Clinical features of capsule endoscopy in young adults: A single-center retrospective study
Hui-Wen Xu and Yi-Ru Chen contributed equally to this work.
Declaration of conflict of interest: The authors declare that there is no conflict of interest regarding the publication of this paper.
Author contribution: Sen-Lin Zhu, Hui-Wen Xu, and Yi-Ru Chen contributed to the study design, draft, and critical revision of the manuscript. Hui-Wen Xu, Yi-Ru Chen, and Mei-Qian Wang collected and analyzed data. All authors read and approved the final manuscript.
Financial support: This work was funded by Guangzhou Science and Technology Development Funds (Key Program, No. 201803010103).
Abstract
Background and Aim
Capsule endoscopy (CE) has been used in clinical examination among people of various ages, while few studies exclusively focused on the young. We aimed to explore its clinical features in young adults and those with obscure gastrointestinal bleeding (OGIB).
Methods
A total of 479 young adults aged 18–44 years were analyzed, with median age of 33 years. Primary positive findings of patients were classified into four kinds of lesions, and potential risk of bleeding among patients with OGIB was assessed based on Saurin classification (P0-2 lesions).
Results
The overall completion rate and diagnostic yield of CE among young adults were 89.77 and 77.04%, respectively. Significant differences were found among overall completion rate/diagnostic yield and inpatient status/CE brand. Positive diagnostic yield among 157 patients with OGIB was 51.59% (P1-2 lesions), and the significant risk of bleeding was 37.04% (P2 lesions). Among patients with OGIB in which 134 patients with a total of 216 lesions, ulceration was the commonest P2 lesions, followed by angioectasia and telangiectasia. Inpatient rate, completion rate, and diagnostic yield were higher among patients with overt OGIB, and disease categories of overt OGIB were different compared with occult OGIB.
Conclusion
CE is an optimal tool for discovering lesions in young adults and could play a role in evaluating the bleeding risk of young adults with OGIB.
Introduction
Capsule endoscopy (CE) has been used in clinical examination of small bowel diseases, especially obscure gastrointestinal bleeding (OGIB), due to its visualization and minimal invasiveness.1, 2 A meta-analysis consisting of 20 prospective studies concluded that the incremental yield of CE was 30% compared with small bowel barium radiography and push enteroscopy for diagnosing clinically significant findings in patients with OGIB.3 Some research studies have divided the population into four groups: young adults ≤44 years old, middle-aged adults between 45 and 64 years of age, young-old adults between the 65 and 74 years of age, and older adults ≥75 years old.4, 5
Zhang et al. found that there were no differences in diagnostic yield of CE among three age groups with OGIB, young adults (17–40 years), middle-aged (41–65 years), and elderly (>65 years), but pathological changes in each age group were significantly different. The young adults group was most likely to have Crohn's disease, small intestine tumors, or non-specific enteritis.6 CE was feasible in over-80-year-old patients with OGIB, and small bowel angiodysplasia lesions were more frequent during this population compared with matched younger group with 63.4 ± 14.5 years.7
On the other hand, in other studies, diagnostic yield of OGIB was significantly higher in >65 years old group8 and ≥75 years old group.9 In a retrospective and multicenter study, Yung et al. analyzed 220 young patients with iron deficiency anemia between 19 and 50 years, and found that both weight loss and lower mean corpuscular volume were associated with higher diagnostic yield for perilous pathology.10 The above findings show that different age groups have different characteristics of intestinal disease. We notice that few CE studies merely focused on young adults and those with OGIB.
Methods
Inclusion and exclusion criteria
It is introduced that there are studies that divide the population into four age groups in the introduction, and there are many studies on CE in the elderly. It is worth noting that not much attention has been paid to young and middle-aged people. In addition, the number of young adults in the data we collected was the most, so we selected people between 18 and 44 years.
Inclusion criteria for the study were as follows: (i) age of 18–44 years; (ii) inability of gastroscopy or colonoscopy to identify lesions that could explain the main symptoms during the attack period. Patients exhibiting any of the following were excluded: (i) history of abdominal surgery; (ii) incomplete medical records of transit time, such as gastric transit time (GTT) and small bowel transit time (SBTT).
From 29 September 2002, to 2 July 2019, 479 patients who underwent CE examination in our tertiary medical center were eligible for the designed single-center retrospective study. The Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University approved this study.
CE procedure
CE procedure was usually performed in the morning. Patients were instructed to consume a light liquid diet at least 12 h prior to examination, followed by overnight fasting. Patients were also instructed to take 50 g of mannitol at 20:00 and 22:00 h on the evening prior to examination and to drink over 1500 mL of water. An antifoaming agent was administrated 30 min prior to swallowing capsule.
All patients confirmed their understanding of CE procedure and provided written informed consent aimed at this procedure. Patients underwent examination using PillCam (Given, Israel) (n = 174), OMOM (Chongqing, China) (n = 95), and MiroCam (Intromedic, Seoul, Korea) (n = 210) devices.
Study outcomes
In the present study, we collected the relevant data of young adults from paper CE examination records preserved in our hospital, calculated the overall completion rate and diagnostic yield, and evaluated the bleeding risk of patients with OGIB. These observed clinical features of young adults in our study could benefit the clinical application of CE.
The primary outcomes were positive findings, which were defined as the presence of depicted lesions on paper medical records, including four categories: neoplastic lesions (e.g. gastrointestinal stromal tumors, leiomyoma and mass lesions, etc.) and vascular lesions (e.g. angioectasia, telangiectasia and angioma, etc.),11 inflammatory lesions (e.g. erosion, ulceration, erythema, gastritis, duodenitis, jejunitis, ileitis, Crohn's disease, etc.), other lesions (e.g. diverticulum, submucosal nodule, ileal lymphoid follicular hyperplasia, polyp, stricture-causing lesions, etc.).3, 12, 13 Regardless of the number of lesions, both location and category of lesions were combined to make a qualitative record.
Furthermore, potential risks of bleeding among young adults with symptoms of OGIB were assessed according to Saurin classification (P0-2 lesions), and significant risks were relied on P2 lesions. P0 lesions such as diverticula and nodules have no potential for bleeding, P1 lesions like red spots and erosions have uncertain risk, and P2 lesions were regarded as a significant risk of bleeding, including tumors, varices, angioma, and ulceration.14 Besides, positive diagnosis of patients with OGIB was defined as P1 and P2 lesions that could explain the etiology of OGIB.14 As secondary outcomes, passing the ileocecal valve was defined as completion of CE, and SBTT ranged from the time of the first photo of duodenum to the photo of ileocecal valve.15
Statistical analysis
SPSS v25.0 (New York, NY, USA) and GraphPad Prism v8.0.2 (San Diego, CA, USA) were used for statistical analysis and graphing. Categorical data were tested by χ2 test, such as overall completion rate and diagnostic yield. Two independent samples t test and one-way anova were used for numerical variables like SBTT. P value <0.05 (two-sided test) was considered significant difference.
Results
Clinical characteristics of the study population
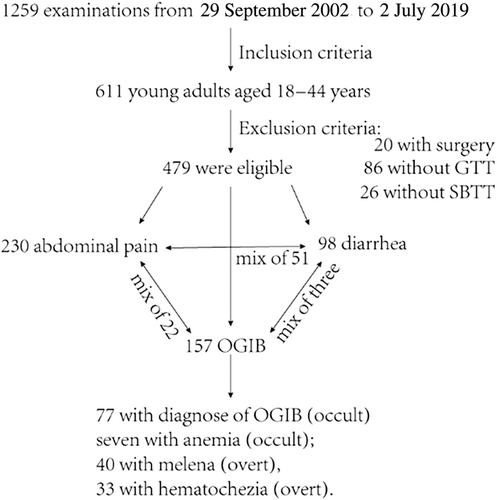
Among 479 young adults analyzed in our study, 160 were women, while 319 were men, and the median age was 33 years (interquartile range: 26–39). Among the analyzed population, 196 (40.92%) were hospitalized patients. The cost of gastroenteroscopy is further cheaper than invasive enteroscopy or noninvasive CE, and it is recommended to conduct gastroenteroscopy first and again. All people performed gastroscopy and colonoscopy prior to CE, while few conducted enteroscopy. The total number of three examinations was 588, 526, and 15, respectively. Patients presented with symptoms of abdominal pain, diarrhea, and OGIB were 230, 98, and 157, respectively (Fig. 1).
Regarding clinical characteristics of young adults aged 18–44 years (Table 1), a total of 430 examinations (89.77%) passed ileocecal valve, indicating completion of CE. There was no significant difference in the overall completion rate based on sex (P = 0.906). Notably, the overall completion rate among inpatients was significantly lower than that among outpatients (86.22 vs 92.23%, P = 0.033). In addition, there was a significant association between overall completion rate and CE brand (P = 0.002).
| Completion rate (89.77%) | Diagnostic yield (77.04%) | |||||
|---|---|---|---|---|---|---|
| Total (479) | Unfinished (28) | Completed (129) | P | Negative findings (23) | Positive findings (134) | P |
| Sex | 0.906 | 0.688 | ||||
| Women (160) | 16 (10.00%) | 144 (90.00%) | 35 (21.88%) | 125 (78.12%) | ||
| Men (319) | 33 (10.34%) | 286 (89.66%) | 75 (23.51%) | 244 (76.49%) | ||
| Hospitalization | 0.033 | 0.027 | ||||
| Outpatient (283) | 22 (7.77%) | 261 (92.23%) | 75 (26.50%) | 208 (73.50%) | ||
| Inpatient (196) | 27 (13.78%) | 169 (86.22%) | 35 (17.86%) | 161 (82.14%) | ||
| Brands | 0.002 | <0.001 | ||||
| PillCam (174) | 26 (14.94%) | 148 (85.06%) | 60 (34.48%) | 114 (65.52%) | ||
| OMOM (95) | 13 (13.68%) | 82 (86.32%) | 28 (29.47%) | 67 (70.53%) | ||
| MiroCam (210) | 10 (4.76%) | 200 (95.24%) | 22 (10.48%) | 188 (89.52%) | ||
- Bold font indicates P < 0.05.
Positive findings were detected in a total of 369 young adults, with an overall diagnostic yield of 77.04%. There was no significant association between overall diagnostic yield and sex (P = 0.688). Overall diagnostic yield was significantly higher among inpatients than outpatients (82.14 vs 73.50%, P = 0.027). We also observed a significant association between overall diagnostic yield and CE brand (P < 0.001).
The mean and SD of SBTT was 306.45 ± 106.20 min across all 479 capsule examinations. SBTT data were split according to sex, and the split data exhibited a normal distribution. There were no significant differences in SBTT based on sex (P = 0.555). The mean of SBTT among inpatients was statistically equal to that among outpatients (P = 0.595). We also conducted a one-way anova to examine the effect of CE brand on SBTT, and no significant differences existed in the mean SBTT of the three brands (F = 0.876, P = 0.417). The analyses of SBTT among young adults or those with OGIB are shown in Table S1.
Clinical of features patients with OGIB
These 157 patients (44 women, 113 men) with OGIB presented a mean and SD SBTT of 317.96 ± 119.35 min, with 96 (61.15%) patients in hospital. Initial diagnosis descriptions prior to CE procedure were as follow: 77 with diagnosis of OGIB, seven with anemia, 40 with melena, and 33 with hematochezia (Fig. 1). Thus, 84 with occult and 73 with overt OGIB were found in our study. However, to our surprise, only a significant association between overall completion rate and CE brand (P = 0.029) was found when observing clinical features of patients with OGIB (Table S2).
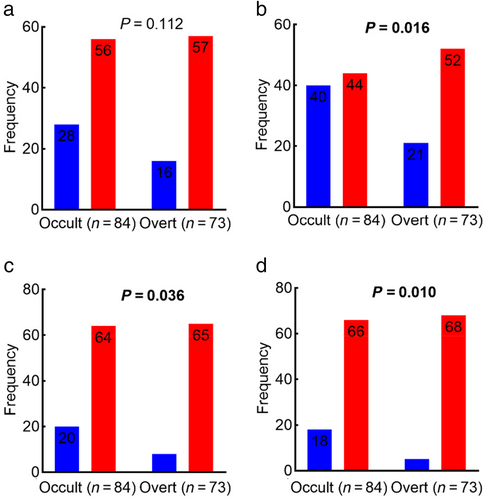
As young adults with OGIB were divided into two groups based on manifestation of occult or overt (Fig. 2), no significant association between OGIB and sex was found (P = 0.112). However, the inpatient rate of overt OGIB was higher than that of occult OGIB (71.23 vs 52.38%, P = 0.016). In addition, both completion rate and diagnostic yield were higher among patients with overt OGIB (89.04 vs 76.19%, P = 0.036; 93.15 vs 78.57%, P = 0.010).
 ), Women; (
), Women; ( ), men. b: (
), men. b: ( ), outpatient; (
), outpatient; ( ), inpatient. c: (
), inpatient. c: ( ), unfinished; (
), unfinished; ( ), completed. d: (
), completed. d: ( ), negative findings; (
), negative findings; ( ), positive findings.
), positive findings.There was no significant difference in SBTT between occult OGIB and overt OGIB (P = 0.964). Similarly, there was no significant difference in SBTT among patients with OGIB based on sex (P = 0.552). The mean SBTT of inpatients was statistically comparable to that of outpatients (P = 0.347). There were no significant differences in the mean SBTT of the three brands (F = 2.242, P = 0.110).
Distribution of lesions found in patients with OGIB
We identified 134 patients with a total of 216 lesions (meaning a detection rate of 85.35%), of which 18 patients with active bleeding, 13 cases with neoplastic lesions, and plenty of vascular lesions including 20 with angioectasia, 14 with telangiectasia, and four with angioma. Besides, many inflammatory lesions were conformed (e.g. two with erosion, 29 with ulceration, three with erythema, four with gastritis, eight with duodenitis, one with jejunitis, five with ileitis, 14 with Crohn's disease, etc.). Other lesions were also found (17 with diverticulum, seven with submucosal nodule, seven with ileal lymphoid follicular hyperplasia, six polyp, four with stricture-causing lesions, etc.).
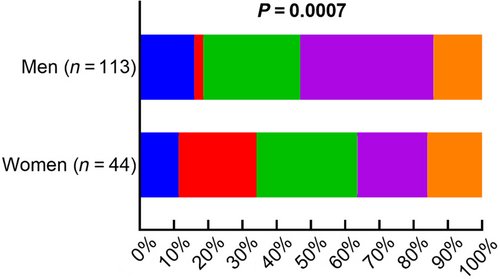
Inflammatory lesions were the most common, followed by vascular lesions and other lesions as defined above. There was a significant association of disease categories with sex (P = 0.0007, Fig. 3), but not with inpatient status (P = 0.4816). Neoplastic lesions were obviously more frequent in women (22.73 vs 2.66%), while inflammatory lesions were less common in women (20.46 vs 38.94%). In addition, disease categories of occult OGIB were significantly different from that of overt OGIB (P < 0.0001, Fig. 4).
 ), Other lesions; (
), Other lesions; ( ), inflammatory lesions; (
), inflammatory lesions; ( ), vascular lesions; (
), vascular lesions; ( ), neoplastic lesions; (
), neoplastic lesions; ( ), negative findings.
), negative findings.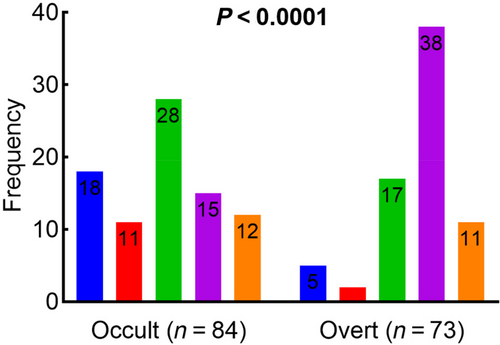
 ), Negative findings; (
), Negative findings; ( ), neoplastic lesions; (
), neoplastic lesions; ( ), vascular lesions; (
), vascular lesions; ( ), inflammatory lesions; (
), inflammatory lesions; ( ), other lesions.
), other lesions.According to Saurin classification and identified lesions among patients with OGIB, Table 2 shows the distribution among depicted location and category of lesions. Five patients had only P1 lesions, three erythema, and two erosion. Among 76 patients represented with 80 P2 lesions, ulceration (36.25%) was the most common, followed by angioectasia (25.00%), telangiectasia (17.50%), and tumor (16.25%). Therefore, positive diagnostic yield among 157 patients with OGIB was 51.59% (P1-2 lesions). Having divided 80 P2 lesions by 216 total lesions, the significant risk of bleeding among young adults with OGIB was as high as 37.04%.
| Saurin classification | Duodenum | Jejunum | Ileum | Small intestine | Other sites |
|---|---|---|---|---|---|
| Neoplastic lesions (13, P2) | — | 2 | 1 | 6 | 4 |
| Vascular lesions (38) | |||||
| Angioectasia (20, P2) | 5 | 1 | 2 | 7 | 5 |
| Telangiectasia (14, P2) | 1 | 2 | — | 7 | 4 |
| Angioma (4, P2) | — | 1 | 1 | 1 | 1 |
| Inflammatory lesions (34) | |||||
| Ulceration (29, P2) | 4 | 1 | 9 | 15 | — |
| Erosion (2, P1) | 1 | 1 | — | — | — |
| Erythema (3, P1) | — | — | — | 2 | 1 |
| Other lesions (24) | |||||
| Diverticulum (17, P0) | 1 | 2 | 6 | 3 | 5 |
| Submucosal nodule (7, P0) | — | — | — | 2 | 5 |
Discussion
We gained clinical characteristics of CE in 479 young adults between 18 and 44 years of age, and found that the overall completion rate and diagnostic yield of CE were 89.77 and 77.04%, respectively. The former is similar to that with 81.30% observed in a systematic review, while the latter is higher than that with 59.40%.15 The reason may be the high inter-observer variability of the main presenting symptom: young adults with abdominal pain were the major in our study, while the majority were patients with OGIB in the previous research.
Significant differences among overall completion rate/diagnostic yield and inpatient status/CE brand in our study were interesting. The finding of the overall completion rate higher in outpatients was consistent with recommendation 2 of ESGE.16 Overall diagnostic yield higher in inpatients was in accordance with the previous study.17 The significant differences in the three brands might result from heterogeneity that existed in the whole CE procedure. There also were differences in overall completion rate and diagnostic yield between MiroCam capsule set at 3 frames per second and PillCam capsule set at 2 frames per second.18 However, although Pillcam SB3 and OMOM devices have significant differences in battery life and download time, no differences were found in overall completion rate and diagnostic yield.19 Therefore, the interesting phenomena are worthy of further research.
On the other hand, SBTT is an important parameter in CE examination. A large sample multicenter study on patients with OGIB found that the longer the SBTT, the higher the positive diagnostic yield of significant lesions via CE.20 An SBTT ≥4 h may be more likely in patients with angioectasia, single lesions, and jejunal lesions, which could result in small bowel bleeding.21 Longer SBTT could independently identify the highly potentially bleeding P2 lesions with higher possibility.22 In our study, the mean SBTT was 306.45 min, and 73.90% of examinations exceeded 4 h, together with a similar overall completion rate and diagnostic yield, which implied reasonable research on patients with OGIB.
Among young adults with OGIB in our study, positive diagnostic yield was 51.59% relied on P1-2 lesions, and significant risk of bleeding was as high as 37.04% according to only P2 lesions. In the previous research,10 based on at least one P2 finding, a similar diagnostic yield of 32.3% was found. Singeap et al. found that an overall diagnostic yield of 62% was in the 224 sample size for OGIB, and diagnostic yield was higher in overt OGIB compared with iron deficiency anemia. They discovered significantly different positive findings between the two groups.23 Consistently, in the present study, the diagnostic yield was higher in overt OGIB, and disease categories of young adults with symptoms of occult or overt OGIB were different. Inflammatory lesions were more frequent in the overt group.
In addition, ulceration lesions were the most common among patients with P2 lesions, followed by angioectasia and telangiectasia. The finding of ulceration was consistent with a meta-analysis that has already identified ulceration lesions as the cardinal lesion for OGIB in patients from Eastern countries.24 Angioectasia is located in mucosal and submucosal layers of the intestine, with little or no smooth muscle. Telangiectasia is lack of capillaries, directly connecting arteries to veins, and has excessive layers of smooth muscle without elastic fibers.11 Besides, ischemia or infiltration of neoplastic lesions could result in small intestine bleeding.11 Angioectasia belonging to P2 lesions with high risk of bleeding is a major cause of small bowel bleeding, and its main location is proximal small intestine.25
In the present study, we also noticed that 18 patients with active bleeding, meaning that those might require more aggressive healthcare. CE is feasible and safe to facilitate patient triage and earlier endoscopic surgery for people presenting with acute upper gastrointestinal hemorrhage in an emergency department setting.12 A high diagnosed yield was gained in patients with OGIB through early video CE, and the incidence of re-bleeding within 1 year after treatment was significantly reduced, indicating that timely and accurate diagnosis can help improve treatment and prognosis.26 Besides, the comparative results on OGIB between CE and enteroscopy are complex and contradictory, CE with higher rate than entheroscopy27, 28 or a higher rate in the latter,29-31 and a combination of them has complementary clinical effects.32, 33
Moreover, we found 23 patients with negative findings, meaning an intestinal lesion could be roughly precluded to a certain extent. It is worth noting that repeated CE could have about 75 rate of new findings in patients with persistent OGIB when the initial study is negative or inconclusive.32, 34 Young patients present with overt bleeding were considered to have further examination for re-bleeding, although with a result of negative CE initially.35 In a systematic review and meta-analysis including 26 studies on OGIB, research has drawn a conclusion that a negative finding provides sufficient evidence of a subsequent rate of re-bleeding (19%).36
However, we also have some limitations, such as a single-center retrospective design, small sample size study, and selection bias. Thus, further multicenter prospective studies are required to obtain more comprehensive evidence regarding the features of CE in young adults, especially those with OGIB.
In summary, the present research found both overall completion rate and diagnostic yield of approximately 80% in 479 young adults via CE examination. Overall completion rate higher in outpatients and diagnostic yield higher in inpatients were found. The positive diagnostic yield of young adults with OGIB was 51.59% (P1-2 lesions), and the significant risk of bleeding was 37.04% (P2 lesions). Besides, ulceration, angioectasia, and telangiectasia were the three common P2 lesions. Moreover, inpatient rate, completion rate, and diagnostic yield were higher among patients with overt OGIB, and disease categories of overt OGIB were significantly different from that of occult OGIB. Thus, CE is an alternative tool for finding lesions in young adults, and could evaluate the bleeding risk of young adults with OGIB. The observed clinical features of young adults in our study could increase the clinical value of CE.
Acknowledgment
The authors sincerely appreciate the medical personnel who participated in collecting, processing, and saving medical information of patients in the examination of small bowel capsule endoscopy in The First Affiliated Hospital of Sun Yat-sen University.




