Relationship Between Adenoma Detection Rate and Respective Withdrawal Time in Different Colon Segments: A Retrospective, Single-Center Study
Funding: This work was supported by Natural Science Foundation of Jiangsu Province (BK20231146), Key Program of Wuxi Medical Center, Nanjing Medical University (WMCM202305) and Cohort Research Program of Wuxi Medical Center, Nanjing Medical University (WMCC202314).
Xujin Chen and Bingxin Xu contributed equally to this work.
ABSTRACT
Background and Aims
The 6-min withdrawal time for colonoscopy is widely considered the standard of care. However, there may not be appropriate if the 6-min is equally divided into various colon segments. Since the adenoma detection in each colon segment is not the same, there may be differences with the withdrawal time in different colon segments. Our objective was to evaluate the relationships between adenoma detection rate (ADR) and respective withdrawal time in different colon segments.
Methods
Outpatients, age range 18–75 years, undertaking complete colonoscopy were enrolled in this study from November 2019 to November 2020 in the digestive endoscopy center. The entire colon was divided into four different segments: ascending colon, transverse colon, descending colon and rectosigmoid colon. The respective withdrawal time and ADR in each colon segment were recorded respectively.
Results
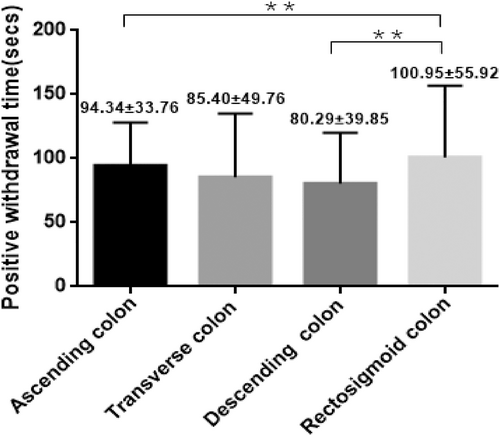
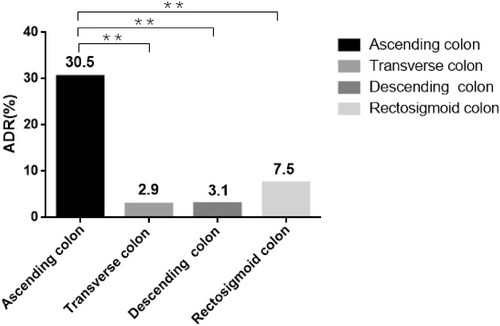
A total of 586 outpatients (279 males, 307 females) enrolled in this study and the general ADR was 38.2%. The positive withdrawal time (adenomas detected) was longer than negative withdrawal time (non-adenomas detected) (334.04 ± 24.21 s vs. 303.65 ± 5.20 s, t = 1.26, p < 0.001). ADR in ascending colon, transverse colon, descending colon and rectosigmoid colon were respectively 30.5%, 2.9%, 3.1% and 7.5%. While all of their positive withdrawal time were longer than negative withdrawal time (94.34 ± 33.76 s vs. 70.40 ± 41.84 s, t = 3.31, p = 0.001; 85.40 ± 49.76 s vs. 71.66 ± 36.87 s, t = 1.95, p = 0.025; 80.29 ± 39.85 s vs. 69.73 ± 35.96 s, t = 1.40, p = 0.016;100.95 ± 55.92 s vs. 80.96 ± 42.87 s, t = 3.61; p < 0.001, respectively). The withdrawal time threshold in the ascending colon, transverse colon, descending colon, rectosigmoid colon determined by receiver operating characteristic (ROC) curve were 77, 61, 56 and 109 s, respectively. In the ascending colon, ADR was significantly higher (47.0% vs. 33.1%, p < 0.001) when the colonoscopy withdrawal time was ≥ 77 s. When the withdrawal time was ≥ 61 s in the transverse colon (42.7% vs. 32.7%, p = 0.013), ≥ 59 s in the descending colon (42.3% vs. 29.9%, p = 0.004) and ≥ 109 s in rectosigmoid colon (52.2% vs. 33.9%, p < 0.001), ADR was also significantly higher. After adjusting for age, sex and BMI, Logistic regression analysis showed that withdrawal time ≥ 77 s in the ascending colon (OR, 1.796; 95% CI, 1.273–2.532; p < 0.001), ≥ 61 s in the transverse colon (OR, 1.535; 95% CI, 1.094–2.155; p = 0.013), ≥ 56 s in the descending colon (OR, 1.722; 95% CI, 1.193–2.486; p = 0.004) and ≥ 109 s in the rectosigmoid colon (OR, 2.134; 95% CI, 1.446–2.350; p < 0.001) were independent risk factors for the increase of ADR.
Conclusions
ADR and withdrawal time are all various in individual colon segments. During the operation of colonoscopy, withdrawal time in the ascending colon may be shortened appropriately. The adenomas in the rectosigmoid colon are more likely to be detected and do not take longer withdrawal times. We need to choose the appropriate time according to different colon segments.
Abbreviations
-
- 95% CI
-
- 95% confidence interval
-
- ADR
-
- Adenoma detection rate
-
- OR
-
- Odds ratio
-
- PDR
-
- Polyp detection rate
-
- SDR
-
- Serrated polyp detection rate.
-
- SSL
-
- Sessile serrated polyps
1 Introduction
Colorectal cancer (CRC) is the third most common malignant tumor in the world and its mortality rate ranks the second [1, 2], its incidence is still rising. It is predicted that the number of new CRC cases will reach 3.2 million globally in 2040 [3]. The trend of CRC in younger adults has been confirmed. Recent data shows that the incidence and mortality of early-onset colorectal cancer (age at diagnosis < 50 years) are increasing rapidly worldwide [4, 5], which represents a huge public health challenge.
Regular colonoscopy and timely intervention of polyps can effectively prevent colorectal cancer [6]. After colonoscopy screening and polypectomy, the incidence of colorectal cancer can be reduced by 46% and the mortality rate can be reduced by 88% [7, 8]. However, at present, the rate of missed adenoma diagnosis in colonoscopy is as high as 26% (95% CI: 23%–30%) and the rate of missed advanced adenoma diagnosis is as high as 9% (95% CI: 4%–16%) [9]. However, every 1% decrease in the adenoma detection rate (ADR) will increase the risk of colorectal cancer by 3% [10]. Therefore, improving ADR has become one of the important measures to prevent colorectal cancer. Extending the withdrawal time can improve the ADR of the proximal and distal colon and reduce the rate of missed diagnosis [11]. At the same time, for patients who undergo a complete colonoscopy, the influencing factors related to ADR, such as bowel preparation, endoscopists' experience and endoscopic equipment, have become established facts, while the withdrawal time has become the most important intervention factor [12, 13]. In 2019, the National Clinical Research Center for Digestive Diseases (Shanghai) recommended [14] that the withdrawal time should not be less than 6 min, which is consistent with American and European guidelines [15, 16]. However, most of the cohort studies that report the withdrawal time and ADR are retrospective studies, there are no studies that report the withdrawal time and ADR of individual colonic segments in China. At the same time, the higher rate of missed diagnosis of adenomas in the proximal colon leads to no significant decrease in the mortality rate [17]. Therefore, we carried out this study in order to explore the reasonable withdrawal time and improve the ADR of individual colonic segments which finally improve the quality of colonoscopy.
2 Methods
2.1 Study Design and Participants
This was a retrospective observational study involving 586 consecutive patients who underwent screening, surveillance or diagnosis sedated colonoscopy from November 2019 to November 2020 by 29 endoscopists at the Affiliated Wuxi People's Hospital of Nanjing Medical University, Department of Digestive Endoscopy Center. Endoscopists were divided into four grades according to their working years and the total number of colonoscopies [18, 19], thus, minimize the influence of the endoscopist on colonoscopy results. Grade A endoscopists had 5 < X ≤ 10 years of endoscopic experience and the annual number of colonoscopy operations reached 800; Grade B endoscopists had 10 < X ≤ 15 years of endoscopic experience and the annual number of colonoscopy operations reaches 1000; Grade C1 and Grade C2 endoscopists had similar work experience, which above 15 years and the annual number of colonoscopy operations reached 1500. Seven to eight endoscopists were assigned to each level. Each endoscopist enrolled consecutive patients for a period of time during the study.
The inclusion criteria for patients was as follows: (1) age ≥ 18 year, age ≤ 75 year; (2) patients who underwent colonoscopy for the first time, or at least not within the last 5 years. The exclusion criteria included: (1) patients with a history of colorectal surgery; (2) patients with familial adenomatous polyposis; (3) patients with inflammatory bowel disease; (4) patients with inadequate bowel preparation (Boston bowel score < 2 for any segment or < 6 for all segments); (5) patients who were difficult to identify hepatic flexure and splenic flexure; (6) patients who could not tolerate colonoscopy or reach the ileocecal area during the colonoscopy; (7) additional retroflexion observations in any colon segment; (8) patients with incomplete data, which would affect data analysis.
2.2 Bowel Preparation and Colonoscopy Procedure
Preparation before colonoscopy: patients should complete blood coagulation function, infectious diseases and electrocardiogram examination before the colonoscopy. Irritating food or medicine that affected gastrointestinal motility should be forbidden for patients 3 days before colonoscopy. Low-fiber diet was recommended before colonoscopy. Food and water were forbidden for patients at least 4 h before colonoscopy. At 7:00 a.m. on the day of examination, 4 L of polyethylene glycol solution was dissolved in 3000 mL warm water, patients should take it evenly in 3 h. At 10:00 a.m., 5 g dimethicone oil was mixed with 100 mL water for a single dose. Colonoscopy would be performed after suction of the fluid residue. Endoscopists estimated the quality of bowel preparation on the basis of the extent of mucosal visualization. The quality of the bowel preparation was graded by Boston bowel preparation scale.
Colonoscopy procedure: All the endoscopists who performed colonoscopy had worked for more than 5 years. Patients were in the left lateral position [20, 21] and none of the patients changed positions during colonoscopy. All colonoscopes were advanced to the ileocecal region. High-definition colonoscopes (Olympus CV-290 host and CF-HQ290I colonoscopy) were used for all colonoscopy without a distal attachment cap. We retrospectively measured the colonoscopy withdrawal times in the ascending colon segment (including cecum and hepatic flexure), transverse colon segment, descending colon segment (including splenic flexure) and rectosigmoid colon segment. Endoscopists were required to take pictures with computer system when taking into the anus; reaching the cecum, hepatic flexure, splenic flexure, sigmoid colon and other symbolic parts. The time was recorded by the computer system at the instant of the polyps were found and after the polyps were biopsied. Per institutional protocol all colonoscopies were videotaped. The data of all patients included in the study were obtained from the database of the digestive endoscopy center. The time of each colonic segment was calculated by two senior Grade C endoscopists according to the time in the photographs, and was verified by a third Grade C endoscopist.
The amount of time taken for biopsy specimen or polyp removal was measured and subtracted from the withdrawal times. Also, the amount of time taken to clean the mucosa and for the suctioning of excessive retained fluid was excluded from the determination of the withdrawal time.
2.3 Histopathologic Evaluation
Pathological specimens were placed in 10% formalin (40% formaldehyde) solution and sent for histopathological examination. All pathology specimens were reviewed by two GI pathologists at the Affiliated Wuxi People's Hospital of Nanjing Medical University. The histology of individual polyps was recorded by location.
2.4 Data Collection
We included data on patient demographics, colonoscopy withdrawal times, endoscopist experience levels, Boston bowel preparation scores and adenoma characteristics including histologic type (tubular adenoma, villous adenoma, adenoma with dysplasia, sessile serrated lesion (SSL), advanced adenoma and adenocarcinoma) and size (< 5, 5–10, ≥ 10 mm) in individual colonic segments.
2.5 Outcome Measurements
The following measurements were calculated for each colonic segment and entire colon: Withdrawal time was calculated by subtracting the cecal intubation time from the total procedure time. Cecal intubation time was defined as the time for passage of the colonoscope from the rectum to the cecum. The times taken for biopsies, polypectomy, and cleaning mucosa (e.g., suctioning excess retained fluid) were measured and subtracted from withdrawal times [22]. The positive withdrawal time was defined as the mean withdrawal time of colonoscopies during which adenomas were detected. On the contrary, the negative withdrawal time was defined as the mean withdrawal time of colonoscopies during which non-adenomas were detected. PDR was defined as the number of colonoscopies detecting at least 1 polyp divided by the total number of colonoscopies [23]. ADR was defined as the number of colonoscopies detecting at least 1 adenoma divided by the total number of colonoscopies [23]. SDR, Serrated PDR (SDR), defined as the number of colonoscopies detecting any serrated polyps, such as hyperplastic polyp, sessile serrated adenoma/polyp, or traditional serrated adenoma, divided by the total number of colonoscopies [24]. APC was defined as the number of adenomas detected per colonoscopy [23]. Advanced adenoma was defined as any adenoma of 10 mm or greater in size, or containing villous histology, or with high-grade dysplasia [25].
2.6 Statistical Analysis
All analyses were performed using IBM SPSS version 26.0 (SPSS Inc., Chicago, Illinois, United States). Continuous variables were expressed as means ± standard deviation and categorical variables were expressed as numbers with percentages. Receiver operating characteristic (ROC) curves were used to determine the time threshold, sensitivity and specificity of each segment. Chi-square test or Fisher exact test were used for univariate analysis of ADR/PDR. Logistic regression analysis was used to analyze the differences affecting ADR/PDR of each colonic segment under different withdrawal time, adjusting the influence of confounding factors. A probability level of p < 0.05 was considered statistically significant.
3 Results
3.1 Demographics
A total of 586 patients (47.6% male, 52.4% female) were successfully examined by 29 endoscopists. The mean age of the patients was 56.38 ± 9.34 years. 86.2% of patients had a normal body mass index, which between 18.5–28 kg/m2. Among all the patients, 86.9% had excellent bowel preparation (bowel preparation scores of each colonic segment were all ≥ 2 points) and 13.1% had fair bowel preparation (as long as any part of colonic segment scores < 2 points). There were three main purposes of colonoscopy, 43.3% of patients underwent colonoscopy for screening, 23.7% for surveillance and 32.9% for diagnosis (Table 1).
| Characteristics | No. of patients | Percentage of patients(%) | |
|---|---|---|---|
| Age at colonoscopy, y | 18–49 | 138 | 23.5 |
| 50–69 | 389 | 66.4 | |
| 70–75 | 59 | 10.1 | |
| Sex | Male | 279 | 47.6 |
| Female | 307 | 52.4 | |
| Body mass index, kg/m2 | < 18.5 | 22 | 3.8 |
| 18.5–28 | 505 | 86.2 | |
| ≥ 28 | 59 | 10.1 | |
| Comorbidity | Hypertension | 154 | 26.3 |
| Diabetes mellitus | 45 | 7.7 | |
| Coronary heart disease | 26 | 4.4 | |
| Chronic lung disease | 12 | 2.0 | |
| Previous history of gastrointestinal neoplasms | 86 | 14.7 | |
| History of abdominal surgery | 169 | 28.8 | |
| Indication for colonoscopy | Screening | 254 | 43.3 |
| Surveillance | 139 | 23.7 | |
| Diagnosis | 193 | 32.9 | |
| Bowel preparation | Fair | 77 | 13.1 |
| Excellent | 509 | 86.9 | |
- Note: Bowel preparation [26]: Excellent: Bowel preparation scores of each colonic segment were all ≥ 2 points. Fair: As long as any part of colonic segment scores < 2 points. Segment scores of individual colonic defined as follows: Score 0: unprepared colon segment, mucosa not seen due to solid stool that cannot be cleared. Score 1: portion of mucosa of colon segment seen, but other areas of the segment not well seen due to staining, residual stool and/or opaque liquid. Score 2: minor amount of residual staining, small fragments of stool and/or opaque liquid, but mucosa of segment seen well. Score 3: entire mucosa of segment seen well with no residual staining, small fragments of stool and/or opaque liquid.
3.2 Respective Withdrawal Time and ADR in the Four Different Colon Segments
The general ADR of enrolled 586 patients was 38.2%. The positive withdrawal time (adenomas detected) was longer than negative withdrawal time (non-adenomas detected) (334.04 ± 24.21 s vs. 303.65 ± 5.20 s, t = 1.26, p < 0.001). ADR in ascending colon, transverse colon, descending colon and rectosigmoid colon were respectively 30.5%, 2.9%, 3.1% and 7.5% (Figure 2). While all of their positive withdrawal time were longer than negative withdrawal time (94.34 ± 33.76 s vs. 70.40 ± 41.84 s, t = 3.31, p = 0.001; 85.40 ± 49.76 s vs. 71.66 ± 36.87 s, t = 1.95, p = 0.025; 80.29 ± 39.85 s vs. 69.73 ± 35.96 s, t = 1.40, p = 0.016; 100.95 ± 55.92 s vs. 80.96 ± 42.87 s, t = 3.61, p < 0.001; respectively) (Figure 1). The positive withdrawal time in ascending colon was respectively shorter than that in rectosigmoid colon (94.34 ± 33.76 s vs. 100.95 ± 55.92 s, p < 0.001). While the ADR in ascending colon was obviously higher than that in other three segments of colon (30.5% vs. 2.9%, 3.1%, 7.5%, p < 0.001). The positive withdrawal time in rectosigmoid colon was longer than that in descending colon (100.95 ± 55.92 s vs. 80.29 ± 39.85 s, p < 0.001). However, there were no statistical differences between them in ADR (7.5% vs. 3.1%, p > 0.05).
3.3 Respective Withdrawal Time and ADR of Different Grades of Endoscopists
According to the whole colon, the mean withdrawal time was 302.46 ± 125.37 s for all the endoscopists regardless of their grades. Considering the grades of endoscopists, withdrawal times were 302.68 ± 123.49, 310.00 ± 125.31, 308.43 ± 129.30, 287.24 ± 120.41 s for Grade A, B, C1, C2 endoscopists, respectively (Table 2). It could be found that for the whole colon, the higher the endoscopists grade, the shorter the withdrawal time. Grade B endoscopists had the longest withdrawal time and the highest ADR, indicating that prolonged withdrawal time could increase ADR, this was also demonstrated in the SDR of the proximal colon, Grade B endoscopists had the highest SDR, but for Grade C1 and Grade C2 endoscopists, who had the same grade, their ADR and SDR were similar after reaching the appropriate withdrawal time threshold. However, the withdrawal time of Grade C2 endoscopists was significantly less than that of Grade C1 endoscopists, indicating that when the withdrawal time reached a certain threshold, the ADR was relatively constant, not the longer the withdrawal time, the higher the ADR. We also found that the detection rate of advanced adenoma of Grade C2 endoscopists was higher than that of Grade C1 endoscopists. We also found similar results by comparing the APC of different levels of endoscopists, Grade B endoscopists had highest APC, which was 0.94. Grade C1 endoscopists followed behind, which was 0.72. The APC of Grade A was lowest, which was 0.55 (Table 2).
| Endoscopists grades | No. of patients | Withdrawal time (s) | ADR (%) | PDR (%) | APC | Advanced adenoma (%) | SDR in the proximal colon (%) |
|---|---|---|---|---|---|---|---|
| Grade A | 38 | 302.68 ± 123.49 | 28.9 | 42.1 | 21/38 | 0.0 | 7.9 |
| Grade B | 166 | 310.00 ± 125.31 | 44.0 | 67.5 | 157/166 | 6.0 | 9.6 |
| Grade C1 | 215 | 308.43 ± 129.30 | 36.7 | 59.5 | 155/215 | 0.5 | 6.0 |
| Grade C2 | 167 | 287.24 ± 120.41 | 36.5 | 58.7 | 108/167 | 1.2 | 4.8 |
| Total | 586 | 302.46 ± 125.37 | 38.2 | 60.6 | 441/586 | 2.2 | 6.8 |
- Abbreviations: ADR, adenoma detection rate; APC, adenomas per colonoscopy; PDR, polyp detection rate; SDR, serrated polyp detection rate.
According to individual colon segment, the mean withdrawal times were 71.25 ± 42.11, 71.76 ± 38.14, 69.57 ± 36.57, 82.82 ± 45.67 s in the ascending colon, transverse colon, descending colon and rectosigmoid colon, respectively. Through analysis, we found that for individual colon segment, endoscopists grades also affected the withdrawal time. However, it was not the longer the withdrawal time, the higher the ADR, which reflected that individual colon segment had an appropriate withdrawal time threshold (Table 3).
| Endoscopists grades | Ascending colon | Transverse colon | Descending colon | Rectosigmoid colon | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Withdrawal time (s) | ADR (%) | PDR (%) | Withdrawal time (s) | ADR (%) | PDR (%) | Withdrawal time (s) | ADR (%) | PDR (%) | Withdrawal time (s) | ADR (%) | PDR (%) | |
| Grade A | 75.79 ± 56.49 | 18.4 | 21.0 | 74.37 ± 32.35 | 2.6 | 5.2 | 69.87 ± 30.98 | 0.0 | 0.0 | 82.66 ± 37.48 | 10.5 | 18.4 |
| Grade B | 73.33 ± 47.50 | 38.0 | 47.0 | 79.52 ± 42.77 | 3.0 | 9.0 | 71.29 ± 38.68 | 2.4 | 5.4 | 85.86 ± 41.25 | 5.4 | 25.9 |
| Grade C1 | 71.91 ± 38.99 | 27.4 | 32.5 | 70.70 ± 38.49 | 3.3 | 7.5 | 72.03 ± 39.48 | 5.4 | 11.4 | 86.84 ± 54.85 | 9.8 | 21.4 |
| Grade C2 | 67.32 ± 36.19 | 29.9 | 34.7 | 64.80 ± 32.45 | 2.4 | 8.4 | 64.62 ± 31.08 | 1.8 | 5.4 | 74.93 ± 31.70 | 6.0 | 19.2 |
| Total | 71.25 ± 42.11 | 30.5 | 36.5 | 71.76 ± 38.14 | 2.9 | 8.0 | 69.57 ± 36.57 | 3.1 | 7.2 | 82.82 ± 45.67 | 7.5 | 20.3 |
- Abbreviations: ADR, adenoma detection rate; PDR, polyp detection rate.
Through further analysis for pathological features of polyps in individual colon segment, including the size and shape of polyps (Table 4). We could find that polyps < 5 mm were relatively common in individual colonic segment, especially in the rectosigmoid colon. In terms of morphologic type, adenoma with dysplasia account for the largest proportion in all colonic segments.
| Clinicopathologic characteristics | Ascending colon | Transverse colon | Descending colon | Rectosigmoid colon | |
|---|---|---|---|---|---|
| Size, mm | < 5 | 31 | 22 | 19 | 79 |
| 5–9 | 31 | 25 | 25 | 52 | |
| ≥ 10 | 9 | 4 | 5 | 27 | |
| Morphologic type | Hyperplastic polyp (HP) | 22 | 9 | 14 | 48 |
| Adenoma with dysplasia | 38 | 30 | 27 | 74 | |
| Sessile serrated lesion (SSL) | 1 | 0 | 0 | 3 | |
| Advanced adenoma | 5 | 4 | 3 | 8 | |
| Adenocarcinoma | 3 | 1 | 0 | 3 | |
3.4 The Withdrawal Time Threshold of Individual Colon Segment
According to the ROC curve, Youden's index was the largest in the ascending colon segment, with a sensitivity of 72.73% and a specificity of 73.38% when the withdrawal time reached 77s. The withdrawal time threshold of transverse colon segment, descending colon segment and rectosigmoid colon segment were 61, 56 and 109 s, respectively (Table 5).
| Individual colon segment | AUC (95% CI) | Withdrawal time threshold (s) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
3.5 Lesion Detection Rates According to the Withdrawal Time Threshold
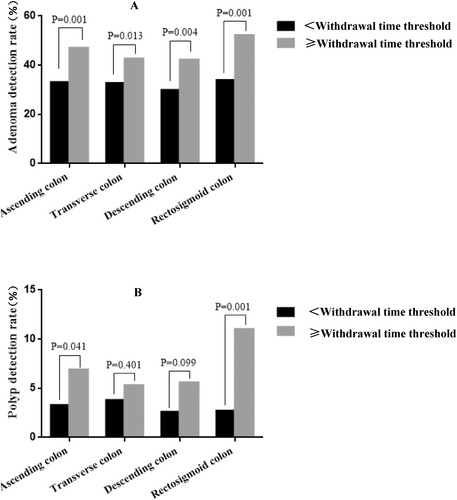
In the ascending colon segment, the ADR (47.0% vs. 33.1%, p < 0.001, Figure 3A), PDR (6.9% vs. 3.3%, p = 0.041, Figure 3B) were significantly higher when the withdrawal time was ≥ 77 s compared with < 77 s. After adjusting for age, sex, BMI, indication for colonoscopy and bowel preparation, Logistic regression analysis showed that the ADR (odds ratio [OR], 1.796; 95% confidence interval [CI], 1.273–2.532; p < 0.001), PDR (OR, 2.209; 95% CI, 1.014–4.812; p = 0.046) were significantly higher as well (Table 6).
| Withdrawal time threshold (s) | ADR | PDR | SDR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| < 77 vs. ≥ 77 | 1.796 | 1.273–2.532 | 0.001 | 2.209 | 1.014–4.812 | 0.046 | 5.020 | 2.453–10.274 | 0.001 |
| < 61 vs. ≥ 61 | 1.535 | 1.094–2.155 | 0.013 | 1.406 | 0.632–3.124 | 0.403 | — | ||
| < 56 vs. ≥ 56 | 1.722 | 1.193–2.486 | 0.004 | 2.248 | 0.838–6.029 | 0.108 | |||
| < 109 vs. ≥ 109 | 2.134 | 1.446–2.350 | 0.001 | 4.514 | 2.058–9.901 | 0.001 | |||
In the transverse colon segment, the ADR (42.7% vs. 32.7%, p = 0.013, Figure 3A) was significantly higher when the withdrawal time was ≥ 61 s compared with < 61 s. PDR (6.9% vs. 3.3%, p = 0.401, Figure 3B) were higher when the withdrawal time was ≥ 77 s compared with < 77 s, although there was not statistically significant. After adjusting for age, sex and BMI, Logistic regression analysis showed that the ADR (OR, 1.535; 95% CI, 1.094–2.155; p = 0.013) was significantly higher as well (Table 6).
In the descending colon segment, the ADR (42.3% vs. 29.9%, p = 0.004, Figure 3A) was significantly higher when the withdrawal time was ≥ 56 s compared with < 56 s. After adjusting for age, sex and BMI, Logistic regression analysis showed that the ADR (OR, 1.722; 95% CI, 1.193–2.486; p = 0.004) was significantly higher as well (Table 6).
In the rectosigmoid colon segment, the ADR (52.2% vs. 33.9%, p < 0.001, Figure 3A), PDR (11.0% vs. 2.7%, p < 0.001, Figure 3B) were significantly higher when the withdrawal time was ≥ 109 s compared with < 109 s. After adjusting for age, sex and BMI, Logistic regression analysis showed that the ADR (OR, 2.134; 95% CI, 1.446–2.350; p < 0.001), PDR (OR, 4.514; 95% CI, 2.058–9.901; p < 0.001) were significantly higher as well (Table 6).
4 Discussion
Although colonoscopy screening could effectively reduce the incidence and mortality of colorectal cancer, Lakoff et al. researchers [27] suggested that the incidence of malignant tumors in the distal colon was lower than that in the proximal colon among people who underwent colonoscopy screening in a 14-year follow-up study. Subsequently, several studies demonstrated that the proximal colon benefited less from colonoscopy than the distal colon. Follow-up findings by Jacob et al. [28] and Singh et al. [29] researchers even suggested that colonoscopy screening did not reduce mortality in the proximal colon cancer. In a multicenter study, the colonoscopy was rechecked after 4 years, the recurrence rate of adenoma in the proximal colon was significantly higher than that in the distal colon (RR = 1.52, 95% CI,1.15 ~ 2.02) [30]. In a retrospective study by Bressler [31], after 6 months to 3 years of colonoscopy, the new cases or missed diagnosis of colorectal cancer in the ascending colon, transverse colon, descending colon and sigmoid were 5.9%, 5.5%, 2.1% and 2.3%, respectively. Suggested that the proximal colon had a higher adenoma missed rate and it was one of the main reasons why the proximal colon had less benefits from colonoscopy. At the same time, ADR in the proximal colon (17.1%) was significantly higher than that in the distal colon (13.5%) (p = 0.001). The detection rate of sessile serrated polyps (SSL) in the proximal colon accounted for 75%–90% of the total colon [23, 32]. These all suggested that the withdrawal time of individual colonic segments should be formulated separately, especially the withdrawal time of the proximal colon should be increased to improve the ADR. At present, there are no studies on the withdrawal time of individual colonic segment in China. In foreign countries, there are few reports on making a reasonable withdrawal time threshold according to individual colonic segment.
Jung et al. researchers [33] studied the withdrawal time of the ascending colon, proximal colon and distal colon, they concluded that ADR (33.2% vs. 13.7%) and PDR (41.2% vs. 16.7%) of the ascending colon increased significantly when the withdrawal time was ≥ 2 min. When the withdrawal time of the proximal colon (including ascending colon and transverse colon) was ≥ 4 min, ADR (47.4% vs. 18.5%) and PDR (56.0% vs. 24.2%) were significantly increased as well. ADR (32.9% vs. 14.6%) and PDR (48.4% vs. 18.6%) were also significantly increased in the distal colon (including descending colon, rectosigmoid colon) when the withdrawal time was ≥ 3 min. This was basically consistent with the results of our study. In our study, colonic segments were further divided into the ascending colon segment, transverse colon segment, descending colon segment, rectosigmoid colon segment and the withdrawal time of each segment was defined precisely. At the same time, our retrospective study also confirmed that the appropriate withdrawal time could significantly improve the ADR and PDR of the whole intestine.
Studies had demonstrated that endoscopists experience, endoscopic equipment and bowel preparation conditions all had effects on ADR. Therefore, we selected experienced endoscopists, unified endoscopic equipment and all the patients had adequate bowel preparation to avoid the influence of the confounding factors on the results. However, in the clinical work, age, gender, endoscopists or different conditions of bowel preparation affected the ADR unavoidably. If endoscopists took exactly the same withdrawal time, which was > 6 min might cause potential misdiagnosis or unnecessary costs. In our study, the optimal withdrawal time derived from analysis is 303 s, which is less than the currently recommended normal examination time (ACG/ASGE 2024 recommends 480 s). The withdrawal time recommended by ACG/ASGE 2024 has a prerequisite, which is that when the adenoma detection rate (ADR) is less than 35%, the withdrawal time can be appropriately extended as a means to increase the ADR to an acceptable level. However, our study found that under the condition of ensuring an ADR generally greater than 35%, and considering the current situation in China (where there is a significant shortage of endoscopists compared to the vast number of patients awaiting examination), a withdrawal time shortened to 5 min is acceptable. Compared to a longer withdrawal time, the ADR at 5 min is not significantly lower than that at 6 min, and the missed lesions are mostly small polyps or non-high-risk adenomas. The time saved can benefit more patients, and a shorter withdrawal time can also reduce the risks associated with anesthesia. Additionally, some researchers have found that when ADR reached 20%, the withdrawal time of senior endoscopists was only 4 min, while that of junior endoscopists was 8 min [34]. And Zhao S, et al. suggested that 9-min WT (withdrawal time) offered benefit relative to 6-min WT for only less experienced colonoscopists (< 5000 colonoscopies) but not for experienced ones [35]. Therefore, we will further expand the sample size to explore the most appropriate withdrawal time for patients of different genders, ages and bowel preparation conditions.
The limitation of our study were as follows: (1) It was a single-center study with a small sample size; (2) The validation set was retrospective data, which was biased.
5 Conclusion
In conclusion, the ADR and PDR of individual colon segment and the whole colon were significantly increased when the withdrawal time of the ascending colon segment, transverse colon segment, descending colon segment and rectosigmoid colon segment were ≥ 77, 61, 56, 109 s, respectively. The ADR and withdrawal time are all various in individual colon segments. It is necessary to choose appropriate withdrawal time according to different colonic segments.
Ethics Statement
The protocol of this retrospective observational study was approved by the Clinical Research Ethics Committee of Wuxi People's Hospital on December 31, 2020 (approval number, KS202079).
Consent
All authors approved the final manuscript and the submission to this journal.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The datasets generated or analyzed during this study are available from the corresponding author on reasonable request.




