The effects of low-dose anthracycline-based chemotherapy on the levels of serum NT-proBNP level and left ventricular systolic and diastolic dysfunctions: A prospective observational study
Fatemeh Mohammadi and Leila Bigdelu contributed equally to the present study as the first author.
Abstract
Background and Aims
The present study aimed to evaluate the relationship between serum N-terminal (NT)-pro-brain natriuretic peptide (BNP) levels and incidence of left ventricular (LV) systolic and diastolic dysfunction in patients who underwent low-dose anthracycline chemotherapy.
Methods
This observational, prospective study was conducted on all patients with proven breast cancer, Hodgkin lymphoma, or non-Hodgkin lymphoma and no history of previous cardiac or any chronic diseases who were candidates for low-dose anthracycline chemotherapy from March 2017 to February 2018. We evaluated the serum NT-proBNP level and performed trans-thoracic echocardiography at baseline, 6, and 9 months after the chemotherapy.
Results
Among 57 patients who successfully finished the study, 13 (22.8%) patients were men and 44 (77.19%) patients were women, and the total mean age was 52 ± 14.86 years. Our results revealed that the LV systolic and diastolic function and NT-proBNP mean levels were in the normal range at all three measured times. Additionally, no significant differences were observed between the levels of NT-proBNP, LV systolic, and diastolic function at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline (p = 0.6, 0.1, and 0.4, respectively).
Conclusion
Following low-dose anthracycline chemotherapy, none of our patients encountered LV systolic and diastolic dysfunctions and changes in serum NT-proBNP level. However, further studies with a larger population, longer follow-up duration, and higher dosage of anthracyclines are required to determine the effects of low-dose anthracycline on NT-proBNP level and LV systolic and diastolic functions.
1 INTRODUCTION
Anthracyclines are well-known and highly effective anticancer drugs frequently used for a wide range of malignancies.1 However, dose-dependent cardiotoxicity is the major limitation of administering these drugs.2 Acute toxicity following anthracycline is reversible and occurs a few days after infusion. In contrast, chronic toxicity is irreversible and mostly happens within 1–3 months or even years after administering anthracycline.3 Congestive heart failure is the most common type of anthracycline-induced chronic cardiac toxicity, with a poor prognosis.4, 5 Therefore, early diagnosis of chemotherapy-induced cardiotoxicity and left ventricular dysfunction is of high clinical importance.6 In this regard, the most common way to monitor cardiac function is estimating left ventricular ejection fraction (LVEF) using echocardiography.7 However, determining LVEF cannot detect early changes and toxicities and is costly and challenging.8 Therefore, there is great interest in finding a sensitive, accessible, and cost-effective circulating biomarker to detect anthracycline-induced cardiotoxicity early.9
N-terminal (NT)-pro-brain natriuretic peptide (BNP) is one of the suggested biomarkers secreted in response to ventricular wall tension and is associated with heart failure.10 It has been emphasized that BNP leads to natriuresis, diuresis, and vasodilation. Some studies have reported enhanced plasma levels of NT-proBNP following chemotherapy with anthracycline.11 However, the prognostic role of NT-proBNP and the correlation between NT-proBNP and LV dysfunction following chemotherapy with anthracycline is still controversial.
Therefore, the present study aimed to evaluate the relationship between serum NT-proBNP levels and LV systolic and diastolic dysfunction in patients who underwent chemotherapy with a low-dose anthracycline.
2 METHODS
2.1 Ethical statement
This study was confirmed by the ethics committee of Mashhad University of Medical Sciences (approval code. IR.MUMS.fm.REC.1395.260). All participants received and signed written informed consent.
2.2 Study design
The prospective observational study was conducted in the general department of Imam Reza and Ghaem Hospitals affiliated with Mashhad University of Medical Sciences, Mashhad, Khorasan Razavi province, Iran, from March 2017 to February 2018. Anthracycline was administered with 60 mg/m2 in four courses (cumulative dose = 240 mg/m2) in breast cancer patients, and with 50 mg/m2 in six to eight courses (cumulative dose = 300–400 mg/m2) in Hodgkin and non-Hodgkin lymphoma patients. The NT-proBNP level and transthoracic echocardiography were performed for all enrolled patients at the beginning of the study and 6 and 9 months after the chemotherapy. Noteworthy, one echocardiography specialist did all echocardiography.
2.3 Inclusion and exclusion criteria
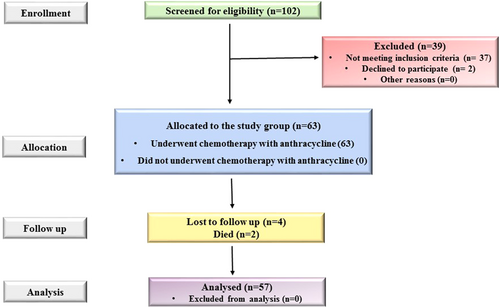
Our inclusion criteria were patients with proven breast cancer, Hodgkin lymphoma, or non-Hodgkin lymphoma, and no history of previous cardiac disease who underwent chemotherapy with anthracycline referred to the general department of Imam Reza and Ghaem Hospitals from March 2017 to February 2018. In contrast, the exclusion criteria were patients with a previous history of chemotherapy with anthracycline, diabetes, history of cardiac disease, moderate to severe valvular heart disease, hypertension, and liver or kidney or thyroid dysfunction. In this context, 102 patients with proven these cancers were included in our study, whereas only 63 patients had eligibility and were allocated to the study (Figure 1).
2.4 Evaluation of outcome
The demographic patients’ information was collected, including age, sex, dyslipidemia, smoking, and type of cancer. Furthermore, the serum NT-proBNP level and echocardiography results, including E/A ratio, E/e′ ratio, LVEF, left ventricular end-diastolic volume (LVEDV), left ventricular end-systolic volume (LVESV), left atrial volume (LAV), and tricuspid annular plane systolic excursion (TAPSE), were evaluated at 0, 6, and 9 months after the chemotherapy.
Diastolic dysfunction was evaluated using the E/A ratio, representing the ratio of the early (E) to late (A) ventricular filling velocities and the E/e′ ratio, which is the ratio of early diastolic mitral flow velocity to early diastolic septal annular velocity. Normal ranges for LVEF were 50%–70%, and the normal ranges for other evaluated echocardiography results were according to the American society of echocardiography chamber quantification guidelines.12 In addition, the normal NT-proBNP levels are less than 125 pg/ml for <75 years and less than 450 pg/ml for ≥75 years old.
2.5 Statistical analysis
Data were analyzed using the SPSS version.22 statistical software (SPSS Inc.) and GraphPad Prism 8.01 software (GraphPad Software Inc.) and were expressed according to the nature of parametric and nonparametric as means± SD or number with percentage, respectively. The normality of the data was checked with the Kolmogorov–Smirnov test. As appropriate, the comparison between continuous variables was performed using repeated measures of ANOVA for parametric data or the Freedman test for nonparametric data. The p values (p) ≤ 0.05 were considered statistically significant.
3 RESULTS
3.1 Study population
Among the 57 patients who successfully finished the study, 13 (22.8%) patients were men, and 44 (77.19%) patients were women, and the total mean age was 52 ± 14.86 years, with the range of 16–78 years (Table 1). In addition, 5 (8.8%) subjects had dyslipidemia and 3 (5.3%) were smokers (Table 1). The number of patients with breast cancer, Hodgkin lymphoma, and non-Hodgkin lymphoma was 33 (57.89%), 13 (22.8%), and 11 (19.22%), respectively (Table 1).
| Characteristic | N | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 13 | 22.8 |
| Female | 44 | 77.19 |
| Dyslipidemia | ||
| Yes | 5 | 8.8 |
| No | 52 | 91.2 |
| Smoke | ||
| Yes | 3 | 5.3 |
| No | 54 | 94.7 |
| Cancer | ||
| Breast | 33 | 57.89 |
| Hodgkin lymphoma | 13 | 22.8 |
| Non-Hodgkin lymphoma | 11 | 19.29 |
3.2 The echocardiographic results of patients at baseline, 6, and 9 months after chemotherapy with anthracycline
The E/A and E/e′ ratios, as indexes of diastolic dysfunction, did not significantly change between the baseline, 6, and 9 months after chemotherapy (p = 0.4, and 0.2, respectively). The mean level of E/A ratio was 1.0679 ± 0.78 at baseline, 0.9308 ± 0.37 after 6 months, and 1.0786 ± 0.94 after 9 months of chemotherapy with low-dose anthracycline (p = 0.4, Table 2). Furthermore, the mean level of E/e′ ratio at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline was 6.4907 ± 1.81, 6.5871 ± 1.83, and 6.4580 ± 1.85, respectively (p = 0.2, Table 2).
| Criteria | Before | After 6 months | After 9 months | p Value |
|---|---|---|---|---|
| E/A ratio | ||||
| Mean ± SD | 1.0679 ± 0.78 | 0.9308 ± 0.37 | 1.0786 ± 0.94 | 0.4a |
| Min | 0.4 | 0.3 | 0.12 | |
| Max | 1.7 | 1.6 | 1.8 | |
| E/e' ratio | ||||
| Mean ± SD | 6.4907 ± 1.81 | 6.5871 ± 1.83 | 6.4580 ± 1.85 | 0.2b |
| Min | 4.00 | 4.00 | 4.00 | |
| Max | 9.77 | 9.80 | 9.55 | |
| LVEF (%) | ||||
| Mean ± SD | 54.263 ± 3.159 | 53.8463 ± 3.733 | 54.65 ± 2.945 | 0.1a |
| Min | 42.0 | 39.0 | 40.0 | |
| Max | 62.0 | 61.0 | 60.0 | |
| LVEDV (ml) | ||||
| Mean ± SD | 91.123 ± 9.836 | 90.808 ± 8.659 | 92.039 ± 9.836 | 0.07a |
| Min | 78.0 | 77.0 | 78.0 | |
| Max | 111.0 | 107.0 | 110.0 | |
| LVESV (ml) | ||||
| Mean ± SD | 33.860 ± 12.111 | 33.885 ± 11.848 | 34.610 ± 12.352 | 0.1a |
| Min | 19.0 | 19.0 | 19.0 | |
| Max | 57.0 | 55.0 | 57.0 | |
| LAV (ml) | ||||
| Mean ± SD | 34.768 ± 7.691 | 35.412 ± 7.579 | 35.26 ± 7.594 | 0.07b |
| Min | 19.0 | 20.0 | 21.0 | |
| Max | 46.0 | 50.0 | 49.0 | |
| TAPSE (cm) | ||||
| Mean ± SD | 2.137 ± 0.38 | 2.104 ± 0.31 | 2.096 ± 0.34 | 0.3a |
| Min | 1.6 | 1.6 | 1.1 | |
| Max | 3.2 | 3.1 | 3.0 |
- Abbreviations: LAV, left atrial volume; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; LVESV, left ventricular end-systolic volume; TAPSE, tricuspid annular plane systolic excursion.
- a Comparing between the results of baseline, 6, and 9 months after chemotherapy using repeated measures of ANOVA.
- b Comparing the results of baseline, 6, and 9 months after chemotherapy using Friedman test.
Our results also showed that the mean levels of LVEF, LVEDV, LVESV, and LAV were in the normal range (Table 2). Moreover, there were no significant differences between all three measured times after chemotherapy with low-dose anthracycline (Table 2). The mean LVEF level at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline was 54.263 ± 3.159%, 53.8463 ± 3.733%, and 54.65 ± 2.945%, respectively (Table 2, p = 0.1). Additionally, the mean LVEDV was 91.123 ± 9.836 ml at baseline, 90.808 ± 8.659 ml after 6 months, and 92.039 ± 9.836 ml after 9 months of treatment with an anthracycline (Table 2, p = 0.07). Moreover, the mean LVESV level at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline was 33.860 ± 12.11, 33.885 ± 11.848, and 34.61 ± 12.352 ml, respectively (Table 2, p = 0.1). The mean LAV was 34.768 ± 7.691 ml at baseline, 35.412 ± 7.579 ml after 6 months, and 35.26 ± 7.594 ml after 9 months of treatment with an anthracycline (Table 2, p = 0.07).
In our study, we also evaluated the TAPSE levels as a marker of systolic function. Our results showed that the mean levels of TAPSE were in the normal range, and no significant differences were observed between all three measured times after chemotherapy with low-dose anthracycline (Table 2). The mean TAPSE levels were 2.137 ± 0.38 cm at baseline, 2.104 ± 0.31 cm after 6 months, and 2.096 ± 0.34 cm after 9 months of chemotherapy with low-dose anthracycline (Table 2, p = 0.3).
3.3 The NT-proBNP level at baseline, 6, and 9 months after chemotherapy with anthracycline
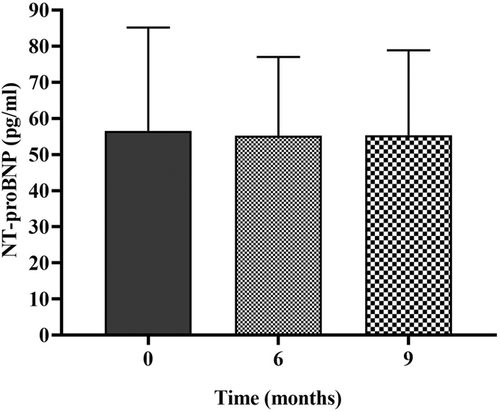
As illustrated in Figure 2, our results revealed that the NT-proBNP mean levels were in the normal range at all three measured times, and there were no significant differences between the levels of NT-proBNP at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline. The NT-proBNP level at baseline, 6, and 9 months after chemotherapy with low-dose anthracycline was 56.5511 ± 28.348, 55.2410 ± 21.778, and 55.38± 23.51 pg/ml, respectively (Figure 2, p = 0.6).
4 DISCUSSION
This observational, prospective, cross-sectional study was conducted on all patients with proven breast cancer, Hodgkin lymphoma, or non-Hodgkin lymphoma and no history of previous cardiac or any chronic disease who underwent chemotherapy with low-dose anthracycline from March 2017 to February 2018. The present study's findings indicated that none of our patients experienced LV systolic and diastolic dysfunction or NT-proBNP increment following the chemotherapy with a low-dose anthracycline.
Anthracyclines, including doxorubicin, daunorubicin, and epirubicin, are considered highly prescribed anticancer drugs used to treat many hematologic and solid malignancies.13, 14 It has been emphasized that acute toxicity following chemotherapy with anthracycline may manifest as ST-segment and T-wave abnormalities. In contrast, late anthracycline cardiotoxicity mainly consists of congestive heart failure and LV dysfunction.15 However, the prevalence and severity of late anthracycline cardiotoxicity are strongly correlated with the cumulative dose, method and duration of administration, previous treatment with other antineoplastic agents, presence of any underlying cardiac disorders, and the demographics of the patient.16 Interestingly, the prevalence of cardiotoxicity significantly propagated when patients were given doses of doxorubicin >550 mg/m2.17 In the present study, none of our patients experienced LV systolic and diastolic dysfunction following the chemotherapy with a low-dose anthracycline. However, we performed our investigations on patients who received low-dose anthracycline chemotherapy. The anthracycline dosage was 60 mg/m2 in four courses in breast cancer patients and 50 mg/m2 in six to eight courses in lymphoma patients. Therefore, our patients' lack of systolic and diastolic dysfunction may be due to the low dose of anthracycline administered in this study.
Several studies investigated the prognostic role of NT-proBNP in diagnosing anthracycline-induced cardiotoxicity. However, the results are controversial, consisting of either no association or correlation between the levels of NT-proBNP and decreased LVEF. The results of the present study showed no increment in NT-proBNP levels, LV systolic and diastolic dysfunction, as well as no relation between the NT-proBNP level and LVEF in patients following chemotherapy with low-dose anthracycline. However, our patients had no previous history of cardiac or other chronic disorders, including diabetes, liver dysfunction, and kidney dysfunction. In accordance with our results, Dodos and co-workers revealed that the LVEF, fractional shortening, and E/A ratio markedly diminished, while Tei Index significantly enhanced following the 6 and 12 months after anthracycline-based chemotherapy in healthy patients. Although these changes, these cardiac markers have remained within the normal range during the follow-up. Additionally, the mean NT-proBNP levels did not meaningfully change following anthracycline-based chemotherapy.18 Similarly, Sawaya et al. evaluated 43 patients with HER-2-overexpressing breast cancer receiving doxorubicin 240 mg/m2 for 6 months. They excluded patients with LVEFs < 50%, not all patients with a previous history of cardiac diseases, diabetes mellitus, and hypercholesterolemia. They reported that nine patients (20.93%) encountered cardiotoxicity 6 months after chemotherapy with an anthracycline. No significant differences were observed in the results of systolic and diastolic blood pressure, heart rate, LVEDV, LV end-diastolic diameter, LAV, and NT-proBNP level between the baseline and 6 months after chemotherapy with an anthracycline. In addition, the LVESV significantly increased while the LVEF decreased after 6 months of chemotherapy with anthracycline.19 These two studies demonstrated that LV systolic and diastolic functions and NT-proBNP level parameters could not predict anthracycline-induced cardiotoxicity.
In contrast, Sandri and co-workers conducted a cross-sectional study on 52 patients treated with high-dose chemotherapy for aggressive malignancy. Similar to our study, they excluded patients with a history of ischemic, valvular, or hypertensive heart disease, uncontrolled hypertension, and LVEF < 50%. They found that 17 (33%) patients had persistently increased, 19 patients (36%) had only transient increases, and 16 (31%) had no increases in NT-proBNP levels at 72 h after chemotherapy. They also showed that only patients with persistently increased NT-proBNP significantly worsened the left ventricular diastolic indexes from baseline to 12 months after chemotherapy.20 The increment in NT-proBNP levels in 33% of healthy patients in this study may be due to high-dose chemotherapy. Additionally, Romano et al. investigated 71 patients with breast cancer and without a history of coronary artery disease who were treated with not-high-dose chemotherapy (NHDC) with an anthracycline. They showed that 50 patients had normal or transiently elevated NT-proBNP levels (Group A), while 21 patients had persistently elevated NT-proBNP levels (Group B) after NHDC with anthracycline. Moreover, they reported that no patients encountered LVEF < 50% in both groups following 3, 6, and 12 months after NHDC. Patients in Group A showed no significant changes in LVEF, EDV, and ESV; however, patients in Group B had a notable reduction in LVEF, while increasing EDV and ESV compared to the baseline and Group A. However, they did not exclude patients with hypertension, diabetes mellitus, and hypercholesterolemia, which may be the reason for changes in NT-proBNP levels and cardiac function.21 Feola and co-workers also evaluated the effects of anthracycline chemotherapy in 53 patients with breast carcinoma. They determined that the BNP level remarkably propagated, while LVEF significantly alleviated following 1 and 2 years after chemotherapy in all patients. However, patients with a reduction of LVEF > 10% showed higher BNP levels during the follow-up, while all patients had LVEF > 50%. Additionally, they did not exclude all patients with previous cardiovascular and other chronic diseases, and 40% had hypertension.22 These studies suggested that persistently increased NT-proBNP after administration of anthracycline is strongly associated with the development of chemotherapy-induced cardiotoxicity. However, the effects of high dosage of anthracycline and other underlying chronic disorders on the pro-BNP level and LVEF is still under discussion.
5 CONCLUSION
In summary, our results revealed that none of the patients without a history of previous cardiac or any chronic disease encountered LV systolic and diastolic dysfunction and changes in the serum NT-proBNP level following the chemotherapy with low-dose anthracycline. However, further studies with a larger population, longer follow-up duration, and different doses of anthracycline are required to clearly determine the relationship between NT-proBNP level and LV systolic and diastolic function following chemotherapy with an anthracycline.
AUTHOR CONTRIBUTIONS
Fatemeh Mohammadi: data curation; investigation. Leila Bigdelu: conceptualization; funding acquisition; investigation; methodology. Abolghasem Allahyari: conceptualization; investigation; methodology. Negar Morovatdar: data curation; formal analysis. Vafa Baradaran Rahimi: formal analysis; writing – original draft; writing – review & editing.
ACKNOWLEDGMENT
This study was financially supported by the research council of Mashhad University of Medical Sciences (Grant Number: 951149).
CONFLICT OF INTEREST
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Vafa Baradaran Rahimi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon reasonable request.