Significance of Endoscopic Redness of Duodenum in Health Checkup
Funding: Motohiko Kato received “Research grant for prevention of lifestyle-related diseases in 2018” from the Japan Health Promotion Foundation.
ABSTRACT
Background and Aim
It is important for endoscopist to diagnose the lesion redness. In this study, we focused on the redness of duodenal bulb. We objectively analyzed the changes in redness of the duodenal bulb using linked color imaging (LCI) with chromatic indicators.
Methods
Seven endoscopists observed the duodenal bulb with white light imaging (WLI) and LCI, and evaluated them by visual analogue scale (VAS) for the degree of redness. The difference in VAS between WLI and LCI was defined as ΔVAS. All images were quantified by the Comission Internationale de l'Eclariage-L*a*b* color space. Values related to color differences (ΔE*, ΔL*, Δa*, and Δb*) were calculated from the two images of WLI and LCI. Multiple regression analysis was performed for the factors with the health checkup correlated with ΔVAS and the correlation between ΔVAS and ΔE*, ΔL*, Δa*, and Δb* was also examined.
Results
The analysis prospectively included 1144 examinees. In multiple regression analysis, it revealed that sex (β = 0.5847, p < 0.0001) and metabolic syndrome (β = 0.4138, p = 0.0012) were the factors independently influenced ΔVAS. And only Δa*, a chromatic index for changes in the degree of redness, showed a statistically and considerably positive correlation with ΔVAS (r = 0.4529, p < 0.0001).
Conclusion
To evaluate the difference in the degree of redness between WLI and LCI of duodenal bulb in esophagogastroduodenoscopy may help in early detection of metabolic syndrome, which rarely has symptoms.
1 Introduction
With the development of endoscopic technology including image-enhanced endoscopy [1-3] and widespread use of endoscopic instruments, the opportunities to undergo esophagogastroduodenoscopy (EGD) are increasing. Recently, we focused on cases in which the duodenal bulb appeared red in combination with linked color imaging (LCI) in screening EGDs.
LCI is an image-enhanced endoscopy that can enhance slight differences in color by extending color saturation and color phase differences in the red legion [3]. By this technology, the usefulness for the diagnosis of Helicobacter pylori (Hp) infection related-gastritis [4] and identification of Barrett's esophagus [5], gastric cancer [6, 7], duodenal tumor [8], and colorectal polyp [9, 10] was reported. However, there are no previous reports on the degree of redness of the duodenal bulb in itself including LCI, and its clinical significance is unknown. We hypothesized that it might be a sign of some disease of which the patient is unaware. Our institution is a private and corporate health checkups facility that includes EGD. The health checkups include a detailed interview including oral medication, and blood tests related to Hp infection and lifestyle-related diseases are actively conducted. Taking advantage of this situation, we decided to examine factors associated with redness of duodenal bulb in a large number of healthy subjects.
Therefore, the aim of this study was to explore the health checkup findings associated with the amount of change in the degree of reddish perception of the duodenal bulb by endoscopists with LCI compared to white light imaging (WLI). Furthermore, we evaluated objectively how the perception of redness in the duodenal bulb by endoscopists changes with LCI compared to WLI, using chromatic indicators.
2 Methods
2.1 Study Design
This was an exploratory prospective observational study with a single-center. The entry period was set to be within approximately 3 years, and the target number of examinees was set at 1200, based on the calculation of the number of examinees who could be entered into the study based on the number of annual examinees at the Japan Health Promotion Foundation. As a result, consecutive 1200 examinees who were performed the health checkup including EGD in Japan Health Promotion Foundation from June 2019 to December 2022 were included in this study. The exclusion criteria were as follows: cases with a history of surgery for the upper gastrointestinal tract, cases with a history of hereditary diseases with gastrointestinal polyposis, and cases with inflammatory diseases including duodenal ulcer and inflammatory bowel disease. The institutional review board of the hospital with the health checkup institution approved this study, and the Ethics Committee within the Japan Gastroenterological Endoscopy Society formally reviewed and approved this study (E19-002). In addition, this study was performed in compliance with the 2013 revision of the Helsinki Declaration.
2.2 Endoscopic Procedure
EGD as the health checkup was performed by seven specialized endoscopists consisted of four institutions; Tokyo University, Keio University, Teikyo University and Toho University. All endoscopists have been certified Japan Gastroenterological Endoscopy Society without visible color blindness. We routinely used transnasal endoscope (EG-L580NW, Fujifilm Corporation, Tokyo, Japan) with the LASERIO endoscopic system (Fujifilm Corporation, Tokyo, Japan). When performing EGD, pictures of duodenal bulb were taken by WLI and LCI, respectively, on condition that were filled direct view angle and on equal terms whenever possible.
2.3 Evaluation of Redness Every Endoscopic Image With Endoscopists' Color Perception
Degree of redness have been prospectively evaluated at once, performing EGD, according to 0–100 as visual analogue scale (VAS) [11] for every image by the same endoscopists taken the pictures. ΔVAS was determined as difference in VAS between WLI and LCI, and it was reflected the difference in perception of redness between two images by the endoscopists.
2.4 Information of Health Checkup Examinees
All examinees were performed health checkup items by Japan Health Promotion Foundation consisted of physical examination, blood test, urinalysis, chest X-ray, electrocardiogram, and EGD. Especially, since the Japanese have a relatively high rate of Hp infection, anti-serum IgG antibody titer for Hp and pepsinogen I and II were measured at the examination to assess their Hp infection status [12]. Hp infection status was classified into (1) present infection state, (2) post eradication state, and (3) uninfected state by these results and eradication history interview; diagnosed as (1) when satisfied anti-serum Hp IgG antibody titer positive without history of eradication therapy, (2) when satisfied anti-serum Hp antibody titer negative and presence of eradication therapy, and (3) when satisfied anti-serum Hp antibody titer negative without history of eradication therapy. Pepsinogen I/II ratio was determined due to analogize the decreased gastric acid secretion capacity due to Hp continuous infection state. Pepsinogen I/II ratio of 3.1 or higher is considered normal, while 3.0 or lower suggests decreased gastric acid secretory capacity associated with persistent Hp infection [12]. Medical interview about history of taking non-steroidal anti-inflammatory drugs (NSAIDs), antithrombotic drugs (antiplatelet drugs and anticoagulant drugs), and proton pump inhibitors (PPIs) was performed. Moreover, the results of these examinations were also used to determine metabolic syndrome (MetS) [13] to assess the risk of life-style related diseases and cardiovascular events for the examinees. Diagnostic criteria for MetS are as follows: waist diameter of at least 85 cm for men and 90 cm for women, and at least two of the following: (1) lipid abnormalities (triglyceride ≥ 150 mg/dL and/or high-density-lipoprotein cholesterol < 40 mg/dL), (2) hypertension (systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure≥ 85 mmHg), or (3) hyperglycemia (fasting blood sugar ≥ 110 mg/dL).
2.5 Objective Evaluation of Endoscopic Images Based on the Chromatic
Evaluating color objectively, we employed Comission Internationale de l'Eclariage (CIE)-L*a*b* color space [14] to digitize color of the pictures. All colors can be quantified by CIE-L*a*b* color space, plotting the color on the coordinates of a cubic function. Of the three axes, L* axis is defined as degree of brightness, a* axis as degree of redness, and b* axis as degree of yellowness. L*, a*, and b* values of each image paired with WLI and LCI were calculated, excised the images as square shaped at the maximum as possible and processing the color of whole image averagely and uniformly by Photoshop 2023 (Adobe System Inc., San Jose, California, United States). The definitions for the difference between two colors using the CIE-L*a*b* color space are as follows; ΔE* is the color difference quantified the degree of difference between two colors and is calculated as the distance between two colors on the graph, ΔL* is the difference of degree of brightness between two colors, Δa* is the difference of degree of redness between two colors and Δb* is the difference of degree of yellowness between two colors, respectively (Figure S1).
In this study, we obtained ΔE*, ΔL*, Δa*, and Δb* to digitize the difference of degree of color between WLI and LCI, to calculate using L*, a*, and b* values of each pair of WLI and LCI pictures.
2.6 Outcomes
The primary outcome of this study was set as correlation between ΔVAS and each health checkup data (age, sex, height, weight, presence of NSAID, antithrombotic drug and/or PPI medication, Hp infection status, pepsinogen I/II ratio, and MetS).
The secondary outcomes of this study were set as correlation between the factors affected ΔVAS and ΔVAS values and correlation between ΔVAS and difference in each factor of CIE-L*a*b* color space (ΔE*, ΔL*, Δa*, and Δb*).
2.7 Statistical Analysis
Statistical analysis was carried out using JMP software (version 15.1.0, SAS Institute Inc., Cary, NC, United States). Multiple regression analysis was performed on factors affecting ΔVAS. In multiple regression analysis, t-value represents the magnitude of the effect of each explanatory variable on the objective variable; the larger the value, the stronger the effect. β-value is the standardized partial regression coefficient, which is the degree of influence on the regression equation; the larger its absolute value, the stronger the influence of the explanatory variable. R2-value is the coefficient of determination, which is a measure of the accuracy of the multiple regression equation. The closer the adjusted R2-value is to 1, the higher the accuracy of the multiple regression equation. Furthermore, we performed t test for the factors that affected ΔVAS in the results of multiple regression analysis and ΔVAS (> 0 or < 0). Next, correlation coefficients between the color difference of WLI and LCI perceived by endoscopists (ΔVAS) and ΔE*, ΔL*, Δa*, and Δb*, which are barometers of chromatic difference were analyzed to determine the presence of correlation each other. When it was statistically significant, the correlation coefficient, r value, was evaluated as follows: 0 < r < |0.2|, almost no correlation; |0.2| < r < |0.4|, slightly correlation; |0.4| < r < |0.7|, considerable correlation; |0.7| < r < |1|, considerably strong correlation, respectively. All p values were two-tailed, and p < 0.05 was considered to be statistically significant.
3 Results
3.1 Participants Flow
From June 2019 to December 2022, 1200 examinees underwent medical checkups in the facility. After excluding examinees with absence of LCI images (N = 34), poor images for the chromatic evaluation (N = 19), Von Hippel–Lindau disease (N = 1), duodenal ulcer (N = 1), and ulcerative colitis (N = 1), 1144 examinees were enrolled and analyzed (Figure S2).
3.2 Characteristics
The characteristics of the examinees in this study are shown in Table 1. The median age was 47 years, and approximately 70% of the examinees were male. Medications including NSAID, antithrombotic and PPI were a few percent, respectively. About Hp infection status, 8.9% and 17.6% of the examinees were current status and after eradication status, respectively. Pepsinogen I/II ratio was 5.2, within normal range. Details of another blood test items (Triglyceride, high-density lipoprotein cholesterol, and fasting blood sugar) and blood pressures related to MetS are shown in Table 1.
| Factors | N = 1144 | |
|---|---|---|
| Age | Median (range) | 47 (23–89) |
| Sex, n (%) | Male | 798 (69.8) |
| Height, n (m) | Median (range) | 1.69 (1.43–1.92) |
| Weight, n (kg) | Median (range) | 65.2 (37.5–128.0) |
| Waist circumference, n (cm) | Median (range) | 83.0 (55.4–124.7) |
| NSAID medication, n (%) | Present | 12 (1.0) |
| Antithrombotic medication, n (%) | Present | 22 (1.9) |
| PPI medication, n (%) | Present | 31 (2.7) |
| Current Hp infection, n (%) | Present | 102 (8.9) |
| Past history of Hp eradication, n (%) | Present | 201 (17.6) |
| Pepsinogen I/II ratio, n | Median (range) | 5.2 (0.3–11.8) |
| Triglyceride, n (mg/dL) | Median (range) | 92 (24–976) |
| HDL-C, n (mg/dL) | Median (range) | 63 (29–149) |
| Fasting blood sugar, n (mg/dL) | Median (range) | 92 (57–325) |
| Systolic blood pressure, n (mmHg) | Median (range) | 120 (81–200) |
| Diastolic blood pressure, n (mmHg) | Median (range) | 76 (48–121) |
- Abbreviations: HDL-C, high-density lipoprotein cholesterol; Hp, Helicobacter pylori; NSAID, non-steroidal anti-inflammatory drug; PPI, proton pump inhibitor.
3.3 Difference in the Perception of Redness According to the Endoscopists' Feeling
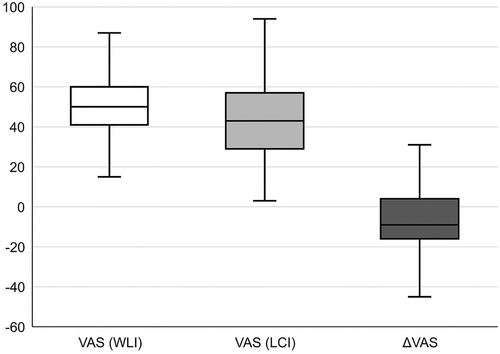
The endoscopists evaluated the VAS for every WLI and LCI images by their own perception of redness, and ΔVAS was calculated by subtracting the VAS for WLI from the VAS for LCI (Figure 1). As a result, median VAS (WLI) was 54, median VAS (LCI) was 43, and median ΔVAS was −9, respectively.
3.4 Multiple Regression Analysis for ΔVAS
Next, we performed a multiple regression analysis for ΔVAS to evaluate the impact of each background factor on the ΔVAS (Table 2). It was determined that the model was significant (p < 0.0001), however, showed only 3.5% of variance. As a result, only sex (β = 0.5847, p < 0.0001) and meeting the diagnostic criteria for MetS (β = 0.4138, p = 0.0012) were found to be the factors independently influenced ΔVAS.
| (Factors) | β | t | p |
|---|---|---|---|
| Age | −0.0001 | −0.6556 | 0.5136 |
| Sex | 0.5847 | 4.3746 | < 0.0001 |
| Height | −0.0007 | −1.5629 | 0.2640 |
| Weight | 0.0001 | 1.0042 | 0.3264 |
| NSAID medication | −1.3691 | −1.0729 | 0.2436 |
| Antithrombotic medication | 0.1422 | 0.2003 | 0.8413 |
| PPI medication | −0.4891 | −0.9325 | 0.2835 |
| Hp infection | −0.0695 | −0.4180 | 0.6718 |
| Pepsinogen I/II ratio | −0.0052 | −0.6171 | 0.5945 |
| Diagnosed as MetS | 0.4138 | 2.8898 | 0.0012 |
| R2 = 0.0432, Adj. R2 = 0.0347, p < 0.0001 | |||
- Abbreviations: Adj. R2, adjusted R2; Hp, Helicobacter pylori; MetS, metabolic syndrome; NSAID, non-steroidal anti-inflammatory drug; PPI, proton pump inhibitor; VAS, visual analogue scale.
3.5 Relationship Between ΔVAS and MetS
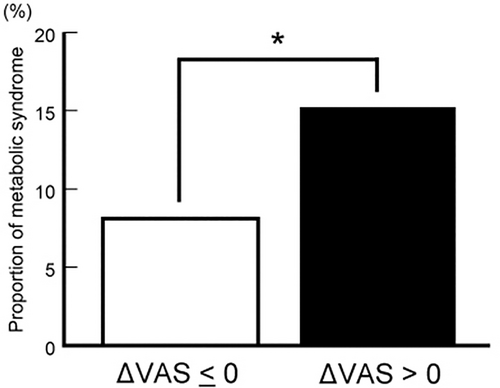
We focused on MetS from the results of a multiple regression analysis. When the ΔVAS was divided into groups with ΔVAS greater than 0 and less than 0, the former had a significantly higher frequency of MetS (15.2% v.s. 8.2%, p = 0.0005) (Figure 2). By the way, five examinees which consisted of one examinee with Δa* > 0 and four examinees with Δa* ≤ 0 were performed biopsy from the duodenal bulb by chance. In both groups, just only mild chronic duodenitis was noted, and there were no specific differences on the hematoxylin–eosin stain specimens, including the degree of inflammatory cell infiltration, congestion, or angiogenesis.
3.6 Image Analysis by CIE-L*a*b* Color Space Between WLI and LCI
Table 3 shows the L*, a*, and b* values of WLI and LCI calculated by image analyses and values for the difference in color between the two images calculated from each L*, a*, and b* values. ΔE* indicated as the color difference between WLI and LCI showed 15.8, ΔL* indicated as the brightness difference showed 8, Δa* indicated as the redness difference showed −7, and Δb* indicated as the yellowness difference showed −9, respectively, as the median.
| Factors | Data | ||
|---|---|---|---|
| WLI | L* | Median (range) | 52 (26–65) |
| a* | Median (range) | 28 (9–45) | |
| b* | Median (range) | 33 (17–53) | |
| LCI | L* | Median (range) | 60 (5–72) |
| a* | Median (range) | 20 (2–43) | |
| b* | Median (range) | 24 (4–49) | |
| ΔE* | Median (range) | 15.8 (6.6–45.7) | |
| ΔL* | Median (range) | 8 (−44–30) | |
| Δa* | Median (range) | −7 (−21–9) | |
| Δb* | Median (range) | −9 (−30–9) | |
- Abbreviations: LCI, linked color imaging; WLI, white light imaging.
3.7 Correlation of Endoscopists' Color Perception and Color Analysis
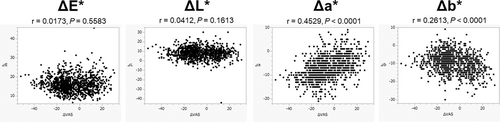
We assessed the correlation between ΔVAS and ΔE*, ΔL*, Δa*, and Δb* (Figure 3). Among them, only Δa* showed a statistically and considerably positive correlation with ΔVAS (r = 0.4529, p < 0.0001), although there were no statistically correlations between ΔVAS and ΔE* (r = 0.0173, p = 0.5583), ΔL* (r = 0.0412, p = 0.1613) and Δb* (r = 0.2613, p < 0.0001).
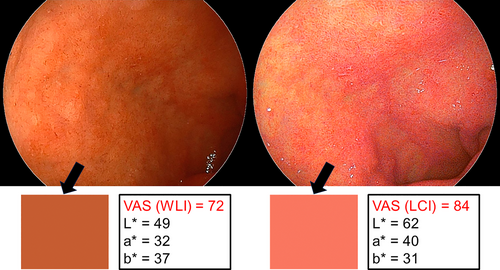
3.8 Case Presentation of MetS With Increased Redness at LCI
We presented representative case with MetS and increased levels of redness at LCI compared with WLI, both endoscopist's sense and chromatic evaluation in this study. The case was a male in his 60's. Upon observation of the duodenal bulb by EGD, the endoscopist rated the VAS (WLI) at 72 and the VAS (LCI) at 84 (Figure 4). ΔVAS was 12, indicating more reddish in the LCI compared to the WLI by the endoscopist. Image analysis revealed that the WLI had L*, a*, and b* of 49, 32, and 37, respectively, while the LCI had L*, a*, and b* of 62, 40, and 31, respectively (Figure 4). From the above values, values related to color difference were obtained; ΔE* was 16.4, ΔL* was 13, Δa* was 8, and Δb* was −6. Chromatically, the color changed from WLI to LCI to a reddish-purple appearance. The case's results of health checkup revealed an abdominal circumference of 112.1 cm, hypertriglyceridemia (283 mg/dL) and systolic hypertension (146 mmHg), which met the diagnostic criteria for MetS.
4 Discussion
In this study, ΔVAS as the endoscopists' perception of the difference in redness was statistically influenced by sex and MetS. Especially, the frequency of MetS was significantly higher in cases in which ΔVAS showed greater than 0 compared with less than 0. And ΔVAS was statistically positively correlated with Δa*, which is considered a chromatic measure of redness difference.
Because the population consisted of cases who had undergone health checkup in this institution, we could examine a variety of factors associated with ΔVAS in this study using multiple regression analysis. As a result, ΔVAS was independently correlated with sex and MetS. Because men and women have each different bodies, there may be differences in the penetration of light emitted from the scope into the duodenum, which may result in different visibility for endoscopists. There may be some lifestyle or other sex-related differences between men and women that we have not been able to examine in this study. We are not able to interpret the accurate reason for the association between endoscopic redness in duodenum and sex in detail, however, the large number of examinees designated by workplaces resulted in a very large proportion of males, which may have affected the results. It is reported that MetS is more frequent in men than in women in Japanese [15], which may have confounded the present results. The reason to support the association between reddish emphasis of duodenum in LCI and MetS is not clear from the results of this study alone since the duodenal biopsy for all examinees was not included in the study plan. Therefore, we speculate that the visceral fat accumulated by MetS may have coated the duodenum and altered the light transmission through the endoscope. Moreover, MetS is said to induce various types of inflammation mediated by adipokines [16] to many organs including the upper gastrointestinal tract [17, 18], and adipokines in the body elevated by MetS may induce some inflammation in the duodenum. To prove these hypotheses, we assume that it would be necessary to perform duodenal biopsy for some examinees and animal experiments using obese model with endoscopic examination, histological evaluation, and adipokine analysis.
In the present study, the frequency of MetS was higher in the group with a ΔVAS greater than 0 (15.2%) compared to the previously reported 7.1% frequency in Japanese in their 40s [19]. MetS is a condition in which visceral fatty obesity is accompanied by lipid abnormalities, hypertension, and hyperglycemia [13]. Early detection of MetS is important because it increases the risk of myocardial infarction and cerebral infarction in the future due to arteriosclerosis [15, 20]. However, MetS has few symptoms, and there are not many opportunities for diagnosis. LCI is an image-enhanced endoscopy increasing brightness and redness that has recently been introduced [21]. Endoscopists can easily use LCI by simply pressing a button on the scope, and LCI can be used immediately at any time without any invasiveness to the patient. Therefore, evaluation of duodenal bulb for redness in combination with LCI during a health checkup may be one of a valuable trigger for diagnosing MetS.
Analysis of chromatic differences between WLI and LCI revealed L* values increased in LCI compared to WLI, while a* and b* values decreased. Instead, those results seemed reasonable, because LCI is an image-enhanced endoscopy with increasing brightness [21], so the L* value would increase and the overall color component would accordingly decrease due to brightness. The median ΔVAS defined as a difference in redness perception when comparing LCI and WLI was a negative number, which means they felt that the redness decreased with LCI in many cases. Therefore, the change in color tone between WLI and LCI was generally linked to the change in chromatic index and the endoscopists' perception of redness. It showed that the sensory evaluation was objectively supported. In addition, analysis of the relationship between ΔVAS defined as the endoscopists' perception of redness and ΔE*, ΔL*, Δa*, and Δb* defined as the chromatic difference indicators showed that only Δa* had a statistically positive correlation with ΔVAS. This result was simple and very easy to understand since Δa* is exactly the value that indicates the difference in the degree of redness. Interestingly, it also suggests that at least the expert endoscopists would be able to properly assess changes in the degree of redness.
This is the first time that we have examined the reddish emphasis in duodenum of LCI compared to WLI, as there have been no previous reports of such a disease. But in general, duodenitis and ulcer associated with Hp infection and duodenitis associated with hypersecretion of gastric acid are necessary to distinguish diseases in which the entire duodenal bulb turns distinctly reddish only with WLI. In the former case, the redness should be shown slight shading of redness with erosions or ulcers, and in the latter case, the redness should be also shown slight shading of redness and no uniformity of redness, which is an important point of differential diagnosis based on endoscopic findings. Furthermore, the present study revealed that the degree of redness was not emphasized by LCI in these diseases.
This study has several limitations. First, this has been evaluated only by well-experienced and specialized endoscopists. Second, color analyses were performed by not moving image but still images. Third, color analyses were evaluated by averaging the colors of the still images, which failed to take into account the maximum and minimum reddish tones. Moreover, the reasons for the increased redness of the duodenal bulb when observed with LCI in MetS cases has not been proven. Then we would like to perform a biopsy of the duodenum from some cases and plan experiments in animals with obese model, to perform histological evaluations and find causes of red appearance of the duodenal bulb endoscopically.
In conclusion, cases in which endoscopists perceived redder observing LCI than WLI were associated with MetS, and the degree of endoscopists' perception of redness was chromatically correlated with Δa*. We hope that this will lead to improve the quality of health checkups and provide the opportunity to the early detection of lifestyle-related diseases.
Acknowledgments
Authors would like to acknowledge all the nurses and office staff at the Ebisu Heart Building Clinic to be supported in this study.
Ethics Statement
This study protocol was reviewed and approved by the Ethics Committee within the Japan Gastroenterological Endoscopy Society, approval number E19-002. The written informed consent was obtained from all the participants.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.




