Retroperitoneal low-grade fibromyxoid sarcoma
Abstract
Introduction
Low-grade fibromyxoid sarcoma is an uncommon deep-seated soft-tissue sarcoma that occurs rarely in young adults and children. Although surgical resection provides a long-term prognosis, late local recurrence and metastasis may occur.
Case presentation
A 44-year-old woman with no prior medical history presented with breathing and abdominal discomfort. Contrast-enhanced computed tomography scan revealed a retroperitoneal tumor protruding into the thoracic cavity and pleural effusion on the left side. Tumor biopsy revealed sarcoma. We performed complete resection of the tumor along with part of the diaphragm and replaced the diaphragm with a prosthetic patch. Histopathologic findings indicated low-grade fibromyxoid sarcoma. The patient experienced no postoperative complications and received no adjuvant therapy. Furthermore, she survived 4 years after surgery without recurrence.
Conclusion
Complete surgical resection is effective for low-grade fibromyxoid sarcoma; therefore, it is important to plan appropriately for complete resection when biopsy reveals malignant findings.
Abbreviations & Acronyms
-
- LGFMS
-
- low-grade fibromyxoid sarcoma
-
- CT
-
- computed tomography
Keynote message
Low-grade fibromyxoid sarcoma (LGFMS)—also called Evans tumor—is a sarcoma that occurs unusually in young adults and even more rarely in the retroperitoneum. Although complete surgical resection is effective for LGFMS, late recurrence and metastasis may occur. Herein, we reported a case of LGFMS with no recurrence for 4 years after complete resection of the tumor, partial resection of the diaphragm, and diaphragmatic replacement.
Introduction
LGFMS is an uncommon sarcoma that frequently occurs in the deep soft tissues of proximal extremities or trunk in young adults but rarely in other sites, including internal organs.
LGFMS comprises deceptively bland-appearing spindle-shaped cells in a combination of collagenous and myxoid stroma.1-5 The disease causes delayed local recurrence and metastasis; however, in a small number of cases, surgical resection provides a long-term prognosis. In this case report, we described a rare case of LGFMS arising in the retroperitoneum as well as present a literature review.
Case presentation
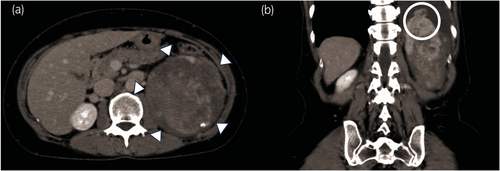
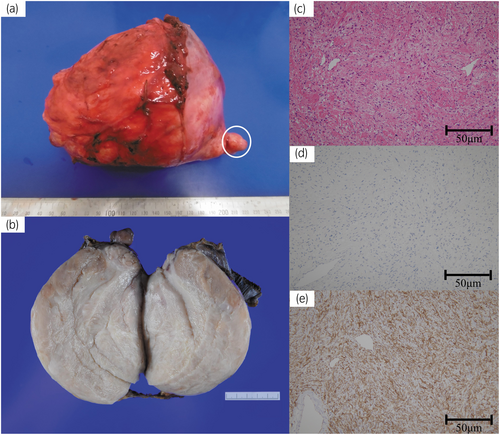
A 44-year-old woman was referred to our hospital with left abdominal discomfort lasting for >2 years and respiratory discomfort lasting for 6 months. Contrast-enhanced CT scan revealed an enhancing mass axis of 14 cm on the cranial side of the left kidney, which had invaded the left diaphragm and left thoracic cavity with pleural effusion on the left side (Fig. 1). No findings suggestive of metastasis for other internal organ were noted. Tumor markers, including carcinoembryonic antigen and carbohydrate antigen 19–9, revealed no abnormal findings. Moreover, echo-guided biopsy indicated the possibility of sarcoma, and the patient was referred to our hospital. Dissection of the retroperitoneal tumor was performed medially between the descending colon and the spleen, caudally between the kidney, and cranially with the diaphragm (Fig. 2a). Notably, 1000 mL of pleural fluid, which was pale and bloody, was collected, and the cytology was benign. The tumor was extensively resected, including the diaphragm, to obtain a sufficient margin. In addition to the retroperitoneal tumor, we found disseminated-like lesions in the left thoracic cavity, which were resected. To preserve as much diaphragm as possible, we removed the diaphragm on the dorsal side of the tumor (Fig. 2b). Furthermore, the diaphragm was reconstructed using a prosthetic patch, suturing the covering of the diaphragm where the diaphragm remained and the patch to the ribs and chest wall where the diaphragm did not remain (Fig. 2c). The operative time was 257 min, and the estimated blood loss was 510 mL. The maximum tumor diameter was 17 cm. The tumor was resected along with the diaphragm; moreover, the lesion protruding into the thoracic cavity, which was identified on CT scan, was removed (Fig. 3a). Gross pathological findings indicate that the cut surface of the tumor after formalin fixation was whitish, and the tumor was solid (Fig. 3b). Histologically, spindle-shaped cells were densely proliferated, but some areas had a slightly low cell density, with proliferation of collagen fiber bundles. Individual tumor cells were spindle-shaped to elliptical and had a nucleus with an irregular shape, weakly acidic cytoplasm, inconspicuous mitotic figures, and unclear background necrotic foci formation. The epithelioid region was observed in a small portion, and hyalinized nodules were confirmed. Immunohistochemistry indicated that the tumor was positive for MUC4, INI-1, bcl-2, and Ki-67 and negative for CD34, STAT6, MDM2, SMA, HHF35, desmin, S100, c-kit, WT1, calretinin, CD31, CK AE1/AE3, CK CAM5.2, EMA, and β-catenin (Fig. 3c–e). Notably, no malignant findings were observed in the intraoperatively resected disseminated-like lesions in the left thoracic cavity. The tumors were diagnosed as LGFMS owing to cell density differences, areas with hyalinized nodules, and lack of epithelioid areas. The patient had no complications and was discharged on postoperative day 8. No recurrence was observed for the following 4 years.

Discussion
The retroperitoneum is a rare primary site of LGFMS. To date, only eight cases, including ours, have been reported in the literature (Table 1).1-5 The chief complaint of primary retroperitoneal LGFMS depends on the location and size of the tumor. Histologically, LGFMS typically demonstrates contrasting fibrous and mucous-like zones, bland regular spindle-shaped cells, and spiral or spiral growth patterns.6 In our case, the histological findings were similar to those described above. MUC4 was positive in case 6 and in our case where immunostaining was performed. Positive immunostaining for MUC4 is strong evidence for the diagnosis of LGFMS.7
| No | Author/year | Age/gender/chief complaint | Location | Tumor resection | Radiation | Chemotherapy | Recurrence after initial surgery | Surgery for recurrence | Survival after initial surgery (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Goodlad JR1/1995 | 51/M/− | Retroperitoneum (psoas muscle) | Yes | – | – | Yes, at 72 months | No | 72 |
| 2 | Jannasch O2/2008 | 24/M/− | Retroperitoneum (pelvis) | Yes | Yes | No | No | – | 15 |
| 3 | Bayder DE5/2011 | 44/M/abdominal pain | Retroperitoneum | Yes | Yes | No | No | – | – |
| 4 | Wang G4/2017 | 48/M/no complain | Retroperitoneum (nearby right psoas muscle) | Yes | – | No | Yes, at 24 months (near right psoas major) | – | 24 |
| 5 | Ud Din N3/2018 | 29/F/− | Retroperitoneum | Yes | – | – | Yes, at 128 months | – | 204 |
| 6 | Ud Din N3/2018 | 18/F/− | Retroperitoneum | Yes | – | – | No | – | 36 |
| 7 | Ud Din N3/2018 | 61/M/− | Retroperitoneum | Yes | – | – | No | – | 55 |
| 8 | Our case | 44/F/discomfort of breathing | Retroperitoneum (nearby left kidney) | Yes | No | No | No | – | 48 |
- Treatment, recurrence, and outcomes in eight patients with LGFMS in the retroperitoneum from the literature, including our case. –: not mentioned.
Radical surgical resection of LGFMS is the general treatment. Although there is no established treatment for recurrent cases, surgical resection, chemotherapy, and radiation therapy have been reported as treatment options. Securing the resection margins is difficult because of the proximity of these retroperitoneal tumors to other surrounding organs. In the present case, the tumor appeared to invade the diaphragm grossly; however, pathologic findings revealed no diaphragmatic invasion, and most of the normal structure was preserved. Williams et al.8 reported a case of recurrence within 5 months after chemotherapy. Because of the low grade of malignancy of LGFMS and the associated low mitotic rate, chemotherapy and radiation therapy are unlikely to be effective.9 An incomplete excision margin is a risk factor for recurrence and metastasis.10 Cases with complete resection with free margins have a better 5-year local recurrence-free survival rate than those with microscopic or macroscopic residual tumor in the resected specimen.11 Moreover, Charoenlap et al.12 described unplanned excision for soft tissue sarcoma should be avoided because of its detrimental effect especially when residual tumor remains after unplanned excision. Scheer et al.11 also reported that resection margins ranged from 0.2 mm to 1.6 cm, and recurrence or metastasis was observed in these cases with resection margins of less than 0.2 cm. Thus, sufficient margins (at least 0.2 cm) should be taken to prevent postoperative recurrence. Therefore, the current approach is wide resection with negative margins and the patient may not require chemotherapy or radiation therapy.13 Accordingly, radical treatment should be pursued, but overly invasive surgery should be avoided. Nonetheless, the prognosis is relatively good if complete resection is possible.
Local recurrence has been reported from several years to 15 years.6 Charoenlap et al.12 reported patients were followed at least for 8 years after surgery including clinical and radiographic examination every 3–4 months in the first 2 years, 6 months for the next 2 years, and then every year. Therefore, based on this literature, we plan to follow up with CT scans at least every year for at least 10 years.
Conclusion
We reported a case of retroperitoneal LGFMS. We also found that complete surgical resection is effective for LGFMS. Therefore, it is important to plan appropriately for complete resection when biopsy reveals malignant findings.
Author contributions
Takeaki Noguchi: Writing – original draft. Takahisa Suzuki: Conceptualization; writing – review and editing. Yosuke Shibata: Writing – review and editing. Mitsuyuki Koizumi: Writing – review and editing. Kimito Osaka: Writing – review and editing. Takeshi Kishida: Writing – review and editing.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an Institutional Reviewer Board
Not applicable.
Informed consent
Written informed consent was obtained from the patient.
Registry and the Registration No. of the study/trial
Not applicable.