A case of bladder cancer after bilateral lung transplantation following bone marrow transplantation
Abstract
Introduction
The incidence of bladder cancer following transplantation is high; however, no previous studies have reported the development of bladder cancer following bone marrow and bilateral lung transplantations.
Case presentation
A 42-year-old man who was followed for bilateral lung transplantation due to chronic graft-versus-host disease following bone marrow transplantation complained of gross hematuria. Transurethral resection of the bladder tumor was performed for cT1N0M0 bladder cancer. On the following night, he experienced severe respiratory failure and was intubated. He was discharged on postoperative day 32 with the introduction of home oxygen therapy. The pathological diagnosis was invasive urothelial carcinoma, high-grade, pT1, with urothelial carcinoma in situ. Further treatment could not be performed because of his poor performance status and immunosuppressive state.
Conclusion
Vigorous screening for bladder cancer coexisting with other malignancies should be performed for transplant recipients for the early diagnosis and prompt treatment of a relatively aggressive bladder cancer.
Abbreviations & Acronyms
-
- BCG
-
- bacillus Calmette–Guerin
-
- CIS
-
- carcinoma in situ
-
- ICI
-
- immune checkpoint inhibitor
-
- POD
-
- postoperative day
-
- PS
-
- performance status
-
- TURBT
-
- transurethral resection of the bladder tumor
-
- UC
-
- urothelial carcinoma
Keynote message
Patients with bladder cancer following organ transplantation may have limited treatment indications. Transplant recipients should be screened for malignancies including bladder cancer.
Introduction
Previous studies have indicated a 1.5-fold incidence of bladder cancer following solid-organ transplantation.1 In particular, high-grade non-muscle-invasive bladder cancer was reported to be the most frequent among types of bladder cancer, and most of the cases occur following kidney transplantation.2 Herein, we report a case of bladder cancer that emerged following bilateral lung transplantation and bone marrow transplantation.
Case presentation
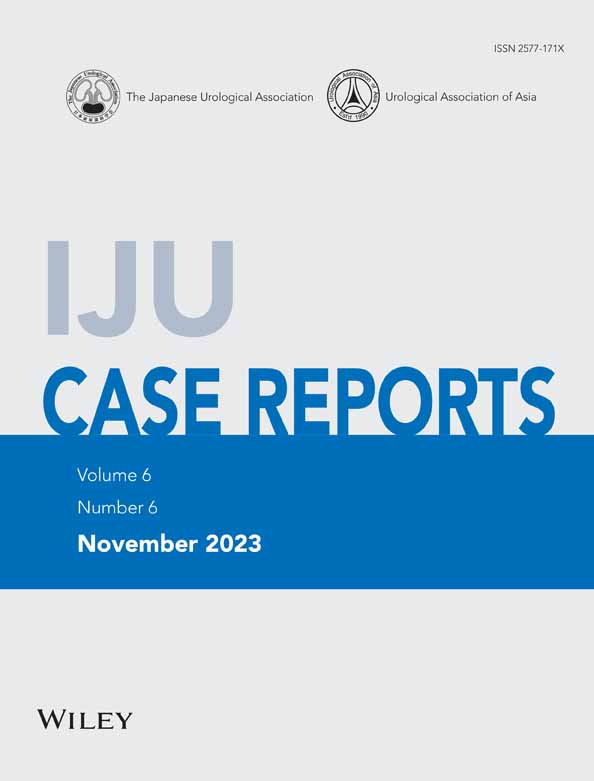
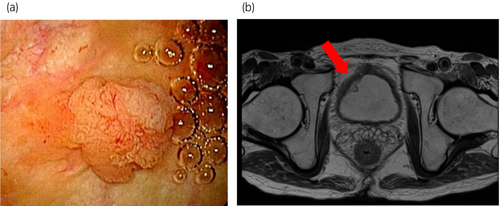
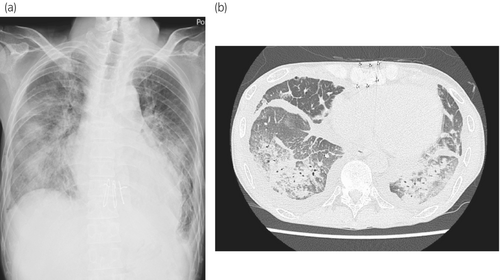
A 42-year-old man who was followed for bilateral lung transplantation for chronic graft-versus-host disease after bone marrow transplantation complained of gross hematuria. He was diagnosed with chronic myeloid leukemia 19 years ago and received bone marrow transplantation 8 years ago. Three years ago, he underwent bilateral lung transplantation. He was taking 1.5 mg of tacrolimus, 1000 mg of mycophenolate mofetil, and 9 mg of prednisolone as immunosuppressive agents. Cystoscopy showed a 10-mm solid tumor with a stalk at the dome of the bladder (Fig. 1a). Urine cytology was class V. The patient was referred to our hospital for further treatment. Magnetic resonance imaging showed a solid tumor without muscle invasion (Fig. 1b). No metastases to other organs or lymph nodes were found. With the clinical diagnosis of T1N0M0 bladder cancer, TURBT under spinal anesthesia was performed. The operative time was 51 min, with small blood loss, and fluid intake of 300 mL. He was admitted to a high care unit for respiratory care and discharged to the general ward on POD 1. However, at night, he experienced severe respiratory failure, for which he was intubated and transferred to the intensive care unit. Chest X-ray imaging and computed tomography showed severe congestion, consolidation, and ground-glass opacities in both lungs, suggesting fluid overload or pneumonia (Fig. 2a,b). After treatments by diuretics and antibiotics, he was again transferred to the general ward on POD 6 and discharged on POD 32 with the introduction of home oxygen therapy. The pathological diagnosis was invasive UC, high-grade, pT1, with UC in situ (CIS) component (Fig. 3a,b). The second TUR was not performed because of his poor PS and general condition. Intravesical BCG treatment was not performed because he was under treatment with immunosuppressive agent. During the observation period, he was incubated again because of respiratory failure 3 months postoperatively.
Discussion
The incidence of solid tumor after transplantation is higher than that in the general population.1 The standardized incidence ratio of bladder cancer in patients who underwent renal transplantation compared with the general population is two to three times higher,3, 4 with more advanced stage at presentation,5 suggesting poor prognosis of bladder cancer in this population. The exact reason for the high risk of incidence of bladder cancer following transplantation is unknown; however, one of the mechanisms can be the direct oncogenic effect of the long-term use of immunosuppressive agents, an immune-deficient status caused by immunosuppressive agents,3 or integration of BK polyomavirus into urothelial cells.6 Epidemiologically, the incidence of bladder cancer following renal transplantation in Asian populations is much higher than that in European populations.3 In addition, patients with HIV infection may have a higher risk for bladder cancer but much lower than other malignancies such as Kaposi sarcoma and non-Hodgkin lymphomas.7 This result might be due to confounding factors (e.g., smoking); however, the common feature of bladder cancer between patients with HIV infection and transplanted patients is the relatively aggressive histology of bladder cancer.8, 9 Although the precise mechanism is unclear, an immunosuppressive status and genetic or environmental factors can predispose the higher incidence of bladder cancer in patients with transplantation.
In this case, the second TUR was not performed because of poor PS. Considering the pathological diagnosis of invasive UC, high-grade, pT1 with urothelial CIS, this case was classified into the highest risk.10 If he had good respiratory status and good PS, prompt total cystectomy can be considered. Also, the reduction or withdrawal of immunosuppressive agents could be considered to reduce the risk of recurrence. In addition, we did not perform intravesical BCG treatment because he was taking immunosuppressive agents. Intravesical BCG administration can be a contraindication for patients with immunosuppressive status because of the higher risk of severe side effects or possible poor antitumor effects. However, several previous reports have indicated the safety of BCG for transplant recipients, including kidney, heart, and liver transplantations.11, 12 Considering publication bias and reports with a small number of cases, BCG should be used balancing the risks and benefits for the transplant recipients because bladder cancers in transplant recipients are often aggressive. Another possible treatment strategy would be weekly instillation of intravesical chemotherapy, but the protocol for intravesical chemotherapy is still controversial.10
Regarding the immunomodulatory effect of BCG, ICI for patients who underwent solid-organ transplantation is reported to induce the high incidence of graft loss. A review article reported 81% of graft loss with allograft transplantation, and the median time to rejection was 21 days.13 Another multi-center study showed the occurrence of acute rejection in 29 of 69 (42%) patients with the median time from ICI initiation to rejection of 24 days.14 A recent analysis using T-cell receptor sequencing showed one of the mechanisms for the acute rejection; alloreactive CD8+ T cells that remained in the transplanted kidney expand after ICI therapy and accumulate in the allograft to induce rejection.15 Strategies to avoid allograft rejection in ICI therapy is warranted considering the high incidence of bladder cancer in transplant recipients.
Since immunomodulatory agents such as BCG and ICI are the core treatment of bladder cancer, performing a standard therapy for organ recipients is challenging. On the contrary, an immunosuppressive state can contribute to the higher incidence of bladder cancer in organ recipients. To our knowledge, this is the first case report showing the development of bladder cancer following two organ transplantations. Although it is not clear whether the number of transplant organs affect the occurrence of bladder cancer, the long-term immunosuppressive state could influence the emergence of bladder cancer. According to a recommendation from the American Society of Nephrology, screening for bladder cancer is not recommended for kidney recipients,16 but no data are available for other solid-organ recipients. Further studies are warranted to establish an appropriate screening strategy for bladder cancer in solid-organ recipients. However, this case suggests that routine screening with urinalysis, urine cytology, or ultrasound with adequate filling of the bladder should be considered taking aggressiveness and limited therapeutic strategies into account. Also, patient and physician awareness of the relatively high incidence of bladder cancer is necessary for non-kidney organ transplants. Early detection of bladder cancer in those patients is crucial to provide favorable treatment outcomes for bladder cancer.
Conclusion
In transplant recipients, vigorous screening for bladder cancer and other malignancies should be performed for early diagnosis and prompt treatment for relatively aggressive bladder cancer.
Author contributions
Yutaro Arai: Conceptualization; data curation. Yusuke Goto: Funding acquisition; methodology; project administration; writing – original draft; writing – review and editing. Tomokazu Sazuka: Supervision; writing – review and editing. Ayumi Fujimoto: Data curation; writing – review and editing. Hiroaki Sato: Data curation; investigation; project administration. Yusuke Imamura: Supervision. Shinichi Sakamoto: Supervision. Masayuki Ota: Data curation; writing – review and editing. Jun-ichiro Ikeda: Supervision. Tomohiko Ichikawa: Supervision; writing – review and editing.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an Institutional Reviewer Board
This study is approved by our institutional ethical reviewer board and the approval number is 2554.
Informed consent
Informed consent was obtained from the patient.
Registry and the Registration No. of the study/trial
Not applicable.