Elderly Onset Primary Intestinal Lymphangiectasia—A Rare Case
Funding: The authors received no specific funding for this work.
ABSTRACT
Primary intestinal lymphangiectasia (PIL) is a rare protein-losing gastroenteropathy characterized by diffuse or localized ectasia of the enteric lymphatics, which can be accompanied by lymphatic abnormalities in other parts of the body. This condition results in hypoalbuminemia, hypogammaglobulinemia, and lymphopenia due to the abnormal leakage of lymphatic fluid into the gastrointestinal tract. As there are no specific serological or radiological tests available, the gold standard for diagnosing intestinal lymphangiectasia is endoscopic examination with histopathological examination of intestinal biopsy specimens. We present a rare case of primary intestinal lymphangiectasia in a 62-year-old Chinese woman who presented with a six-month history of lethargy, persistent diarrhea, and progressive weight loss. Gastroscopy and colonoscopy were performed, and biopsies revealed dilated intestinal lymphatics with broadened villi in the small intestine. Secondary causes of intestinal lymphangiectasia were ruled out, confirming the diagnosis of PIL. The patient was treated with a high-protein, low-fat diet supplemented with medium-chain triglycerides, resulting in significant clinical improvement.
1 Introduction
Primary intestinal Lymphangiectasia (PIL) is a rare protein-losing gastroenteropathy caused by congenital malformations or obstruction of intestinal lymphatic drainage. This leads to hypoproteinemia, lymphocytopenia and other complications that can severely affect a patient's health. While PIL commonly affects children and young adults, we present a unique case of PIL in a 62-year-old Chinese woman diagnosed through endoscopy and histopathological examination. Additionally, this report explores PIL in detail, including its clinical presentation, diagnostic approach and management strategies. The patient showed significant improvement with dietary modifications, underscoring the importance of tailored nutritional support in addressing this rare and challenging condition.
2 Case Report
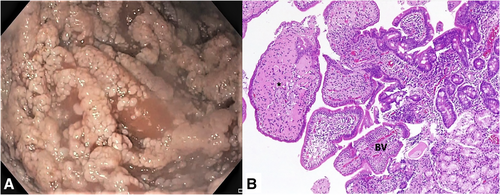
A 62 year old woman presented with a 6 months history of lethargy, persistent diarrhea and progressive weight loss. Apart from bilateral ankle edema, physical examination was unremarkable. Blood tests showed a normal full blood count and normal renal function tests with no albuminuria. Liver function tests were unremarkable except for a low the serum albumin of 28 g/L. We proceeded to perform a gastroscopy and colonoscopy. The gastroscopy showed a normal esophagus and stomach; however examination of the duodenum showed multiple distinctive white mucosal plaques “carpeting” the duodenal bulb and extending to the third part of the duodenum (Figure 1A). Concurrent colonoscopy demonstrated a normal colonic mucosa but similar extensive white plaques were observed in the terminal ileum. Biopsies of the duodenal and ileal mucosa revealed enlarged villi with dilated lymphatic vessels, consistent with intestinal lymphangiectasia (Figure 1B).
The patient had no history of abdominal surgery or radiation therapy and had been in good health prior to the onset of symptoms. Secondary causes of intestinal lymphangiectasia were ruled out, confirming the diagnosis of primary intestinal lymphangiectasia (PIL). Although a computed tomography (CT) scan and enteroscopy were recommended, the patient was reluctant to undergo further testing at that time. She was prescribed a high-protein, low-fat diet supplemented with medium-chain triglycerides. At her six-month follow-up, the patient showed significant improvement, with weight gain, reduced diarrhea, and diminished ankle edema.
3 Discussion
Primary intestinal lymphangiectasia (PIL) is a rare protein-losing gastroenteropathy characterized by diffused or localized ectasia and leakage of enteric lymphatics. These abnormalities are often accompanied by lymphatic abnormalities elsewhere in the body. The ectatic lymphatics may be located in the mucosa, submucosa or subserosa, leading to hypoproteinemia, lymphocytopenia, decreased levels of serum immunoglobulin. PIL arises from congenital malformations or obstructions in the intestinal lymphatic drainage [1, 2]. Symptoms vary depending on the severity of lymphatic loss, ranging from mild lower limb edema to generalized edema, abdominal or pleural effusion, and recurrent diarrhea and abdominal pain [3].
Due to the rarity of PIL, its global prevalence and incidence remain unknown. Since its first description in 1961 by Waldmann et al. [4], only less than 200 cases have been reported in the literature [5]. Although PIL typically develops in childhood, with a mean age of onset of approximately 11 years, milder cases of PIL have been reported adulthood [1, 6]. The exact etiology remains largely unknown; however, a genetic predisposition has been proposed. This hypothesis is supported by the fact that most diagnoses are made in early childhood (< 3 years of age) [3], along with reports of multiple siblings diagnosed with the disorder [7].
The diagnosis of PIL is made through endoscopic examination with biopsy of the duodenum and/or jejunum, revealing characteristic histopathological findings. Endoscopy typically shows scattered lymphangiectasia (white spots) with a characteristic “snowflake” appearance. Histopathological examination of biopsy specimens confirms the diagnosis by identifying dilated lymphatic vessels in the mucosa and submucosa, along with polyclonal plasma cell [8].
The cornerstone of PIL management is dietary modification, which involves a high-protein, low-fat diet supplemented with medium-chain triglycerides (MCT) [9]. This approach helps mitigate protein loss and alleviate symptoms.
In conclusion, PIL is a rare and complex disorder that can significantly impact a patient's health due to its effect on protein and lymphatic loss. While typically diagnosed in childhood, PIL can also present in adulthood with a wide range of symptoms. The exact cause of PIL remains unclear, though a genetic predisposition is suspected. Accurate diagnosis relies on endoscopic evaluation and histopathological examination. Management primarily involves dietary modifications, emphasizing the importance of tailored nutritional support in mitigating the effects of this challenging condition.
Acknowledgments
Li-Han Goh and Khean-Lee Goh wrote the manuscript, and Khean-Lee Goh was primarily responsible for the patient's care. Madhavan Manoharan read the intestinal biopsies and made the histopathological report.
Consent
The patient consent was obtained.
Conflicts of Interest
The authors declare no conflicts of interest.




