Difference between remimazolam toluenesulfonic acid and propofol in waking quality and conscious state after general anesthesia
Abstract
Objective
To explore the difference of anesthesia recovery and postoperative conscious state between remimazolam toluenesulfonic acid and propofol after induction and maintenance of general anesthesia.
Methods
104 patients undergoing elective tracheal intubation general anesthesia in our hospital were randomly divided into 2 groups: Remimazolam Toluenesulfonic acid group (Group R) and Propofol group (Group P). MOAA/S score, the modified Aldrete score, recovery index, time point, a state of consciousness, interpretative vital signs and adverse events were monitored at different time.
Results
Compared with the Group P, the extubation time and orientation recovery time of the Group R were significantly shorter. When the operation time was less than 1 hour, the MOAA/S score of the Group R was shorter than that of Group P at 5 min and 15 min after the operation. To compare with the Group P, the score of MOAA/S in the Group R increased at 5 min, 20 min and 30 min after the operation. When the operation time was less than or equal to 1 h, the modified Aldrete score in the Group R was slightly higher than that in the Group P at 30 min after extubation. There was no injection pain in the the Group R, and the incidence of hypotension was lower than that of propofol.
Conclusion
Compared with Propofol, when the operation time of general anesthesia is more than 1 hour, recovery time of Remimazolam Toluenesulfonic acid is shorter, with more complete and higher-quality recovery.
Introduction
General anesthesia sedatives have a reversible inhibitory effect on the central nervous system (Sneyd, et al., 2020). After injection of sedatives, the consciousness and various reflexes of the patients gradually disappear (Wesolowski, et al., 2016). However, due to the pharmacological property of different sedatives, different patients take amount of time to fully wake up and recover to preoperative state of consciousness. As for short-term general anesthesia ambulatory surgery, the quality of postoperative recovery and the time to regain psychomotor are not only closely linked to whether the patients can be discharged quickly, but also play an important role in accelerating the recovery after long-term general anesthesia surgery. Remimazolam Toluenesulfonic acid is a new esterified type of Benzodiazepine (BZ) sedative. After being metabolized by Plasma Esterase, the context-sensitive half-time (GSHT) is not subject by time-course (Goudra, et al., 2014; Pastis, et al., 2019; Keam, 2020). It can be antagonized by flumazenil with rapid-action profile and quick elimination (Chen, et al., 2020). It is a fresh choice for sedation or general anesthesia. It has been widely used in painless gastroscopy, fiberoptic bronchoscopy and general anesthesia, obtaining extreme focus and studies from scholars at home and abroad (Rex, et al., 2018; Freyer, et al., 2019; Doi, et al., 2020; Schüttler, et al., 2020; Wang, et al., 2020). According to this sedative, there are a lot of papers discussing from basic research to clinical practice, from health cases to clinics, but these papers rarely reports about the quality of postoperative recovery and recovery of normal sense. Propofol is one of the most commonly used anesthetic and sedatives at home and abroad (Wesolowski, et al., 2016; Schraag, et al., 2018). Owing to the difference of their pharmacological property, these two kinds of drugs leave distinctive marks on the CNS. In this paper, through studying the above two kinds of sedatives’ horizontal differentiation in sobering quality and emergence of conscious state when they are applied to short-term and long-term surgeries, we aim at exploring a better anesthesia medication scheme, speeding up the postoperative recovery of patients with general anesthesia to reduce hospitalization time and save medical resources (Figure 1).
Research flow chart
Materials and methods
General information
This study was approved by the hospital ethics committee. After informed consent of patients and their families, a total of 104 patients under general anesthesia undergoing elective endotracheal intubation in our hospital from August 2020 to October 2020 were collected as research subjects.
Inclusion criteria: tracheal intubation under general anesthesia, 18y ≤ age ≤ 60y, regardless of gender; American Society of Anesthesiologists (ASA) grade I-II; the altitude of permanent residence is lower than 2500 meters; willing to sign informed consent and strictly abide by the clinical research protocol to complete this study.
Exclusion criteria
Patients who are under the following conditions are excluded from the study: allergic to related narcotic drugs; suffering from cardiovascular, respiratory, central nervous system, liver and kidney disease; taking other experimental drugs or participating in other clinical trials within 3 months before inclusion; unwilling to continue the experiment.
Eligible patients were randomly divided into two groups: Group R (Remimazolam) and Group P (Propofol).
Anesthesia management program
Anesthesia induction: Group R takes Sufentanil 0.4 μg/kg, Remimazolam Toluenesulfonic acid 0.2 mg/kg and Rocuronium 0.8 mg/kg. Group P takes Sufentanil 0.4 μg/kg, Propofol 2.5 mg/kg and Rocuronium 0. 8 mg/kg.
Anesthesia maintenance: Group R takes Remimazolam Toluenesulfonic acid 0.2-0.6 mg/kg/h, Remifentanil 7-10 μg/kg/h, Cisatracurium 0.1 mg/kg/h; Group P takes Propofol 4-10 mg/kg/h, Remifentanil 7-10 μg/kg/h, and Cisatracurium 0.1mg/kg/h.
The two groups were hooked up to IV drips with Sufentanil 0.2 μg/kg and Parecoxib sodium 40 mg for 30 min before the end of operation. Before suturing the incision, deliver local anesthesia with 0.3% Ropivacaine 10-20 mL. The use of Cisatracurium was stopped 40 min before the end of operation. As soon as the operation completes, stop the use of Remimazolam, Propofoland and Remifentanil right away.
Monitoring indicators
Main outcome measurements: MOAA/S score (Schüttler, et al., 2020), modified Aldrete score (Rex, et al., 2018), time point of recovery index (Table 1).
| Items | Rating(‘) |
|---|---|
| Complete recovery, normal response to normal calls | 5 |
| Slow response to normal calls | 4 |
| Only response to loud and/or repeated name calls | 3 |
| Only respond to slight push or slight shaking | 2 |
| Only response to pain stimulation (pressing trapezius) | 1 |
| No response to painful stimulation (squeezing trapezius) | 0 |
Secondary outcome measures: interpretative vital signs, incidence of adverse events (hypotension, nausea and vomiting, irritability, etc).
Monitoring time: MOAA/S score: immediately after the end of the operation, score was made at 0 min, 5 min, 10 min, 15 min, 20 min, 30 min, 60 min and 90 min.
Modified Aldrete score: at 0, 15, 30, 45, 60 and 90 min after extubation of tracheal tube (Table 2).
| Assessment items | Rating(‘) | |
|---|---|---|
| Activity | ||
| Can freely Move limbs or follow instructions | 2 | |
| Both limbs can move | 1 | |
| All four limbs can not move | 0 | |
| Respire | ||
| Can do deep breathing and effective cough | 2 | |
| Dyspnea, superficial or restricted | 1 | |
| Asphyxia | 0 | |
| Circulation | ||
| Basal blood pressure ± Within 20 mmHg | 2 | |
| Basal blood pressure ± Within 20-50 mmHg | 1 | |
| The fluctuation of blood pressure was more than 50 mmHg | 0 | |
| Consciousness | ||
| Complete recovery | 2 | |
| Can wake up | 1 | |
| No response | 0 | |
| Oxygen saturation | ||
| Breathing air SpO2 > 92% | 2 | |
| Can maintained SpO2 > 92% during oxygen inhalation | 1 | |
| SpO2 < 92% during oxygen inhalation | 0 | |
Statistical analysis
Spss21.0 software was used only for statistical analysis. Measurement data of normal distribution are expressed as mean standard deviation. ANOVA was an approach for comparison between groups. ANOVA of repeated measurement design was used for intra group comparison, and Fisher exact probability method was utilized for uneven variance.
The enumeration data were expressed as rate and constituent ratio. We use Chi square test to draw a comparison between groups, and nonparametric rank sum test was applied to skewing distribution data. If p < 0.05, the difference was statistically significant.
Results
Statistical data of two groups
104 patients undergoing elective tracheal intubation general anesthesia in our hospital were randomly divided into two groups: Remimazolam Toluenesulfonic acid group (Group R, n = 52) and Propofol group (Group P, n = 52). There was no significant difference in age, gender, height, weight, ASA grade and operation time between the two groups, indicating that the baseline of the two groups was neat (Table 3).
| Grouping | Group R (n = 52) | Group P (n = 52) | P-value | |
|---|---|---|---|---|
| Age (years) | 48.6±13.8 | 46.8±11.3 | 0.489 | |
| Gender | Male | 24 (0.46%) | 25 (0.48%) | 0.941 |
| Female | 28 (0.54%) | 27 (0.52%) | ||
| Height (cm) | 161.0±8.6 | 159.5±7.4 | 0.572 | |
| Weight (kg) | 60.2±10.5 | 60.5±9.0 | 0.883 | |
ASA Classification |
Ⅰ | 22 (0.42%) | 24 (0.46%) | 0.576 |
| Ⅱ | 30 (0.58%) | 28 (0.54%) | ||
| Operation time | ≤1 h | 26 cases (50%) | 26 cases (50%) | |
| >1 h | 26 cases (50%) | 26 cases (50%) | ||
Statistics of recovery time points
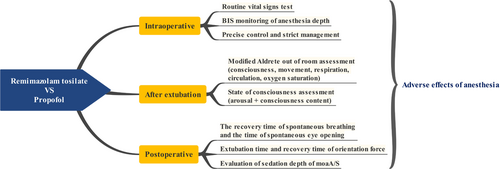
Compared with the Group P, difference in spontaneous breathing time, eye opening time and follow-up time was not statistically significant, but the time of extubation and orientation recovery was distinctly shorter (Figure 2). However, the extubation time in both groups was within 40 min after surgery. There was no adverse event of delayed awakening. The recovery time of directional force was also within 40 min after surgery, suggesting that the two kinds of anesthetic sedative drugs are safe and effective in clinical application.
Recovery time points statistics of two groups. (A) Spontaneous respiratory time. (B) Eye opening time of call. (C) Obedience time. (D) Extubation time. (E) Directional force recovery time.
MOAA/S score
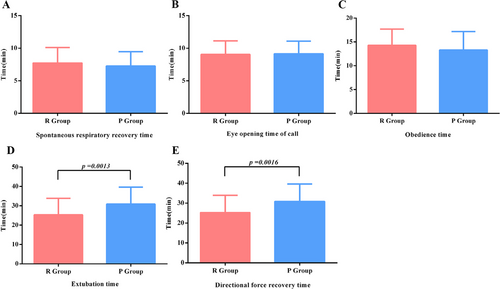
There was no significant differences in MOAA/S score between the two groups at different time points after surgery. About 20 min after the operation, the MOAA/S score of the patients was ≥ 4, suggesting that the two groups of patients woke up within 20 min as shown in Figure 3. However, when the operation time was stratified as ≤ 1 h and > 1 h, the statistical results of the two groups were different. When the operation time was less than 1 hour, the MOAA/S score of the Group R was lower than that of Group P at 5 min and 15 min after the operation. Compared with the Group P, the scores of MOAA/S in the Group R increased at 5 min, 20 min and 30 min if the operation time exceeding 1 h as shown in Figure 3 and Figure 3. For prolonged surgery, the Group R woke up faster (Figure 3, Table 4).
| Time point | 0 min | 5 min | 10 min | 15 min | 20 min | 30 min | 60 min | 90 min |
|---|---|---|---|---|---|---|---|---|
Operation time ≤ 1 h |
||||||||
| R Group (n = 26) | 0.0±0.00 | 0.6±0.86** | 2.3±0.84 | 3.6±0.70** | 4.9±0.33 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| P Group (n = 26) | 0.0±0.00 | 1.3±0.84 | 2.2±0.43 | 4.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| Operation time >1 h | ||||||||
| R Group (n = 26) | 0.0±0.00 | 0.4±0.50** | 1.2±0.75 | 2.4±0.50 | 4.4±0.50** | 5.0±0.00** | 5.0±0.00 | 5.0±0.00 |
| P Group (n = 26) | 0.0±0.00 | 0.0±0.00 | 0.8±1.01 | 1.9±0.99 | 3.7±0.85 | 4.4±0.50 | 5.0±0.00 | 5.0±0.00 |
| sum | ||||||||
| R Group (n = 52) | 0.0±0.00 | 0.5±0.10 | 1.8±0.13 | 3.0±0.12 | 4.6±0.07 | 5.0±0.00 | 5.0±0.00 | 5.0±0.00 |
| P Group (n = 52) | 0.0±0.00 | 0.7±0.12 | 1.5±0.14 | 2.9±0.18 | 4.3±0.13 | 4.7±0.06 | 5.0±0.00 | 5.0±0.00 |
- ** Comparison between P group and R group p < 0.01.
MOAA/S score of two groups at different operation time. (A) Total MOAA/S scores of patients in the two groups at different time points; (B) MOAA/S score at different time points: patients with surgery time ≤1 h; (C) MOAA/S score at different time points: patients with surgery time > 1 h. **Comparison between P group and R group p < 0.01.
Modified Aldrete score
In general, the total Aldrete score of the two groups at 30 min after extubation was higher in the R group than in the P group, and the difference was statistically significant, as shown in Figure 4. However, the Aldrete score was different at different time points after extubation for short-term and long-term operations. In Figure 4, we found that the difference of Aldrete total score between the two groups of patients with operation time less than or equal to 1 h was consistent with the overall data. However, as shown in Figure 4, at 15 min and 30 min after extubation the total Aldrete score of the R group was higher than that of the P group with operation time of more than 1 h, and the differences between the groups were statistically significant. So we can firmly believe that for long-term operation, recovery quality of Group R is better. Scores of 60 min and 90 min after extubation in the two groups declined, which suggests that the patients may fall asleep again and fuzzy consciousness after awakening, so it requires intensive supervision.
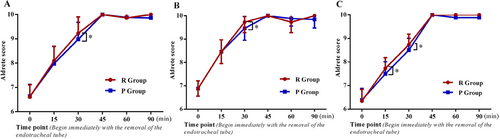
Modified Aldrete score after extubation in two groups with different operation time. (A) Total Modified Aldrete score of patients in the two groups at different time points. (B) Modified Aldrete score at different time points: patients with surgery time ≤ 1 h. (C) Modified Aldrete score at different time points. patients with surgery time > 1 h. *Comparison between P group and R group p < 0.05.
Based on the difference of the overall score, we split the 5 parts of the Aldrete score, and conducted statistical analysis on the levels of less than or equal to 1 h and more than 1h respectively according to the length of the operation. It was found that in the 5 parts, for patients with operation time longer than 1h, at 1 h 15 min and 1 h 30 min after extubation, there were significantly more patients in the Group R who were fully conscious than those in the Group P. The difference was statistically significant (p < 0.05) as shown in Figure 5. There was no significant difference in oxygenation, respiration, circulation and movement at each time point (Figure 5). Some of the patients in the two groups fell asleep again and oxygen saturation decreased 45 min and 60 min after extubation, but the difference between the groups was not statistically significant. It was suggested that the recovery of consciousness in the Gropu R was better than that in the Group P, especially when the operation time lasted for more than 1 h.
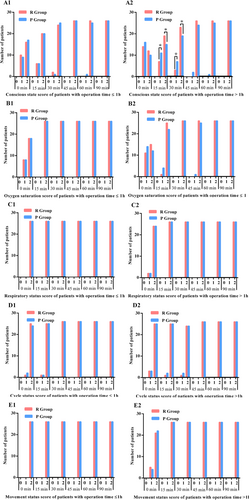
Statistical analysis of five parts of modified Aldrete score after extubation in patients with different operative time in the two groups. (A1) Conscious state score of patients with operation time ≤1 h. (A2) Conscious state score of patients with operation time > 1 h. (B1) Oxygen saturation score of patients with operation time ≤ 1 h; (B2) Oxygen saturation score of patients with operation time > 1 h. (C1) Respiratory status score of patients with operation time ≤1 h; Respiratory status score of patients with operation time > 1 h; (D1) Cycle status score of patients with operation time ≤ 1 h; (D2) Cycle status score of patients with operation time > 1 h; (E1) Movement status score of patients with operation time ≤ 1 h. (E2) Movement status score of patients with operation time > 1 h. *Comparison between Group P and Group R p < 0.05.
Conscious state statistics
For the consciousness state of patients after extubation, we made more detailed observation and statistics in Table 5. It was found that 30min and 45min after extubation, due to drug metabolism insufficiency and lack of external stimulation, patients in both groups fell asleep again. However, compared with the propofol group, fewer patients fell asleep again in the remazolam group, and the difference between the groups was statistically significant.
| Time point After extubation | Grouping (n = 52) | Wakefulness | Conscious content | ||||
|---|---|---|---|---|---|---|---|
| Conscious | Drowsiness | Lethargy | Coma | Confusion | Delirious state | ||
| 0 min | Group R | 28 | 24 | 0 | 0 | 41 | 0 |
| Group P | 30 | 22 | 0 | 0 | 39 | 2 | |
| 15 min | Group R | 31 | 21 | 5 | 0 | 38 | 0 |
| Group P | 25 | 27 | 9 | 0 | 35 | 2 | |
| 30 min | Group R | 43* | 9* | 0 | 0 | 30 | 0 |
| Group P | 33 | 19 | 2 | 0 | 32 | 0 | |
| 45 min | Group R | 48* | 4* | 0 | 0 | 21 | 0 |
| Group P | 39 | 13 | 0 | 0 | 28 | 0 | |
| 60 min | Group R | 51 | 1 | 0 | 0 | 18 | 0 |
| Group P | 45 | 7 | 0 | 0 | 22 | 0 | |
| 90 min | Group R | 52 | 0 | 0 | 0 | 15 | 0 |
| Group P | 49 | 3 | 0 | 0 | 20 | 0 | |
- * Comparison between P group and R group p < 0.05.
Statistics of adverse events
There was no significant differences in the incidence of postoperative nausea and vomiting between the two groups. Compared with Group P, the Group R has no injection pain. The incidence of preoperative hypotension in the Group R (9.62%) was significantly lower than that in the Group P (23.08%) (p = 0.0021). It is suggested that the use of remazolam is relatively safe and comfortable (Figure 6, Table 6).
| Complication | Group R (n = 52) | Group P (n=52) | p |
|---|---|---|---|
| Injection pain | 0.00% (0 case) | 21.20% (11 cases) | 0.0001 |
| Hypotension | 9.62% (5 cases) | 23.08% (12 cases) | 0.0021 |
| Postoperative irritability | 0.00% (0 case) | 3.85% (2 cases) | 0.082 |
| Postoperative nausea and vomiting | 5.77% (3 cases) | 7.69% (4 cases) | 0.128 |
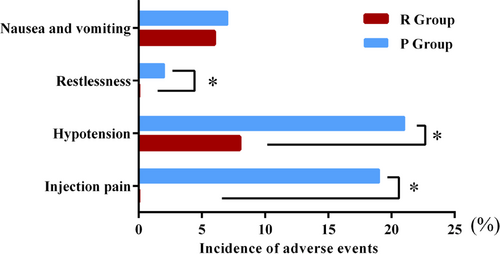
Statistics of anesthesia related complications in two groups. *Comparison between Group P and Group R p < 0.05.
Discussion
With the development and application of bio psycho social medical model, the National Health Commission issued the pilot work plan of accelerated rehabilitation surgery (2019-2020) in November 2019, which puts forward new requirements for the whole surgical system (Sear, 2018). It is hoped to take a series of optimization measures to achieve the purpose of speedy rehabilitation of patients (Gin, 2013; Khurmi, et al., 2017; Tanious, et al., 2017). The implementation of ERAS is closely related to anesthesia management, especially when it comes to accurate anesthesia management and drug selection, which can improve the quality of anesthesia recovery, improve the postoperative consciousness of patients, reduce the incidence of anesthesia related complications, in the pursuit of rapid recovery (Rogers and McDowell, 2010; Hansen, 2015). The advent of a new anesthetic and sedative drug, Remimazolam Toluenesulfonic acid, provides a new option for accelerated rehabilitation management of anesthesia (Chen, et al., 2020; Doi, et al., 2020; Rex, et al., 2021). Its emergence has aroused the close attention from scholars at home and abroad. Many articles with great factors have been published all over the world (Antonik, et al., 2012; Borkett, et al., 2015; Pambianco, et al., 2016; Bevans, et al., 2017; Hirata, et al., 2020; Pesic, et al., 2020). Yet there are limited reports about the quality of recovery and the recovery of consciousness. In this paper, through the induction and maintenance of general anesthesia, respectively, the application of Remimazolam Toluenesulfonic acid or propofol, to explore which anesthesia related complications rate is smaller, which performs better in waking up and more in line with the concept of accelerated rehabilitation management.
The study found that there was no significant difference in spontaneous breathing time, eye opening time and command time between the two groups, but the extubation time and orientation recovery time was significantly shorter. Meanwhile, the scores of MOAA/S were lower in 5 min and 15 min after operation when the operation time was less than 1 h; the scores of MOAA/S at 5 min, 20 min and 30 min after the operation and the scores of modified Aldrete at 15 min and 30 min after extubation increased. These statistics demonstrate that there is no significant difference in the recovery time and quality between the two sedatives in short-term operation. However, for long-term operation, the recovery time and quality of Remimazolam Toluenesulfonic acid were faster and higher, which is more favorable (Worthington, et al., 2013; Sato, et al., 2020; Saito, et al., 2021). After extubation, the scores of both groups decreased at 60 min and 90 min, indicating that the patients had a vague consciousness when falling asleep again after awakening, which required intensive monitoring.
Separate statistics of the five parts of the modified Aldrete score showed that there were differences in the changes of consciousness, movement, circulation and oxygen saturation 15 min immediately after extubation between the two groups. The patients in the two groups fell asleep again and oxygen saturation decreased 45 min and 60 min after extubation (Yamamoto, et al., 2021). For 30 min and 45 min after extubation, compared with the Group R, more patients in Group P were in the state of drowsiness, and more patients fell into the confusion of consciousness. Compared with propofol, Remimazolam Toluenesulfonic acid not only had no injection pain, but also a lower incidence of hypotension, suggesting that it was relatively safer and more comfortable (Jia, et al., 2021; Tachibana, et al., 2021).
Remimazolam Toluenesulfonic acid is a kind of benzodiazepine sedative hypnotic drug, which produces a sedative effect by regulating GABAA receptor (Saari, et al., 2011; Yamamoto, et al., 2021). Through the metabolism of plasma esterase, there is no burden on liver or kidney (Lamperti, 2015; Kochhar, et al., 2016). After continuous transfusion, the time-dependent half-life was not affected by the infusion time, lasting about 5-7 min. It can be antagonized by flumazenil with strong specificity and controllability, and owns the advantages of quick onset, quick elimination at the same time (Chen, et al., 2021). Moreover, It has short sedation recovery time, almost no injection pain, and low incidence of hypotension and respiratory depression, which is a better alternative for sedation under general anesthesia (Yoshida, et al., 2021).
Conclusion
Compared with propofol, when the operation time of general anesthesia is more than 1 hour, recovery time of remimazolam toluenesulfonic acid is shorter, with more complete and higher-quality recovery. If we use remimazolam toluenesulfonic acid, patients’ state of consciousness is better, benefiting to accelerate the recovery of patients. But it need to be noted that there was drowsiness and fuzzy consciousness in both groups 60 min after operation, so postoperative monitoring and individualized management should be strengthened. In the preoperative period, its incidence of hypotension was lower than that of propofol. There was no injection pain. However, this study also has several shortcomings, such as small sample size. The conclusion of this study has yet to be demonstrated by expanding the sample size for multi-center clinical study.
Ethical statement
This study was approved by the ethics committee in the Affiliated Hospital of Zunyi Medical University.
Consent to participate
Written consent was signed for all the patients of aged 18 y or above. For patients under 18, a legal guardian or parent signed the consent form..
Acknowledgements
Not applicable.
Conflict of interest
The authors declared that they have no conflicts of interest to this work.
Funding
This study was supported by the Beijing Medical Award Fund.
Transparency statement
All the authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Authors' contribution
Juan Li and Liu-Lin Xiong contributed the central idea, analysed most of the data, made figures & tables and wrote the initial draft of the paper. Di Zhou, Yang Jin, Hong-Su Zhou, Chang-Le Fang and Zhao-Qiong Zhu contributed to refining the ideas, carrying out additional analyses and finalizing this paper.