Fetal Gray Matter Heterotopia
Funding: This study was supported by China Society for Maternal and Child Health Research (Grant/Award Number: 2023CAMCHS003A17).
Abbreviations
-
- GMH
-
- gray matter heterotopia
-
- MRI
-
- magnetic resonance imaging
A pregnant woman underwent fetal brain magnetic resonance imaging (MRI) following ultrasound detection of a posterior fossa cyst at 29 weeks' gestation. She presented with no relevant medical history and underwent a routine obstetric examination during pregnancy. The fetal head position, fetal cranial development, and limb development remained normal until 29 weeks. A fetal MRI examination showed a posterior fossa cyst, and another nodular gray matter signal was observed adjacent to the right lateral ventricle. Follow-up MRI at 31 weeks + 3 days showed no major changes (Figure 1). The patient successfully delivered a male neonate at 40 weeks' gestation. A brain MRI was performed at 7 months of age and confirmed the diagnosis of fetal gray matter heterotopia (GMH) (periventricular type) (Figure 2). He showed no neurological abnormalities such as epilepsy. Moreover, his skin manifestations were normal, and his growth and development were consistent with his monthly age.
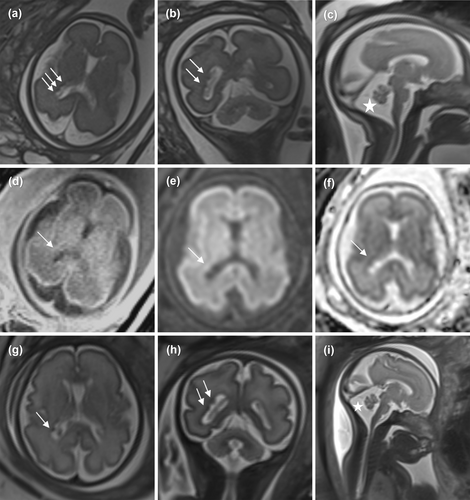
MRI imaging findings of fetal GMH. MRI findings of this lesion showed no significant changes at 29 weeks + 2 days of gestation (a–f) and 31 weeks + 3 days of gestation (g–i). (a–c, g–i) T2-half Fourier single-shot turbo spin echo sequence; (d) T1-weighted MRI; (e) diffusion-weighted MRI; and (f) a matching apparent diffusion coefficient map. MRI shows that the lateral ventricle is not smooth, and multiple abnormal signal nodules (arrow) can be seen within the wall of the lateral ventricle. The mid-sagittal MRI shows a widening of the cerebellomedullary cistern (star). GMH, gray matter heterotopia; MRI, magnetic resonance imaging.
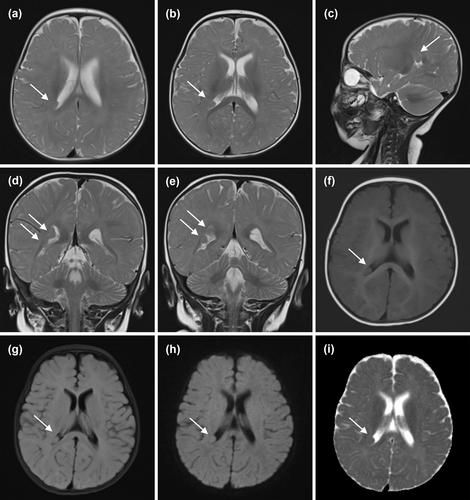
MRI findings of male neonate at 7 months with GMH. (a–e) T2-weighted MRI; (f) T1-weighted MRI; (g) T2-fluid-attenuated inversion recovery-weighted MRI; (h) diffusion-weighted MRI; and (i) a matching apparent diffusion coefficient map. A nodule was observed in the ventricular wall of the right lateral ventricular triangle, projecting into the ventricles (arrow). The signal was identical to the signal from the cerebral cortex in all sequences.
Fetal GMH is a relatively uncommon congenital disorder that arises from impaired neuronal migration. The three main types of GMH are periventricular nodular heterotopia, subcortical heterotopia, and subcortical band heterotopia. The most common type is periventricular nodular heterotopia, as found in the present case. GMH can sometimes be accompanied by other abnormalities, such as ventriculomegaly, agenesis of the corpus callosum, and congenital heart disease. Fetal MRI is increasingly being used to diagnose fetal GMH because of its high soft tissue resolution. However, there have been few reports of pathological or postnatally confirmed fetal GMH.
Author Contributions
Jiaojiao Liu: writing – original draft (lead). Lianxiang Xiao: conceptualization (lead), supervision (lead).
Acknowledgments
The authors have nothing to report.
Ethics Statement
This study was approved by Shandong Provincial Maternal and Child Research Ethics Approval (Approval No.: 2024-13).
Consent
The case was retrospectively analysed, the fetal and postnatal imaging data used were from previous medical records, and the images were anonymised, which does not pose a risk of compromising the patient's privacy. Therefore, informed consent was exempted.
Conflicts of Interest
This article belongs to a special issue (SI)—fetal imaging, maternal and children imaging. As the SI's guest editor, Professor Lianxiang Xiao is excluded from all the editorial decisions related to the publication of this article. The remaining author declares no conflicts of interest.
Citing Literature
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.