including second resection for such multicentric recurrences appeared to be effective, although the clinical significance of adjuvant chemotherapy is still unclear.
Acknowledgments
This study was supported in part by Health and Labor Sciences Research Grants for Research on Occupational Safety and Health (epidemiological and cause-investigated study of cholangiocarcinoma in printing company workers) and by Industrial Disease Clinical Research Grants (establishment of diagnostic methods for occupational cholangiocarcinoma; 14040101-01). This work was also supported in part by the Japan Society for the Promotion of Science KAKENHI Grant Number 26462048 (clinicopathological and molecular biological analysis of carcinogenesis of intrahepatic cholangiocarcinoma by chemicals).
Conflict of interest
None declared.
Author contributions
Study design: Kubo S. Acquisition of data: Kubo S, Takemura S, Tanaka S, Shinkawa H, Kinoshita M, Hamano G, Ito T, Yamamoto T, Terajima H, Tachiyama G, Yamada T, Nakamori S, Arimoto A, Fujikawa M, Tomimaru Y, Sugawara Y, Nakagawa K, Unno M, Mizuguchi T, Takenaka K, Kimura K, Shirabe K, Saiura A, Uesaka K, Taniguchi H, and Fukuda A. Pathological aspects of the study: Yamamoto T, Sato Y, and Nakanuma Y. Data analysis: Kubo S, Kinoshita M, Hamano G, Sato Y, and Nakanuma Y. Manuscript drafted: Kubo S. All authors reviewed the manuscript.