Inadvertent mental excitement after ultrasound-guided bilateral thoracic paravertebral block: a case report
Abstract
Background
Bilateral Paravertebral block has been used successfully for postoperative pain relief in thoracic, abdominal, and pelvic regions. Despite the need for relatively large doses of local anaesthetics, there are few reports of systemic toxicity. Here we reported a case of local anaesthetic toxicity after ultrasound-guided bilateral thoracic paravertebral block before general anaesthesia leading to mental. To our knowledge, the onset of this patient has never been reported previously, and we will discuss the potential risk factors and preventive measures for such patients in the future.
Case information
A 38-year-old female patient presented for elective open resection of liver tumor, when bilateral 7th thoracic (T7) paravertebral blocks were performed under the guidance of ultrasound with 0.5% ropivacaine (3 mg/kg) in the anesthesia preparation area. After 20 minutes, the patient suddenly became extremely excited and requested to suspend the operation, because Guanyin Bodhisattva just told her that the operation would put her life in danger.
Conclusion
Although the dose of ropivacaine was up to 3 mg/kg for lumbar epidural, or 4.3 mg/kg for major nerve block based on the manufacturer’s recommendation, we believe that the bolus dosage of 0.5% ropivacaine 3 mg/kg was high for bilateral thoracic paravertebral block in this patient.
Background
With the development of ultrasound technology and the proposal of multimodal analgesia, peripheral nerve blocks are widely used in perioperative analgesia. Paravertebral block (PVB) is a technique of injecting local anesthetics into the paravertebral space produces an ipsilateral somatic and sympathetic nerve block, which can effectively control the pain of thoracic and abdominal surgery. A previous case reported serious systemic toxicity in continuous PVB with bupivacaine after thoracotomy and lobectomy leading to seizure, aspiration, ultimately death (Fagenholz PJ, et al., 2012). However, the complication rate of single-injection bilateral thoracic paravertebral block (TPVB) with ropivacaine under ultrasound-guided is very low (Richardson J, et al., 2011; Niesen AD, et al., 2020). This is the first case of neurological complication that is dominated by excitement and eventually leads to cancellation of the operation after preoperative TPVB with ultrasound-guided.
Case presentation
A 38-year-old female (height: 160 cm, weight: 57.5 kg) was scheduled to undergo open local resection of recurrent hepatocellular carcinoma in our hospital. The patient was found to have liver tumor during a physical examination 5 months ago and subsequently underwent an open liver tumor resection in another hospital, which was successful. The patient's biochemical examination showed that the albumin decreased to 38.5 g/L, and no significant change in other tests from the previous findings. Before general anaesthesia, bilateral TPVB was successfully performed by a skilled anesthesiologist at T7-8 level in an anaesthetic procedure room with standard monitoring. The patient was placed in the left lateral decubitus position. A 2-5 MHz curved array transducer (M-Turbo, Sonosite, Bothell, USA) was used to identify paravertebral space at T7 level. An in-plane needle guidance technique with a 10 cm, 22 G insulated needle (PAJUNK GmbH Medizintechnologie, Geisingen, Germany) was used to perform the right lateral TPVB under aseptic conditions (Figure 1, 2). Then, 17 ml of 0.5% ropivacaine was injected after confirming a negative aspiration for blood. Anterior movement of the pleura indicated the appropriate spread of the local anaesthetics in the paravertebral space (Figure 3). An out-plane needle guidance technique was performed on the contralateral side using the same drug. The vital signs were closely monitored since the patient arrived in the anesthesia preparation room. After 20 minutes, the patient suddenly became extremely excited and repeatedly stressed that Guanyin Bodhisattva just told her that the operation would put her life in danger. She strongly requested the operation to be suspended with intermittent crying. Based on her wordy and unrealistic content, anxiety, and dramatic irritability, we immediately diagnosed her as local anesthetic intoxication, which is a mind of moderate excitement and confusion (the different types of manifestations and diagnoses caused by local anesthetic intoxication were shown in the and Figure 4). We attempted to comfort the patient but did not relieve the patient’s emotion. After talking with the patient’s sister, we learned that the patient had been a devout Buddhist since she was diagnosed with liver cancer. When she was informed that the carcinoma had recurred, she became very anxious and hesitated to get a second operation. After 4 hours of close monitoring in the anesthesia preparation room, the patient's vital signs and cognitive function were stable. Finally, the operation was cancelled according to the wishes of the patient.
| Excitement | Inhibition | |||||
|---|---|---|---|---|---|---|
| Mild | Moderate | Severe | Mild | Moderate | Severe | |
| Circulatorysystem | + | + + | + + + | - | - - | - - - |
| Nervous system | +/- | + + | + + + | -~- - - | ||
| Respiratorysystem | - | + | + + | - | - - ~- - - | |
| Muscular tone | / | / | + | / | / | / |
- Notice: The number of ‘+’ or ‘-’ indicates the extend of the severity.

The behavior of thoracic paraspinal space block.
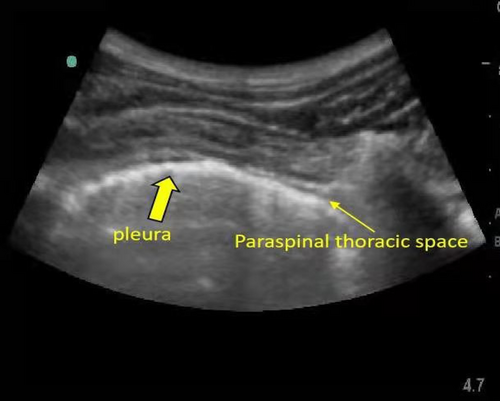
Corresponding ultrasonic image.
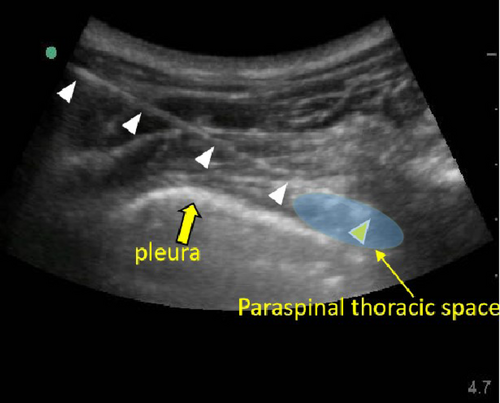
The image shows the path of neengle (white triangle), the tip (yellow), and the space of local anesthetic (blue).
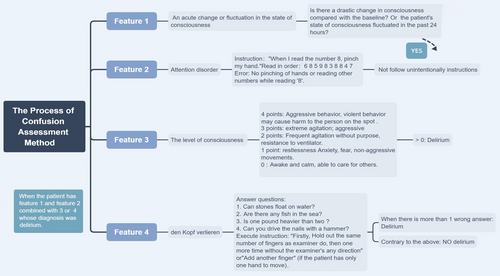
The process of confusion or delirium assessment method.
One month later, the patient was admitted to the hospital again for operation. The operation was successfully completed without paravertebral nerve block. At the end of the operation, 20 ml of 0.5% ropivacaine was used for local infiltration of the incision for postoperative analgesia. The patient recovered well without complication after surgery.
Discussion
Reportedly, the incidence of local anesthetic systemic toxicity (LAST) in peripheral nerve blocks is about 0.03% (Gitman M, et al., 2018). TPVB is the injection of local anesthetics into the thoracic paravertebral space. Compared with spinal anesthesia, it is considered to be the same effective and relatively safe. Therefore, it is widely used in intraoperative and postoperative analgesia of thoracic and abdominal surgery. 0.5% ropivacaine 3 mg/kg is the conventional concentration and dosage. There was no LAST in hundreds of patients who accepted bilateral TPVB with the same concentration and dosage previously in our institution. Although the dosage for regional nerve blocks are large variation within and among hospitals (Taenzer AH, et al., 2019). The concentration and dosage we used were the same or even smaller than those used in some hospitals and researches. A small observational study reported the plasma concentrations of ropivacaine peaked at almost above 2.2 μg/ml between 5-15 minutes after the bilateral bolus injection with 3 mg/kg. But only one patient suffered serious seizure within one minute of preoperative PVB (Ho AM, et al., 2016). There were studies using plasma concentration of 3 μg/ml or 4 μg/ml as the threshold toxicity (Bakker SMK, et al., 2018; Koniuch KL, et al., 2019). Due to the limitation of clinical researches, these threshold toxicities were calculated by animal models or published case reports. Unfortunately, the plasma concentrations were not measured in our patient. In future work or research, it is worth to measure the plasma concentration of local anesthetics to provide more evidence for the threshold toxicity and minimum effective dose of local anesthetics. Secondly, ropivacaine is an amide local anesthetic, mainly eliminated by liver metabolism. patients with liver cancer lead to a decrease in liver function and plasma albumin, which may lead to increase of the unbound ropivacaine that was responsible for the systemic toxicity (Jokinen MJ, et al., 2007).
Central nervous system (CNS) symptoms often precede the cardiovascular system when the patient has local anesthetic intoxication. This is because the CNS is more sensitive to local anesthetics. And seizure is the most common symptom of the CNS. However, excitement was the only manifestation in our case. This atypical presenting signs of LAST should arouse the attention of anesthesiologists. Another special feature was that our patient experienced excitatory symptoms 20 minutes after TPVB instead of immediately. This suggested the ropivacaine was not injected directly into the blood, but slowly absorbed into the blood attributed to the puncture of the blood vessel during the puncture process, and eventually the plasma concentration reached the threshold toxicity 20 minutes after the injection of ropivacaine. Interestingly, the patient did not have symptoms of LAST in the first bilateral TPVB with the same concentration and dose of ropivacaine. The concentration of ropivacaine may below the threshold toxicity without vascular damage. Additionally, another possible explanation for this phenomena is that the symptom of toxicity have been masked or affected by the general anesthesia (Murouchi T, et al., 2015).
This case alerts anesthesiologist that a single-injection of 3 mg/kg ropivacaine for ultrasound-guided bilateral TPVB may cause systemic toxicity in patients with liver disease. For patients with preoperative mental symptoms such as anxiety and depression, it may cause the patient become excited and unable to accept the operation. A randomized control study confirmed the addition of 5 μg/ml epinephrine to a single bolus injection of ropivacaine for TPVB could delay its systemic absorption and reduce peak plasma concentration (Manoj K, et al., 2005). And some studies have proved that the addition of dexmedetomidine or dexamethasone can reduce the amount of ropivacaine while providing high-quality analgesia (Zhang P, et al., 2019).
Conclusions
In spite of boluses that were within the manufacturer’s recommendation for epidural and major nerve blocks, a single-injection of 3 mg/kg ropivacaine via bilateral TPVB for patients with liver disease may cause local anaesthetic toxicity. Therefore, strict monitoring and awareness to identify LAST is very important during TPVB. Furthermore, the addition of epinephrine or other adjuvant to reduce the absorption of ropivacaine may be a better choice, and more importantly, the ultimate and optimal dose of single bilateral PVB before operation remain to be studied.
Ethical statement
This project was approved by the Ethic Commitees of West China Hospital Sichuan University (No. 2018-276).
Consent to participate
The patient has signed the informed consent.
Acknowledgements
Not applicable.
Conflict of interest
There is no conflict of interest in this study.
Funding
None.
Transparency statement
All the authors affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Authors' contribution
Mao Ye and Fei Liu conceived and designed the work that led to the submission. Hong-Su Zhou and Yi Wei revised the manuscript and approved the final version.