Combined hepatocellular carcinoma–cholangiocarcinoma: A misdiagnosed case preoperatively
Declaration of conflict of interest: The authors declare no competing interests.
Author contribution: Lei Ding and Zeming Hu designed the study, and drafted the report. Wang Hu, Qingrong Wu, Zhiqiang Hu, Jianhong Zhang, and Lihui Jiang prepared the figure, did the literature search, and interpreted data. Zeming Hu critically reviewed the report. Informed consent was obtained from the patient to publish these images.
Graphical Abstract
Combined hepatocellular carcinoma-cholangiocarcinoma (cHCC-CC) is a rare subtype in primary liver cancer, which is difficult to diagnose in clinics. In this report, we present a case of a 62-year-old male with abdominal pain and slightly elevated alpha-fetoprotein. The contrast-enhanced computed tomography scans showed a left liver mass, which showed adherence to the imaging characteristics of hepatocellular carcinoma. However, with the treatment of laparoscopic liver resection, the following histological examination displayed two distinct components, which were consistent with the diagnosis of cHCC-CC.
Case report
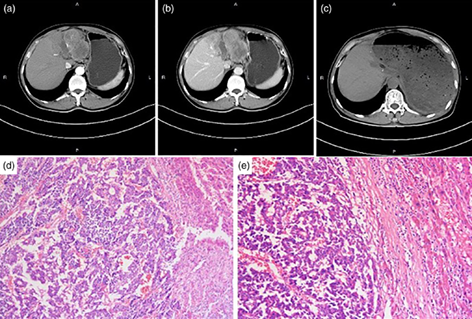
A 62-year-old man with a 6-year history of hepatitis B virus infection presented with a 2-month history of persistent upper abdominal discomfort but worsening for a week, and he was admitted to our department. Laboratory findings revealed his serum alpha-fetoprotein was mildly elevated at 21, 312 ng/mL, and his hepatitis B serology was positive. Serum liver function tests were within the normal limits except for the slightly elevated alanine aminotransferase (250 U/L) and aspartate aminotransferase (210 U/L). Abdominal contrast-enhanced computed tomography (CT) scans revealed a destructive lesion that showed enhancement during the hepatic arterial phase (Fig. 1a) and rapid washout during the portal venous phase (Fig. 1b) in the left liver lobe, which was most likely consistent with hepatocellular carcinoma (HCC).
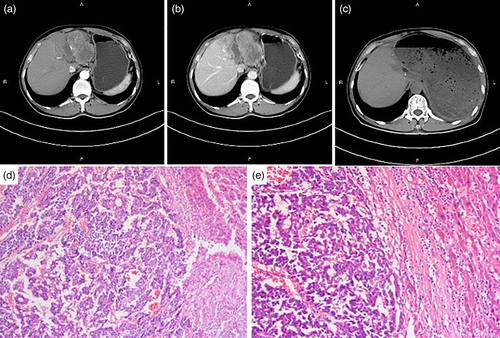
However, the patient has subsequently performed a laparoscopic left hepatectomy and his pathology examination indicated the specimen was poorly differentiated and displayed two distinct components: one with HCC-like feature and the other with cholangiocarcinoma (CC) pattern (Fig. 1d,e). Further immunohistochemical staining confirmed the diagnosis of combined hepatocellular carcinoma–cholangiocarcinoma (cHCC-CC). The postoperative course was without severe complications and the patient was discharged 15 days after surgery. During the subsequent follow-up for 1 year since surgery, the patient remains well without any signs of recurrence (Fig. 1c).
Discussion
cHCC-CC is a relatively rare entity of primary liver malignancy, with incidence widely varying among regions.1 It is frequently misdiagnosed in the preoperative setting as either HCC or CC because the clinic characteristics and imaging features often mimic those of HCC or CC.2 The lesion in the liver shows typical radiological characteristics of HCC, which presents diagnostic challenges of cHCC-CC to the radiologist and surgeon. Indeed, the recent consensus recommends that immunohistochemistry staining is not a prerequisite for the diagnosis of cHCC-CC, while that morphology is the key.3 Thus, preoperative ultrasound- or CT-guided biopsy and histopathology analysis, especially for the tumor morphology, should be highlighted in diagnosis.
Acknowledgment
We would like to acknowledge Prof. Jun Min who came from The Second Affiliated Hospital of Sun Yat-Sen University that participated in the operation.