Neonatal birthweight prediction using two- and three-dimensional estimated fetal weight among borderline small fetuses
Abstract
Purpose
This study aimed (1) to determine the degree of correlation between 2D and 3D estimated fetal weight (EFW) and neonatal birth weight (BW) among borderline small fetuses and (2) to compare the accuracy and precision of 2D and 3D EFW in BW prediction.
Methods
A retrospective cohort study evaluated fetuses who had an ultrasound performed between January 2017 and September 2021 at a tertiary maternal center. All singleton pregnancies with 3D EFW within 4 weeks of delivery were included. Fetuses with known structural or genetic abnormalities were excluded. Pearson's correlation coefficients were determined for both 2D and 3D EFW to BW then compared using Williams' test and Fisher r to z transformation, where applicable. Mean percent difference and standard deviation were used to assess the accuracy and precision, respectively, of 2D and 3D EFWs in BW prediction.
Results
Two hundred forty-eight pregnancies were included. Ultrasound studies were performed with a median interval of 2 weeks (IQR 1, 3) between ultrasound and delivery. Both 2D and 3D estimated fetal weights showed a significant correlation with birth weight (r = 0.74 and r = 0.73, respectively), indicating similar accuracy between the two techniques.
Conclusion
Two-dimensional and three-dimensional EFWs performed similarly in the prediction of BW in borderline small fetuses.
1 INTRODUCTION
Sonographic fetal age and weight estimates have become standardized tools to guide pregnancy management. Initial methods for fetal age and/or weight determination incorporated fetal measurements obtained from traditional, two-dimensional (2D) imaging planes of the biparietal diameter (BPD), the head circumference (HC), the abdominal circumference (AC), and the femur length (FL).1, 2 Hadlock et al. and others used these parameters to create computer-generated formulas to estimate fetal weight.1, 2 Despite the continued use of 2D parameters for estimations of fetal weight, up to 15% error between the 2D estimated fetal weight (2D EFW) and neonatal birthweight (BW) has been shown.2, 3
Understanding that up to 46% of the variance in neonatal BW is attributable to differences in neonatal fat mass, techniques that incorporate sonographic measurements of fetal subcutaneous tissue were introduced.4-14 Three-dimensional (3D) ultrasonography, which incorporates subcutaneous tissue measurement, has been proposed as an alternative method for fetal weight estimation since the 1990s to address inherent errors of standard 2D methods.6-15 Techniques, such as the fractional limb volume technique, were introduced as methods to decrease image capture time and inter- and intra-observer variability while maintaining clinical accuracy.16-18 These 3D methods of fetal weight estimation have been found to perform at least similarly, if not better, than standard 2D methods among fetuses with normal and accelerated fetal growth patterns.9, 10, 15, 19-24 Prior studies assessing 3D fetal biometry in small fetuses have been limited to small populations, consisting largely of fetuses with extreme growth restriction, and have provided conflicting results on the utility of BW prediction when compared to 2D methods.18, 25, 26
Low neonatal birthweight has been established as a predictive factor for adverse neonatal, infant, child, and adult outcomes.27-36 Other measures of neonatal composition, which include soft tissue components, have been proposed as predictors for neonatal nutritional status and associated adverse outcomes.28, 30-37 This suggests clinical utility in the evaluation of fetal soft tissue mass via 3D fetal weight estimation; therefore, this study aimed to assess the degree of correlation between 2D and 3D EFW with BW in fetuses with 2D EFW < 20th, but >10th percentile, for GA.
2 MATERIALS AND METHODS
A retrospective cohort study evaluated ultrasounds performed between January 2017 and September 2021 at a tertiary maternal care center. Study approval was obtained from the MetroHealth Institutional Review Board (#IRB21-00671). All complete obstetric (CPT code 76805), detailed fetal anatomic (CPT code 76811), and follow-up (CPT code 76816) ultrasound studies performed during this period were reviewed. During this time, institutional practice recommended 3D EFW measurement borderline small fetuses, that is, fetuses with standard, 2D EFW and/or an abdominal circumference (AC) measuring <20% but >10% for gestational age (GA) by Hadlock. Pregnancies that had at least one 3D EFW obtained were reviewed for inclusion. Maternal, fetal, sonographic, obstetric, and neonatal outcomes were abstracted and stored within the MetroHealth REDCap database.38, 39 The 2D EFW was obtained using the sonographic technique described by Hadlock et al.1, 2 The 3D EFW was obtained using the sonographic technique described by Lee et al.15, 19, 24
2.1 Study population
Pregnant individuals with singleton gestations and a 3D EFW of a live fetus obtained ≤4 weeks prior to delivery were included. Pregnancies were excluded for the following: gestational dating performed ≥16 weeks gestation, structural, or genetic anomaly diagnosed in the fetus, missing fetal weight calculations, and/or delivery occurred outside of the MetroHealth System. Among individuals with more than one pregnancy meeting eligibility criteria within the defined timeframe, the earliest pregnancy was selected for inclusion. In pregnancies where more than one growth ultrasound was performed ≤4 weeks from delivery, the ultrasound with the shortest interval to delivery was included for analysis.
2.2 Image acquisition
Fractional thigh volumes were acquired using the automated described by Lee et al.19, 24 Three-dimensional thigh volumes were all obtained using GE Voluson models E8 and/or E10. The thigh volume was obtained using a convex volume transducer. A 2D planar, sagittal view was obtained of the fetal thigh closest to the transducer—most anterior fetal thigh. The 2D image of the fetal thigh was set to consume approximately two-thirds of the imaging screen. A 3D sagittal sweep was obtained. The fractional thigh volume was obtained using the commercially available GE imaging package (4D View 5.0, GE Healthcare) that automatically detects the femoral diaphyseal ends and automatically determines 50% of the diaphyseal length. This proportion of the fetal thigh was divided into five equidistant, transverse planes along the mid-section of the fetal thigh. Color filters and alterations in brightness and contrast were utilized to optimize the transverse plane images. The trace function was used to manually trace the circumference of the fetal thigh soft tissue in each of the five transverse, 2D planar images.
Prior to implementation of this practice, all sonographers within The MetroHealth Center Fetal Diagnostic Center underwent 3 months of onsite training with oversight from senior sonographers and maternal–fetal medicine staff which incorporated instruction on 3D fractional thigh volume acquisition.
2.3 Statistical methods
The primary endpoint was the degree of correlation between 3D EFW and BW when assessed within 4 weeks of delivery. It was hypothesized that 3D EFW would demonstrate a high degree of correlation (r ≥ 0.5) with BW. The secondary endpoints were to compare (1) the correlation of 3D EFW with BW to the correlation of 2D EFW with BW; (2) the proportion of EFW predicted within 5% and 10% of BW between 3D and 2D EFW techniques, and (3) the systematic error (accuracy) and random error (precision) between 3D and 2D EFW for BW prediction.
Counts (%) and medians (interquartile range, [IQR]) were performed for the study population, where applicable. Three-dimensional EFW (g; x-axis) were plotted against BW (g; y-axis). Residuals were plotted to test the assumptions of linearity, independence, normality, and equal variance of the predictor variables. Linear regression was performed to confirm associations with BW. Pearson's correlation coefficient (r) was calculated. This process was repeated for 2D EFW (g) and BW (g).
The Pearson's coefficients for 3D EFW versus BW and 2D EFW versus BW were compared using Williams' test for comparison of coefficients from two, dependent, overlapping samples. A p-value of <0.05 was used to indicate significance. Maternal body mass index (BMI, kg/m2) and interval (weeks) between the last ultrasound and delivery were established a priori as covariates. Linear regression was then performed to assess relationship of predetermined covariates on the degree of correlation between 3D EFW and BW and 2D and BW. Pearson's coefficients were adjusted for significant covariates. For individual comparisons of Pearson's coefficients, Fisher's r to z transformations were used to compare correlation coefficients of two, independent, non-overlapping samples. The obtained z scores were then compared using the z statistic with p-value of <0.05 indicating significance.
A percent difference from BW was calculated as BW subtracted from EFW, divided by BW, and multiplied by 100. Systematic error was calculated as mean percent difference of EFW from BW. Random error was calculated as the standard deviation of mean percent difference of EFW from BW. This was performed for both 3D and 2D EFW. The mean percent differences were compared between 3D EFW and 2D EFW using Student's t test for paired. The proportions of pregnancies with percent difference EFW to BW ≤5% and ≤ 10% between 3D and 2D EFW were compared using Chi-squared tests.
3 RESULTS
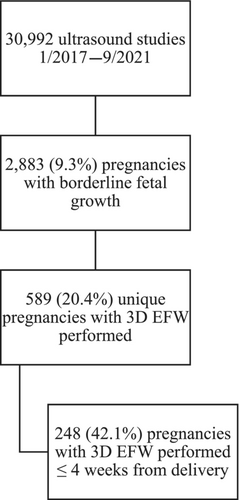
Between January 2017 and September 2021, 30 992 anatomic and follow-up ultrasound studies were reviewed, from which 2883 pregnancies had borderline small fetuses (Figure 1). Five hundred and eighty-nine pregnancies met eligibility criteria and had 3D EFW performed. Two hundred forty-eight of these pregnancies (42.1%) had a 3D EFW performed ≤4 weeks from delivery. Baseline maternal characteristics of the studied pregnancies are listed in Table 1. Notable maternal comorbidities among the pregnancies studied included substance use (64%), chronic hypertension (17%), and pre-existing diabetes (2%). Hypertensive disorders of pregnancy were diagnosed in 17% of the pregnancies studied. Gestational age at delivery ranged from 25 to 41 weeks' gestation with median gestational age of 38 (37, 39) weeks at delivery. Preterm delivery at <37 weeks and at <34 weeks occurred in 17% and 3.6% of the pregnancies studied, respectively.
| All (n = 248) | |
|---|---|
| Maternal characteristics | |
| Age at delivery (years) | 26 (22,30) |
| Body mass index (BMI, kg/m2) at first prenatal visit | 26 (22, 32) |
| Insurance | |
| Private | 36 (15%) |
| Government-based | 186 (75%) |
| Other | 26 (10%) |
| Gravida | 2 (1,4) |
| Nulliparous | 96 (39%) |
| Chronic hypertension | 42 (17%) |
| Pre-existing diabetes | 5 (2%) |
| Substance use | 159 (64%) |
| Obstetric history | |
| History of fetal growth restriction in previous pregnancy | 19 (7.7%) |
| History of hypertensive disorder of pregnancy | 16 (6.5%) |
| Ultrasound outcomes | |
| Gestational age at last ultrasound (weeks) | 36 (34,37) |
| 2D EFW of last ultrasound before delivery | 2444 (2185, 2663) |
| 3D EFW of last ultrasound before delivery | 2291 (1982, 2541) |
| Number of weeks from last ultrasound to delivery | 2 (1,3) |
| < 7 days | 32 (13%) |
| 7–13 days | 54 (22%) |
| 14–20 days | 52 (21%) |
| 21–27 days | 53 (21%) |
| 28–34 days | 57 (23%) |
| Obstetric outcomes | |
| Fetal growth restrictiona | 6 (2.4%) |
| Hypertensive disorder of pregnancy | 41 (17%) |
| Placental abruption | 5 (2.0%) |
| Intrauterine demise | 1 (0.4%) |
| Gestational age at delivery (weeks) | 38 (37, 39) |
| Preterm delivery | |
| < 37 weeks | 41 (17%) |
| < 34 weeks | 9 (3.6%) |
| Cesarean delivery | 53 (21%) |
| Neonatal outcomes | |
| Female sex | 132 (55%) |
| Neonatal birthweight (grams) | 2667 (2430, 2880) |
| Birthweight extremes | |
| < 2000 g | 14 (5.6%) |
| < 2500 g | 74 (29.8%) |
- a Fetal growth restriction (FGR) is defined as a 2D EFW and/or AC measuring <10% for gestational age.
Ultrasound studies included in this analysis were performed at a median gestational age of 36 weeks (IQR 34, 37 weeks). The median number of weeks from last ultrasound measurement to delivery was 2 weeks with 13% undergoing the last ultrasound measurements <1 week from delivery (Table 1). The median 2D EFW and 3D EFW of the last ultrasound prior to delivery were 2444 g (IQR 2185 g, 2663 g) and 2291 g (IQR 1982, 5541), respectively. Fetal growth restriction—defined as 2D EFW or AC < 10% for GA—was diagnosed prenatally in 2.4% of pregnancies analyzed (Table 1). The median BW was 2667 g (IQR 2430, 2880) with 5.6% neonates with BW < 2000 g and 29.8% neonates with BW < 2500 g.
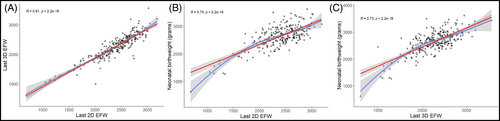
Normal distributions of 2D and 3D EFWs were confirmed. A high degree of correlation was seen between both 2D EFW and BW (R = 0.74, p < 0.05) and 3D EFW and BW (R = 0.73, p < 0.05, Figure 2). There was no difference in the degree of correlation between 2D EFW and BW and correlation between 3D EFW and BW.
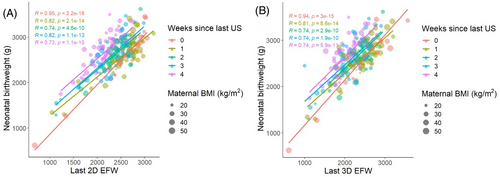
There was no relationship between maternal BMI and degree of correlation between 2D and 3D EFW and BW (Figure 3). However, the degree of correlation between 2D and 3D EFW with BW were significantly associated with number of weeks from last ultrasound to delivery (both p < 0.001, Figure 3). When adjusted for the number of weeks from last ultrasound to delivery, the degree of correlation between EFW and BW improved for both 2D (0.95, 95% CI 0.87, 1.00) and 3D EFW (0.85, 95% CI 0.77, 0.93). Individual comparisons indicated a stronger correlation between 2D EFW and BW and 3D EFW and BW among pregnancies with ultrasounds performed <7 days from delivery when compared to pregnancies with ultrasounds performed ≥7 days from delivery (all p < 0.05, Table 2). Considering only pregnancies with last ultrasound measurements performed <7 days from delivery, 2D EFW and 3D EFW correlated similarly with BW (p = 1.0).
| < 7 days | 7–13 days | 14–20 days | 21–27 days | 28–34 days | |
|---|---|---|---|---|---|
| < 7 days | < 0.05 | < 0.05 | < 0.05 | < 0.05 | |
| 7–13 days | < 0.05 | 0.30 | 1 | 0.24 | |
| 14–20 days | < 0.05 | 0.38 | 0.30 | 0.91 | |
| 21–27 days | < 0.05 | 0.38 | 1 | 0.25 | |
| 28–34 days | < 0.05 | 0.37 | 1 | 1 |
The mean percent differences (systematic error) for all pregnancies were 11.3% and 14.8% with standard deviation (random error) of 8.1% and 9.8% for 2D EFW and 3D EFW, respectively. When stratified by the interval between last ultrasound and delivery, the mean percent difference was larger (less accurate) for 3D EFW when compared to 2D EFW for all ultrasounds performed ≥7 days from delivery (all p < 0.05, Table 3). There was no difference in mean percent difference for 2D and 3D EFW when performed <7 days from delivery.
| 3D EFW | 2D EFW | p value | |
|---|---|---|---|
| 28–34 days from delivery | 14.8% ± 9.8% | 11.3% ± 8.1% | < 0.05 |
| 21–27 days from delivery | 12.3% ± 8.8% | 9.1% ± 6.6% | < 0.05 |
| 14–20 days from delivery | 10% ± 7.1% | 7.7% ± 5.6% | < 0.05 |
| 7–13 days from delivery | 8.1% ± 7.0% | 6.3% ± 5.3% | 0.03 |
| < 7 days from delivery | 6.7% ± 4.4% | 5.1% ± 4.0% | 0.13 |
- Note: The bolded items were to signify statistically significant findings, i.e., p < 0.05.
EFW prediction within 5% of BW occurred more frequently with 2D EFW compared to 3D EFW (28.6% vs. 19.4%, p = 0.02). When stratified by weeks from delivery, 2D EFW and 3D EFW similarly predicted BW within 5% when performed <21 days from delivery (Table 4). EFW prediction within 10% of BW also occurred more frequently with 2D EFW compared to 3D EFW (49.2% vs. 36.7%, p < 0.05). When stratified by weeks from delivery, 2D EFW and 3D EFW similarly predicted BW within 10% when performed <14 days from delivery (Table 4).
| Percent difference from BW ≤5% | Percent difference from BW ≤ 10% | |
|---|---|---|
| 28–34 days from delivery | ||
| Using 2D EFW | 71/248 (28.6%) | 122/248 (49.2%) |
| Using 3D EFW | 48/248 (19.4%) | 91/248 (36.7%) |
| p-Value | 0.02 | 0.004 |
| 21–27 days from delivery | ||
| Using 2D EFW | 66/191 (34.6%) | 113/191 (59.2%) |
| Using 3D EFW | 47/191 (24.6%) | 88/191 (46.1%) |
| p-Value | 0.03 | 0.01 |
| 14–20 days from delivery | ||
| Using 2D EFW | 55/140 (39.3%) | 93/140 (66.4%) |
| Using 3D EFW | 42/140 (30%) | 76/140 (54.3%) |
| p-Value | 0.10 | 0.04 |
| 7–13 days from delivery | ||
| Using 2D EFW | 45/88 (51.1%) | 68/88 (77.3%) |
| Using 3D EFW | 36/88 (40.9%) | 61/88 (69.3%) |
| p-Value | 0.17 | 0.23 |
| < 7 days from delivery | ||
| Using 2D EFW | 45/86 (52.3%) | 67/86 (77.9%) |
| Using 3D EFW | 36/86 (41.9%) | 60/86 (69.8%) |
| p-Value | 0.17 | 0.22 |
- Note: The bolded items were to signify statistically significant findings, i.e., p < 0.05.
4 DISCUSSION
To address degrees of error with standard 2D fetal weight estimates and to improve fetal weight estimation, the incorporation of fetal soft tissue measurements via 3D EFW has been proposed. Fetal weight estimates incorporating these soft tissue parameters may have a similar or improved correlation with neonatal birthweight and composition among fetuses with normal or accelerated growth patterns.9, 10, 15, 19-24 Our study aimed to evaluate if similar findings persist among pregnancies with borderline small fetuses and if 3D methods perform better than standard 2D methods in the prediction of BW.
Our study demonstrated that 3D EFW performed within 4 weeks of anticipated delivery demonstrated a strong correlation with BW (r = 0.73) among a cohort with borderline small fetuses. This was similar to the degree of correlation between 2D EFW performed within 4 weeks of delivery and BW (r = 0.74). An inverse relationship between the degree of correlation between EFW and BW and the number of weeks from last ultrasound to delivery was shown. The highest degree of correlation was demonstrated in pregnancies where the last ultrasound was performed <7 days from delivery.
Our study demonstrated that 2D fetal weight predictions were more accurate (smaller systematic error) and more precise (smaller random error) than 3D EFW when performed ≥7 days from delivery. When measurements were performed <7 days from delivery, systematic and random errors were similar for 2D EFW and 3D EFW. These findings are supported by BW prediction more often within 5% or 10% of BW for 2D EFW when compared to 3D EFW performed 3–4 weeks prior to birth and by similar prediction of BW within 5 and 10% by 2- and 3D EFW when performed within 1–2 weeks of birth. We hypothesize that (1) smaller proportions of fetal adipose tissue (soft tissue) in the studied cohort, (2) variability in the growth of fetal soft tissue in the third trimester, and/or (3) technical limitations of soft tissue measurement in a third trimester fetus may have contributed to the decreased performance of 3D EFW prediction of BW when performed ≥7 days from delivery.40, 41 The biometric parameters used in standard, 2D EFW prediction—BPD, HC, AC, and FL—demonstrate a relatively linear growth trajectory. This linearity may have reduced variability in weight prediction and, therefore, provided increased accuracy and precision of BW prediction. Both 2D and 3D EFW at <7 days from delivery perform similarly for BW prediction because we assume limited fetal growth over a one-week period. These findings suggest that fetal weight estimation using standard, 2D methods may be more reliable in the prediction of BW than 3D methods among borderline small fetuses.
The high-risk maternal population and the specific evaluation of borderline small fetuses serve as strengths of this study. Additionally, this study reports on 41 pregnancies (17%) with preterm delivery as early as 25 weeks' gestation. This differs from prior studies which have largely evaluated 3D EFW correlation with BW among pregnancies with term deliveries. Lastly, the incorporation of ultrasound measurements performed between 1 and 4 weeks from delivery contributes to clinical applicability, specifically in the outpatient setting. This study supports the reliability of both 2D and 3D methods of fetal weight estimation up to 4 weeks from delivery with preference for 2D methods ≥7 days from delivery. Therefore, measurements obtained through outpatient obstetric practice of serial fetal growth surveillance can reliably inform delivering providers. Limitations of this study include its retrospective nature and relatively low capture rate of 3D EFW (20.4%) among all pregnancies with borderline small fetuses indicating low compliance with the protocol. The low capture rate may introduce selection bias, preferentially including pregnancies at increased risk for growth restriction. This may be evidenced by the relatively high rate of substance use and chronic hypertension among this cohort, compared to nationally reported rates.42, 43
5 CONCLUSION
This study demonstrated that both 2D EFW and 3D EFW correlate well with BW when performed within 4 weeks of delivery. The degree of correlation for both 2D and 3D EFW and BW increased inversely with weeks from last ultrasound delivery with the strongest correlation seen when performed <7 days from delivery. Beginning 4 weeks prior to delivery, 2D estimates of fetal weight more accurately predict BW than 3D estimates. 3D estimation of EFW does not improve the accuracy of BW prediction.
ACKNOWLEDGMENTS
The authors thank the sonographers and maternal-fetal medicine physicians at The MetroHealth System's Fetal Diagnostic Center for acquisition and interpretation of the reviewed studies. We also thank the following members of The MetroHealth System/ Case Western Reserve Maternal-Fetal Medicine fellowship for their contributions to study concept and design: Drs. David Hackney, Emily Hamburg-Shields, Alexandra Berra, Danielle Olson.
FUNDING INFORMATION
This study did not utilize external funding.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest or financial interests to disclose.
ETHICAL APPROVAL
Study approval was obtained from the MetroHealth Institutional Review Board (#IRB21-00671).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.