Complete response to pembrolizumab for metastatic urothelial carcinoma in the renal pelvis of allograft kidney
Abstract
Introduction
We present a case of urothelial carcinoma in a renal allograft successfully treated with pembrolizumab.
Case presentation
A 39-year-old woman presented with nausea and anorexia 9 years after a renal transplantation. Positron emission tomography revealed a neoplasm of the renal pelvis of the allograft and multiple lymph nodes with peritoneal metastasis. A diagnosis of a non-muscle-invasive bladder tumor with peritoneal dissemination and jejunal metastasis of urothelial carcinoma was made. After five cycles of gemcitabine and carboplatin, the tumor progressed and pembrolizumab was administered. One week after the first dose, the allograft was rejected, necessitating arterial embolization. After the second cycle, the patient developed Stevens-Johnson syndrome. After discontinuing pembrolizumab, positron emission tomography revealed no increased tumor activity. A complete response was achieved for 21 months without additional treatment.
Conclusion
Pembrolizumab was effective in treating urothelial carcinoma of the renal allograft; however, allograft rejection and loss should be considered.
Abbreviations & Acronyms
-
- CR
-
- complete response
-
- CT
-
- computed tomography
-
- FDG PET/CT
-
- fluoro-2-deoxyglucose positron emission tomography/computed tomography
-
- ICI
-
- immune checkpoint inhibitor
-
- TURBT
-
- transurethral resection of bladder tumor
-
- UC
-
- urothelial carcinoma
Keynote message
UC of a renal allograft after kidney transplantation is rare. Pembrolizumab can increases the risk of rejection in kidney transplant patients. Our patient with an unresectable UC of the renal allograft achieved a complete response to pembrolizumab but with severe allograft rejection. The risk of rejection should be considered when administering pembrolizumab in patients receiving kidney transplant.
Introduction
The incidence of malignancy after kidney transplantation is higher than that in the general population. Most cases of de novo UC occur in the bladder, and UC of renal allografts is very rare.(1-5) The safety and efficacy of pembrolizumab have not been established for solid organ transplant recipients requiring immunosuppressive therapy to prevent allograft rejection.(6, 7) We report the first case of metastatic UC of a renal allograft successfully treated with pembrolizumab, accompanied by severe allograft rejection and loss.
Case presentation
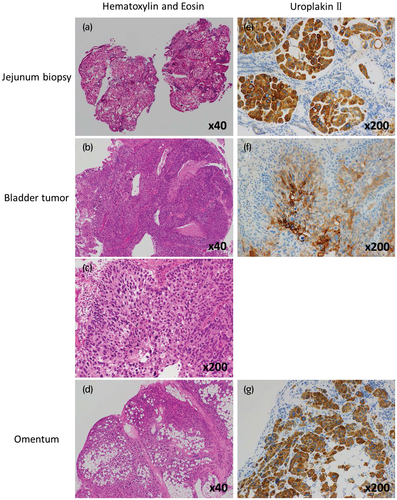
A 39-year-old woman presented with nausea and anorexia at the department of gastroenterology of our institute. She had received living renal transplantation 9 years prior from her father with the same blood type, and had no remarkable transplantation-associated complications or abnormal findings in follow-up urinalysis while under an immunosuppression regimen of 3 mg tacrolimus and 5 mg prednisolone daily. Abdominal CT demonstrated jejunal wall thickness, and biopsies of the jejunal stenosis suggested poorly differentiated metastatic carcinoma, although the primary tumor site could not be detected (Fig. 1a). Pelvic CT revealed bilateral ovarian cysts and bladder tumors, and cystoscopy showed a 2-cm papillary tumor in the bladder neck.
Left ovariectomy, right ovarian cystectomy, and TURBT were performed. Multiple peritoneal dissemination nodules were intraoperatively observed, and nodules of the omentum were diagnosed as malignant by an intraoperative rapid diagnostic method. Therefore, a gastrojejunostomy was performed to bypass the intestinal tract.
The histopathological diagnosis was high-grade invasive UC of the bladder (pT1) (Fig. 1b,c) and benign cystic changes in the bilateral ovary. Immunohistochemical staining of the jejunum biopsy sample and the nodules of the omentum showed similar findings to the bladder tumor, consistent with metastasis of UC (Fig. 1a–g). However, the peritoneal dissemination and jejunal metastasis showed atypical patterns of progressive non-muscle-invasive bladder UC. Urine cytology consistently showed class V after TURBT. Pelvic CT and FDG PET/CT revealed a tumor at the renal pelvis of the allograft (Fig. 2a,b) with supraclavicular, axillary, and mediastinal lymph node and jejunal metastases (Fig. 2c–e). Therefore, the primary site was clinically diagnosed as the renal pelvis of the allograft.
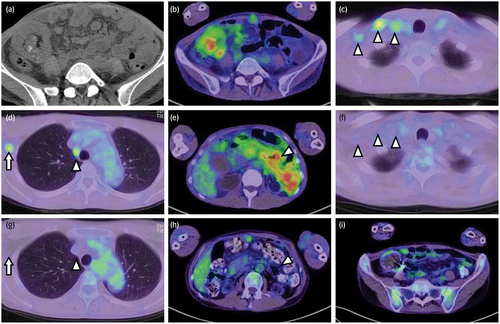
The patient underwent five cycles of systemic chemotherapy with gemcitabine (1000 mg/m2) and carboplatin (area under the concentration-time curve = 4) without changing immunosuppressants, considering the impaired renal function (serum creatinine level = 3.12 mg/dL); however, FDG PET/CT showed disease progression. Before using pembrolizumab as second-line chemotherapy, we proposed an allograft nephroureterectomy; however, she refused the nephroureterectomy, even though she understood the risk of allograft rejection, severe adverse events, and mortality. After starting pembrolizumab (200 mg) and discontinuing tacrolimus, serum creatinine levels increased and she developed a fever of 39°C on the seventh day following pembrolizumab administration. Abdominal CT showed remarkable swelling of the allograft, and antibiotic treatments did not alleviate the fever and inflammation, suggesting allograft rejection; the serum creatinine level increased to 9.96 mg/dL, necessitating hemodialysis. After performing allograft arterial embolization, the fever and severe inflammation quickly improved and the second dose of pembrolizumab was administered while tapering the prednisolone dose (Fig. 3). Before the third pembrolizumab administration, she developed Stevens–Johnson syndrome, requiring 30 mg/day prednisolone, and pembrolizumab administration was discontinued.
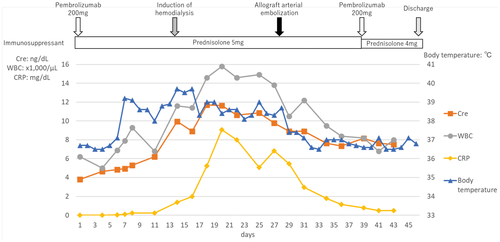
The prednisolone dose was discontinued completely after 7 months; however, FDG PET/CT showed no increased accumulation of FDG at any tumor sites continuously, and a CR was achieved for 21 months without any additional treatment for UC under maintenance hemodialysis (Fig. 2f–i).
Discussion
The incidence of de novo malignancy after kidney transplantation is approximately 3–5 times higher than that in the general population,(8-10) which may be due to long-term immunosuppressive therapy. The incidence of de novo UC is approximately 0.2–1.0%, whereas UC of a renal allograft is rare (0.02–0.05%).(1, 2, 5, 10, 11) The treatment for localized UC of a renal allograft is allograft nephroureterectomy, although the prognosis of patients with metastatic or recurrent cases is poor.(1, 3, 5, 12, 13)
To our knowledge, this is the first case of metastatic UC of a renal allograft treated with pembrolizumab to achieve a CR. The safety and efficacy of ICIs for solid organ transplant recipients have not yet been established. Previous studies reported a 28.9–40% overall response with 40.1–61.5% allograft rejection and 20–26.2% death secondary to rejection among kidney transplant recipients receiving ICI treatment.(6, 7, 14, 15) In our case, only prednisolone was continued when starting pembrolizumab to avoid reducing the anti-tumor effect of pembrolizumab. In contrast, a recent study reported that use of a mammalian target of rapamycin inhibitor and triple-agent immunosuppression was significantly associated with a low risk of graft rejection.(15) This study suggested that our decision to reduce the immunosuppressant dose may have increased the risk for graft rejection, despite strengthening the efficacy of pembrolizumab.
A limitation is that we failed to evaluate whether the primary tumor originated from the donor urothelial cells with genetic analysis. The risk of upper tract UC developing bladder tumors is approximately 10 times higher than that of bladder tumors developing upper tract UC (30–40% vs. 2–6%).(16, 17) Therefore, we believe that there is a higher possibility that the tumor of the renal pelvis allograft was the primary tumor in this case, which then developed to the bladder.
In summary, we report the first case of metastatic UC of a renal allograft successfully treated with pembrolizumab. Severe allograft rejection required arterial embolization, but a CR was achieved.
Acknowledgments
The authors thank the patient for participating in this case report.
Author Contributions
Jun Kamei: Data curation; methodology; writing – original draft. Hirotaka Yokoyama: Data curation. Toshiro Niki: Investigation; supervision. Ryosuke Suda: Data curation; investigation; writing – review and editing. Toru Sugihara: Supervision; writing – review and editing. Akira Fujisaki: Supervision; writing – review and editing. Satoshi Ando: Investigation; supervision. Daiki Iwami: Supervision. Tetsuya Fujimura: Supervision; writing – review and editing.
Conflict of interest
The authors declare no conflict of interest.
Approval of the research protocol by an institutional reviewer board
A19-199.
Informed consent
Written consent was obtained.
Registry and the registration no. of the study/trial
Not applicable.