Targeted liver ultrasound for chronic liver disease: time to focus?
Abstract
Increasing prevalence of chronic liver disease has led to dramatically increased demands on ultrasound for diagnosis, monitoring and surveillance of complications. Targeted ultrasound of the liver provides an efficient and possibly more accurate means of meeting this demand. It uses a matrix to guide the ultrasound examination to address the specific clinical questions commonly asked in this population. It is easy to implement and can be modified to meet local preferences and emerging technologies.
Introduction
The prevalence of diffuse chronic liver disease has been increasing in Western communities such as ours over the past few decades1 with the majority of disease caused by alcohol, non-alcoholic fatty liver disease, chronic hepatitis C and B. This is accompanied by a substantial increase in demands on diagnostic ultrasound services for the purposes of diagnosis, monitoring, and identification of complications.
Many patients referred for ultrasound are being managed by physicians and specialists with training and experience in liver disease and their referrals tend to be quite specific. Questions commonly asked of the ultrasound examination are: is there evidence of fatty liver disease, fibrosis, cirrhosis, HCC or portal hypertension?
With the exception of fibrosis, which requires an ultrasound elastography means of assessing liver stiffness, these questions are addressed using well-validated gray scale and Doppler techniques targeted to the liver and related vasculature.
Despite the relatively specific nature of the questions there is a widespread sonographic culture, at least in Australia, for these requests to lead to a comprehensive examination of the upper abdomen. This is both time consuming and has the potential to divert the focus of the examination and therefore the diagnostic yield away from the clinical issues.
There is merit, therefore, in terms of diagnostic yield and resource utilisation in attempting to match the focus of the examination to the clinical question. One approach to achieving this focus efficiently is to make use of a matrix based on the clinical questions that need to be answered. This matrix guides the examination to be limited to diagnostically relevant simple and robust ultrasound signs. This approach, which we have termed “targeted ultrasound of the liver” (TUSL), is described below, and has parallels in many other areas of ultrasound where examinations are focused on specific questions, and organs that are in the region of the study are not examined (for example, FAST ultrasound in trauma, and some musculoskeletal studies).
Targeted ultrasound of the liver scanning matrix
-
Look at both the examination requested and the clinical notes to determine the precise nature of the request
-
For the indications listed in the left column there is no routine need to include other abdominal organs (e.g. kidneys, pancreas) unless there is a specific indication or finding during the study.
-
“Survey Liver” means a careful study of the liver. Do not study gall bladder, bile ducts, kidneys, pancreas, spleen or portal vein Doppler unless there is a specific indication or relevant finding.
-
If in doubt ask the radiologist before starting
-
These guidelines should not replace clinical judgement.
| Column 1 | Column 2 | Column 3 | Column 4 | Column 5 |
|---|---|---|---|---|
| Request | Survey liver for focal lesions | Cirrhosis images: – hi res surface – hi res left lobe – hep vein (5/6) | Lig teres (PUV) | Portal & hep veins, PUV and spleen for portal HT |
| Surveillance/screen for HCC ?focal liver lesion | + ONLY do this | |||
| Known cirrhosis ?HCC | + ONLY do this | |||
| ?cirrhosis ?HCC | + | + | + | |
| ?fibrosis ?cirrhosis | + | + | + | |
| HBV/HCV initial study | + | + | + | |
| ?FLD/fatty liver disease/NAFLD/ NASH | + | + | + | |
| ?Portal HT | + | + | + | + |
- Matrix used to guide the ultrasound examination for the indications listed in the left column. “+” indicates that this component of the study is to be included. Refer to text for explanation of abbreviations not listed below:
- HCC – hepatocellular carcinoma, HBV – hepatitis B, HCV – hepatitis C, FLD –fatty liver disease, NAFLD – non-alcoholic fatty liver disease, Portal HT – portal hypertension, PUV – paraumbilical vein
Column 1
The list of request questions reflects our experience of how these questions are asked. There is deliberate overlap and duplication, which is intended to take account of variations in the way questions are framed.
Column 2
“Survey liver” is a careful survey of the entire liver with the main purpose being identification of focal lesions that may need further work-up for diagnosis or exclusion of HCC. This also provides the opportunity to assess for the presence of fatty liver disease.
Column 3
- 1
“Hi-res surface” (high resolution surface) – imaging optimised for near liver surface of left lobe using higher frequency probe (often linear) looking for surface nodularity (Figure 1)
- 2
“Hi res left lobe” (high resolution left lobe) – imaging optimized for internal examination of left lobe using higher frequency probe (Figure 1) looking for internal parenchymal nodularity
- 3
Hepatic vein wall examination preferably in segment 5 or 6. Imaging is optimised for high resolution display of a peripheral tributary of the right hepatic vein perpendicular to the ultrasound beam. It is important to obtain a perpendicular interface to create a good specular reflection. This is best achieved by coronal or oblique coronal imaging from the right side as shown in Figure 2. A peripheral tributary also allows higher resolution scanning. We aim to select a vein of at least 15 mm length and 3 mm diameter. We have shown previously that hepatic vein wall nodularity or waviness is a sensitive and specific sign of cirrhosis2 and our experience suggests that this is a substantially more sensitive sign than surface nodularity, although this is the subject of an ongoing study.

Patient with biopsy proven cirrhosis related to HBV. (a) Normal appearance on routine scanning. Higher frequency linear probe scanning of left lobe shows surface nodularity (b) and internal nodularity (c).
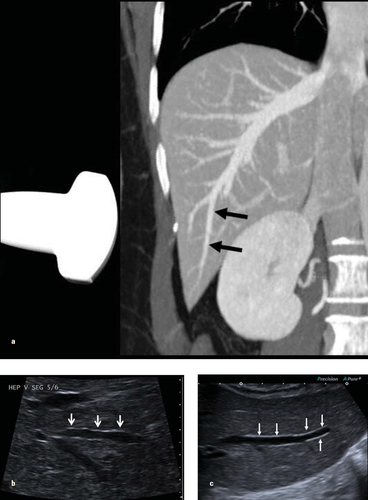
Hepatic vein wall scanning approach. (a) The coronal CT reformat displays the region of right hepatic vein tributary (arrows) examined in segment 5 or 6. The tributary should be perpendicular to the beam and quite peripheral to allow higher resolution scanning. (b) Right hepatic vein tributary (arrows) that shows waviness or nodularity indicative of cirrhosis (biopsy proven), in contrast to (c) a normal straight wall of a segment 5/6 hepatic vein.
We do not use a coarse liver echo pattern alone as a reliable sign of cirrhosis unless it is very pronounced (heterogeneously course) or supported by evidence of portal hypertension (see Column 4 below).
Fatty liver disease
Fatty liver disease (FLD) or steatohepatosis warrants some comments in this section. It is increasingly common and has a significant morbidity and mortality. It includes alcohol related FLD, non-alcoholic fatty liver disease (NAFLD), and NAFLD with a necroinflammatory component, namely non-alcoholic steatohepatitis (NASH). NAFLD may lead to both fibrosis and cirrhosis, portal hypertension and HCC.3
- 1
Mild FLD – slight increase in liver echogenicity. This is partly subjective and may be appreciated by an increase in liver to renal contrast echogenicity.
- 2
Moderate FLD – greater increase in echogenicity to the point that the portal tract echogenicity blends with the surrounding liver parenchyma, so that the portal veins become less distinct.
- 3
Marked FLD – as in (2) but with beam attenuation so that penetration is lost in the posterior part of the liver. Focal fatty sparing may be seen with grades 2 and 3.
Column 4
The ligamentum teres is examined for signs to indicate portal hypertension. These signs are the presence of a hypoechoic band of > 2.5 mm within the echogenic ligament, or the presence of a patent paraumbilical vein with hepatofugal venous flow. Both of these signs have been shown to be specific and in our experience together they represent the most sensitive ultrasound sign of portal hypertension.5,6 The technique has been described previously5
A complete portal hypertension examination is not included as the yield is likely to be lower in this clinical group. The presence of a positive ligamentum teres study is, however, of value in this group as it may add supporting evidence for cirrhosis if other findings are equivocal.
Column 5
If the clinical question includes “?portal hypertension” then the examination is extended as a formal Doppler study of the portal and hepatic venous system, including splenic size measurement.6
The report
The report is also “targeted” and includes the indication and a brief report to address the indication.
The report also includes a standard sentence to draw the referrer's attention to the focused nature of the study – “Note: this is a targeted examination to address the clinical question and does not include other abdominal organs unless otherwise indicated.”
Negative statements should be brief and normally only related to the specific clinical question.
Extension of the study and the report
This approach to targeted ultrasound of the liver should be viewed in practice as a guideline for scanning. Guidelines in medicine, by their nature, need to be applied with cognisance of the local clinical environment and do not remove the need to exercise clinical judgement in the individual patient. This applies to both sonographers and the supervising medical practitioners. Ready availability of consultation between sonographer and supervising medical practitioner, before or during the examination, is the best safeguard to ensure that the guidelines are not applied too rigidly.
The clinical request or findings during the examination may mean that the study should be extended. If the examination reveals something that is not clearly known from the request and is potentially significant, for example, the presence of ascites or biliary dilatation, or an obvious finding adjacent to the liver, the examination and the report should be extended appropriately.
Efficiency and accuracy issues
Examination times are substantially and often dramatically reduced when compared with the historical practice of performing comprehensive upper abdominal studies in this clinical group (the details of this reduction are currently being examined).
The impact on diagnostic yield or accuracy is not known and would be very difficult to establish. It is, however, plausible that accuracy with respect to the specific clinical questions may be higher as a result of scanning being more focused. Indeed our sonographers feel that liver scanning is more thorough and therefore likely to be more accurate even though the total examination time is less. This probably results from removal of the distraction and time pressures of completing a comprehensive and often unnecessary upper abdominal study.
Furthermore, there are efficiency gains in reporting time.
Optional matrix modification
The matrix is adaptable to local practice and preferences. Emerging technologies such as quantitative shear wave elastography can also be added as a means of grading fibrosis. The concept is simple so lends itself to such modification depending on local circumstances.
Conclusion
Targeted ultrasound of the liver (TUSL) provides a means of improving efficiency and possibly diagnostic accuracy in addressing the common clinical questions in chronic liver disease, an area of increasing burden on ultrasound services. It is simple to introduce and can be modified according to local preferences and technologies. As with all guidelines it does not supplant the need for the exercise of clinical judgement by the ultrasound team.