Normal Blood Pressure, High Normal Blood Pressure, and Risk of Incident Atrial Fibrillation: A Population-Based Cohort Study
ABSTRACT
Background and Aims
This study aimed to investigate the association between normal BP, (blood pressure [BP] 120–129/80–84 mmHg), and high normal BP, (BP 130–139/85–89 mmHg), compared to optimal BP, and risk of atrial fibrillation (AF).
Methods
A population-based cohort study was performed including inhabitants of Västerbotten County, Sweden, aged 30–60 years without AF at inclusion who participated in health examinations in 1988–2014. Approximately 40% of participants had ≥ 2 health examinations. The health examination included a questionnaire and measurement of BP, weight, height, and glucose. Cox regression with time-updated covariates was used to estimate the association between BP and AF risk. Restricted cubic spline analyses were performed.
Results
The cohort included 109,697 persons with 162,982 observations and a mean follow-up of 13.6 years. Incident AF was diagnosed in 5260 participants. We found an increased risk of incident AF associated with normal BP (hazard ratio [HR] 1.13, 95% confidence interval [CI] 1.01–1.27) and high normal BP (HR 1.23, 95% CI 1.10–1.38) compared to optimal BP after multivariable adjustment. Systolic BP and diastolic BP in 10 mmHg increments were associated with risk of incident AF, with HRs of 1.11 (95% CI 1.10–1.13) and 1.13 (95% CI 1.09–1.16), respectively, in multivariable models. A restricted cubic spline analysis indicated that the AF risk increased gradually with increasing systolic and diastolic BP.
Conclusion
Individuals with both normal BP and high normal BP have an increased risk of developing incident AF. The risk of AF increased gradually with increasing systolic and diastolic BP.
1 Introduction
Atrial fibrillation and atrial flutter (AF) are the most common clinically significant arrhythmias and have an incidence of 4.0 per 1000 person-years [1]. Hypertension is an important risk factor for AF [2, 3]. Less is known about the possible link between normal blood pressure (BP) (defined as 120–129/80–84 mmHg) and high normal BP (defined as 130–139/85–89 mmHg) and AF risk. Some, but not all, studies have shown an association between increased BP (but < 140/90 mmHg) compared to optimal BP (defined as BP < 120/80), and AF risk [4-9].
Previous studies of BP as a risk factor for incident AF have predominantly assessed BP at a single measurement [6]. As an individual's BP is apt to change over time due to aging, changes in lifestyle, and medications, among other factors, it is important to measure multiple BPs to gain a more accurate estimation of an individual's BP.
As BP values in the normal and high normal range have been associated with a range of cardiovascular conditions, such as myocardial infarction and stroke, it is warranted to explore the associations between normal and high normal BP and risk of other medical conditions where BP is involved in the pathogenesis [10]. As hypertension is one of the most important risk factors for the development of AF, it is of the essence to study the association between BP below hypertensive levels and AF risk.
We used a large, prospective, population-based cohort study in which a large proportion of the participants had multiple BP measurements to investigate the association between BP and risk of incident AF. Our aim was to study the association between normal BP and high normal BP and risk of incident AF.
2 Methods
2.1 Study Cohort and Case Definition
This is a cohort study that included inhabitants of Västerbotten County in northern Sweden (population ~260,000) who participated in the health examination Västerbotten Intervention Programme (VIP) between January 1, 1988, and September 5, 2014. Time to event was defined as time from the health examination to the time of first registration of a diagnosis of AF, that is, incident AF (ICD-10 code I48 or ICD-9 code 427.3) in the Swedish National Patient Registry during the follow-up period. In a study conducted in northern Sweden, AF was identified by searching both the combined inpatient and outpatient register for ICD-10 diagnoses of AF and, in addition, an ECG database was searched for ECGs computer-interpreted as AF. All identified cases with AF were manually validated, and an ICD-10 diagnosis of AF had a positive predictive value of 96.5% [11]. Participants with an AF diagnosis before the health examination were excluded. Observations from all health examinations during the study period were included in the analysis. Covariates were updated at each health examination. Health examinations performed after the participant had been diagnosed with AF were excluded. Follow-up was defined as time from the health examination to the next health examination, to diagnosis of incident AF, moving from Västerbotten County, death, or study end on September 5, 2014, whichever came first. Individuals who did not experience an outcome incident AF event were censored at moving from Västerbotten County, death, or study end on September 5, 2014, whichever came first.
2.2 Health Examinations
All inhabitants of Västerbotten County are invited to participate in the VIP at 40, 50, and 60 years of age, and also at 30 years of age until 1995. Health examinations were performed at the participants' primary health care centers [12]. The VIP participation rate varied over time; it was 54.7% in 1990–1994, 58.3% in 1999–2002, and 62.5% in 2003–2006 [13]. There were only small differences between those who participated and those who did not participate in the VIP [13]. Study participants were invited to health examinations every 10 years. Among those eligible for two or more health examinations, 92.3% participated in two or more health examinations, see Supporting Information S1: Figure S1 for details.
The health examination included measurement of body height, weight, BP, fasting glucose, and an oral glucose tolerance test. Participants answered a questionnaire addressing, for example, education level, smoking habits, alcohol use, history of diabetes, history of myocardial infarction, medication use, and leisure-time physical activity.
2.3 Measurements and Definitions
We analyzed BP both as a continuous variable in 10 mmHg increments and as a categorical variable. Measurements of BP were made after a minimum of 5 min rest. An adequate BP cuff size was required, with the arm positioned at level with the heart. BP measurements were recommended to be performed in the right arm. BP measurements were performed in a supine position until August 31, 2009. From September 1, 2009, BP was measured in a sitting position, and the mean SBP and DBP of two BP measurements were recorded. The VIP health examination is performed by trained nurses in the primary health care in the region. Participants were categorized into one of four different categories according to ESC guidelines on arterial hypertension: optimal BP, systolic BP (SBP) < 120 mmHg and diastolic BP (DBP) < 80 mmHg; normal BP, SBP 120–129 mmHg and/or DBP 80–84 mmHg; high normal BP, SBP 130–139 mmHg and/or DBP 85–89 mmHg; or hypertension, SBP ≥ 140 mmHg or DBP ≥ 90 mmHg [14]. Participants were classified in the highest category for which they met the criteria. Antihypertensive treatment was not included in the definition of BP categories. Persons with antihypertensive treatment were also classified as having achieved BP 140/90 mmHg or more as opposed to achieved BP 139/89 mmHg or less and as having achieved BP 130/80 mmHg or more as opposed to achieved BP 129/79 mmHg or less, respectively. Height and weight were measured. Fasting plasma glucose was analyzed, and participants without diabetes and fasting plasma glucose < 7.0 mmol/L were offered an oral glucose tolerance test. Diabetes was defined as self-reported diabetes or antidiabetic treatment, fasting plasma glucose ≥ 7.0 mmol/L, or a 2-h oral glucose tolerance test plasma glucose ≥ 12.2 mmol/L in capillary samples. Additional data were collected from questionnaires. Participants were categorized as never smokers or ever smokers (including daily smokers, occasional smokers, and previous smokers). Problem drinking was defined as two or more affirmative answers to the CAGE (Cut down, Annoyed, Guilty, Eye opener) questions. Education level was categorized as higher education (more than secondary school education) or no higher education. Physical activity was categorized as regular in participants who exercised at least once a week and as not regular otherwise. Data on the history of myocardial infarction and self-reported use of antihypertensive medications during the 2 weeks preceding the health survey were collected by questionnaire.
2.4 Statistical Analysis
Means, numbers, and proportions with 95% confidence intervals (CIs) were calculated for baseline characteristics. Differences in baseline characteristics between participants with optimal BP, normal BP, high normal BP, and hypertension were determined by the χ2 test (categorical variables) and the Kruskal–Wallis test (continuous variables). We examined the prevalence of different last digit BP levels registered to explore the frequencies of different BP values in the population. Cox proportional hazards regression with time-updated variables was used to calculate hazard ratios (HRs) and 95% CIs for the association between SBP, DBP, and risk of incident AF [15]. Hence, the values of the covariates (e.g., BP, weight, height, plasma glucose, smoking status), measured at the first health examination, were updated from the time point of any subsequent health examinations, thereby including all available health examinations for each participant. If a participant only participated in one health examination, covariates were not updated, and the values of the covariates measured at the first health examination were used throughout the study. Two prespecified models were used. The first model was adjusted for age. In the second model, adjustments were made for age, sex, weight, height, antihypertensive treatment, education level, smoking habits, history of myocardial infarction, diabetes, problem drinking, and physical activity. We also prespecified analyses of the association between BP and AF risk stratified for sex and anti-hypertensive treatment, respectively. The prevalence of missing values for all variables included in these models is presented in Supporting Information S1: Table S1. Observations with missing values for a variable included in an analysis were excluded from that analysis.
To explore any relationships between SBP (90–160 mmHg), DBP (60–110 mmHg), and AF risk, Cox proportional hazards regression analyses with restricted cubic splines were performed. These analyses were adjusted as described above. Four knots (five degrees of freedom) were used. The knots were placed at the 5:th, 35:th, 65:th and 95:th percentiles of the variables as recommended by Harrell Jr. [16].
For categorical variables, the proportional hazards assumption was tested using Kaplan–Meier plots and plots of the log-minus-log of the survival function versus the survival time, with separate curves for each level of the categorical covariates. For continuous variables, Schoenfeld residuals were used. Two-sided p values < 0.05 were considered significant. Statistical analyses were performed in IBM SPSS Statistics for Macintosh, Version 27.0 (Armonk, NY, IBM Corp) and STATA version 14 (Stata Corporation, College Station, TX, USA).
3 Results
The final cohort included 109,697 participants. The participants provided 162,982 observations of exposure variables; 109,697 observations were collected at a first, 44,108 at a second, 9131 at a third, and 46 at a fourth health examination. The participants were followed for a total of 1,496,946 person-years. During the study period, 5260 persons were diagnosed with incident AF after a mean follow-up of 13.6 years (0.0–25.9 years); equivalent to an incidence of 3.5 (95% CI 3.4–3.6) cases of AF per 1000 person-years of follow-up in this middle-aged population. Among the participants, 7420 died during the study period. A graph demonstrating the observed frequencies of ending digits of SBP measurements is found in Supporting Information S1: Figure S2. During the study period, 580 persons with optimal BP, 875 persons with normal BP, 990 persons with high normal BP, and 2734 persons with hypertension were diagnosed with incident AF. The incidence of AF was 1.42 (95% CI 1.31–1.54) cases per 1000 person-years of follow-up among persons with optimal BP; 2.43 (95% CI 2.28–2.60) cases per 1000 person-years of follow-up among persons with normal BP; 3.59 (95% CI 3.37–3.82) cases per 1000 person-years of follow-up among persons with high normal BP, and 6.26 (95% CI 6.03–6.50) cases per 1000 person-years of follow-up among persons with hypertension. The mean participant age at the health examination was 48.7 years. More than one-fourth of the observations were hypertensive, and half of the observations were ever smokers. Characteristics of the study cohort are provided in Table 1. In persons with elevated BP, a number of cardiovascular risk factors, such as higher age, male sex, and diabetes, were more common than in normotensive persons (Supporting Information S1: Table S2).
| Observations, n = 162,982 | |
|---|---|
| Age, years | 48.7 (9.2) |
| Male | 79,075 (48.5%) |
| Height, cm | 171.4 (9.3) |
| Weight, kg | 76.9 (15.1) |
| Systolic blood pressure | 126.6 (17.3) |
| Diastolic blood pressure | 79.0 (10.8) |
| Antihypertensive treatment | 20,506 (12.6%) |
| Problem drinking | 10,506 (6.7%) |
| History of myocardial infarction | 1820 (1.2%) |
| Diabetes mellitus | 7633 (4.7%) |
| Ever smoker | 81,036 (50.0%) |
| Leisure-time physical activity at least once weekly | 55,849 (36.1%) |
| No higher education | 115,466 (71.9%) |
- Notes: Values are shown as mean (standard deviation) or number (%). Problem drinking, ≥ 2 points on the CAGE (Cut down, Annoyed, Guilty, Eye opener) scale.
As continuous variables, SBP and DBP were independently associated with increased risk of incident AF (Table 2). The restricted cubic splines analysis showed a gradual increase in AF risk with increasing SBP and DBP (Supporting Information S1: Figure S3).
| Incident AFa/number of observations | Model adjusted for age | Multivariable modelb | |
|---|---|---|---|
| Systolic BP, in 10 mmHg increments | 5173/161,458 | 1.15 (1.13–1.16) | 1.11 (1.10–1.13) |
| Diastolic BP, in 10 mmHg increments | 5172/161,383 | 1.25 (1.22–1.28) | 1.13 (1.09–1.16) |
| Optimal BP | 580/46,577 | 1 (ref.) | 1 (ref.) |
| Normal BP | 874/39,770 | 1.29 (1.16–1.44) | 1.13 (1.01–1.27) |
| High normal BP | 989/30,572 | 1.50 (1.36–1.67) | 1.23 (1.10–1.38) |
| Hypertension | 2730/44,477 | 2.02 (1.84–2.22) | 1.55 (1.39–1.71) |
- Notes: Associations are shown as hazard ratios with 95% confidence intervals.
- Optimal BP: systolic blood pressure < 120 mmHg and diastolic blood pressure < 80 mmHg. Normal BP: systolic blood pressure 120–129 mmHg or diastolic blood pressure 80–84 mmHg. High normal BP: systolic blood pressure 130–139 mmHg or diastolic blood pressure 85–89 mmHg. Hypertension: systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg.
- Abbreviations: AF, atrial fibrillation; BP, blood pressure.
- a Number of individuals with incident AF during follow-up (each individual is counted only once).
- b Model adjusted for age, sex, weight, height, problem drinking, antihypertensive medication, history of myocardial infarction, diabetes, smoking, education level, and physical activity.
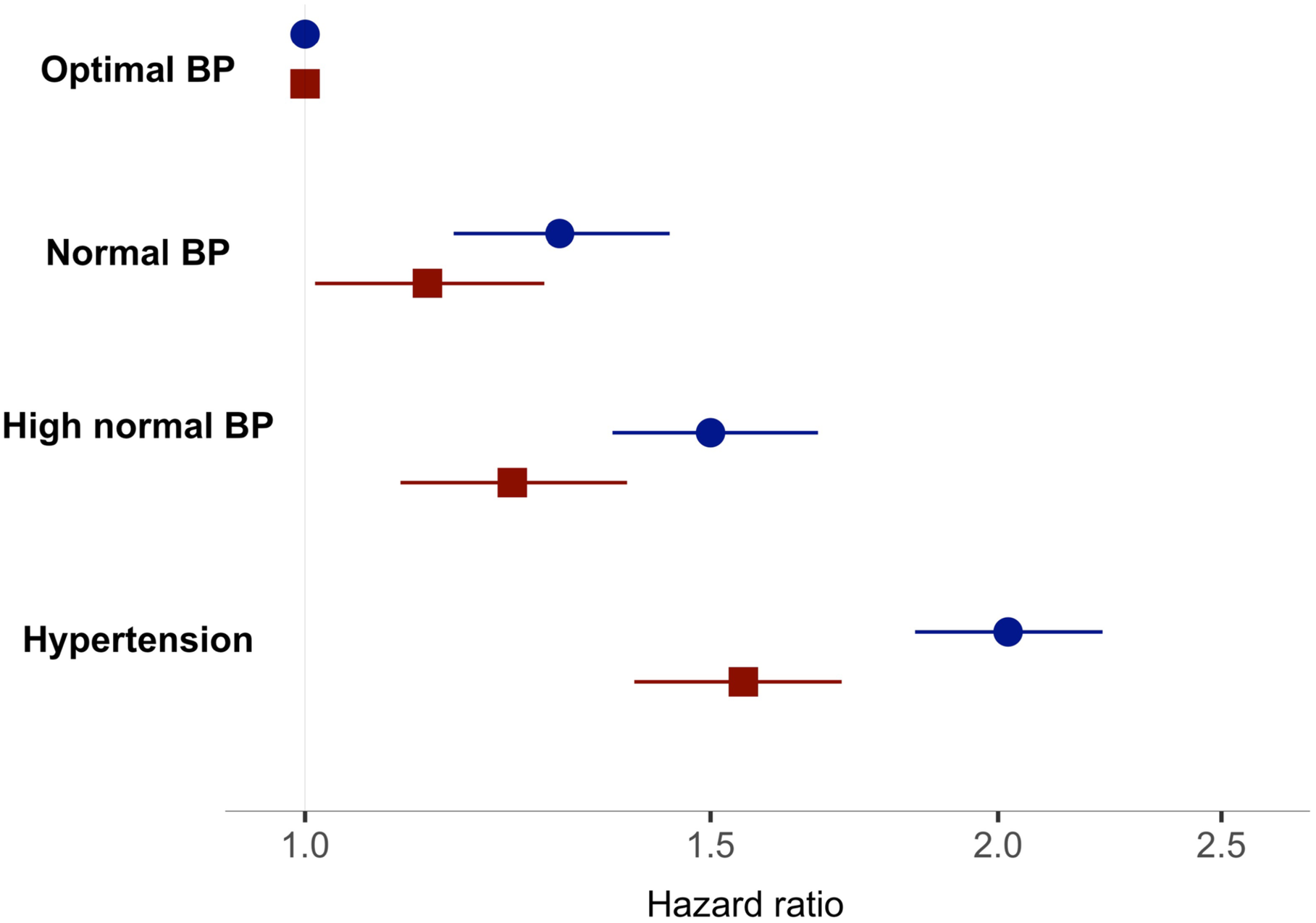
When analyzing BP in categories, normal BP, high normal BP, and hypertensive BP were independently associated with an increased risk of incident AF compared to optimal BP (Table 2 and Figure 1). In a sex-stratified analysis, HRs for the association between normal BP and AF risk were similar to those in the main analysis, though no longer significant (HR 1.08 [95% CI 0.90–1.30] for women and HR 1.11 [95% CI 0.96–1.29] for men in a fully adjusted model). Regarding high normal BP and AF risk, we found HRs similar to those in the main analysis; (HR 1.27 [95% CI 1.06–1.53] for women and HR 1.16 [95% CI 1.01–1.34] for men). We found independent associations between normal BP and risk of incident AF (HR 1.16 [95% CI 1.03–1.30]), high normal BP and risk of incident AF (HR 1.29 [95% CI 1.14–1.45]), and hypertensive BP and risk of incident AF (HR 1.53 [95% CI 1.37–1.72]) in participants not treated with anti-hypertensives. No significant associations were found in participants treated with anti-hypertensives neither with normal BP (HR 0.80 [95% CI 0.56–1.13]), with high normal BP (HR 0.82 [95% CI 0.59–1.14]), nor with hypertensive BP (HR 1.20 [95% CI 0,89–1.62]), and AF risk (Supporting Information S1: Table S3 and Figure S4).
In persons treated with antihypertensive treatment, we found an independent association between achieved BP 140/90 mmHg or more (HR 1.44 [95% CI 1.25–1.66]) compared to lower BP and an increased risk of AF, and we found no significant association between achieved BP 130/80 mmHg or more (HR 1.24 [95% CI 0.98–1.57]) and AF risk.
Together with normal BP, high normal BP, and hypertension, a number of cardiovascular risk factors (age, male sex, height, weight, anti-hypertensive medication, history of myocardial infarction, problem drinking, smoking, and low education level) were independently associated with AF risk (Supporting Information S1: Table S4).
4 Discussion
We found a statistically significant, independent association between normal BP (HR 1.13), high normal BP (HR 1.23), and increased risk of incident AF. The AF risk gradually increased with increased levels of both SBP and DBP.
4.1 Normal BP, High Normal BP, and Risk of Incident AF
An association between normal and high normal BP, with approximately the same definitions as those used in our study, and risk of incident AF similar to that found in our study was reported in a Korean study, a Norwegian study of men, and in the American Women's Health Initiative study of women [5-7]. In contrast to the results of our study, the Framingham study reported no significant association between normal BP and high normal BP combined and AF risk [8]. The Framingham study included fewer participants compared to our study; the fact that they did not find a significant association between normal BP and high normal BP combined and risk of AF may be due to insufficient statistical power. Furthermore, the participants in the Framingham study were, in general, older than those in our study, which may be one explanation for the difference in results between our studies, as there is some evidence that the association between BP and AF risk may be less apparent in individuals aged > 60 years [8].
We also saw a gradual increase in the risk of incident AF with increasing BP with no apparent lower cutoff. Similarly, the AF risk increased gradually with increasing SBP in a European study of population-based cohorts with a similar age and sex distribution as in our study [17]. An association between both SBP and DBP and an increased AF risk was reported in a recent meta-analysis of cohort studies [2].
In our study, a large proportion of study participants had undergone at least two health examinations, and BP values were updated at each health examination. Although time-updated BP values were used in the present study, we did not investigate the association between changes in BP over time and risk of AF. In a study by Rahman et al., longitudinal patterns of SBP, termed trajectories, were associated with AF risk. Participants with initial hypertensive SBP values were at increased risk of AF, regardless of subsequently increasing or decreasing SBP, compared to those who were normotensive throughout the study. Those who were prehypertensive were not at increased risk of AF [18].
In our study, 12.6% of the observations were treated with antihypertensive medications. Though we found an association between normal BP and high normal BP and AF risk in persons not treated with antihypertensive medication, we could not detect an association between normal BP or high normal BP and AF risk in persons treated with antihypertensive medication. Hypothetically, the lack of association between normal BP and high normal BP and AF risk in persons treated with antihypertensive medication may be due to insufficient power in this group. Alternatively, this could be due to the presence of an unmeasured confounder, such as heart failure or a socioeconomic difference between those who were treated and those who were not treated with antihypertensives. From other studies, we know that a target SBP of < 120 mmHg compared to < 140 mmHg in persons with hypertension at increased risk of cardiovascular disease is associated with a lower risk of developing incident AF [19]. In primary health care, individuals with hypertension with SBP ≥ 140 mmHg have a higher AF risk compared to individuals with a lower achieved SBP, but there is no difference in risk of incident AF when comparing individuals with achieved SBP 130–139 and < 130 mmHg [20]. Furthermore, we saw an association between treatment with antihypertensive medication and a higher risk of incident AF (shown in Supporting Information S1: Table S4). This may possibly be a marker of a longer duration of exposure to high BP. We consider it unlikely that this association is due to adverse effects of the antihypertensive medication.
Our observational study design does not allow conclusions about causality and our findings need to be verified in further studies, preferably randomized controlled intervention studies where participants are randomized to BP lowering treatment aiming at an optimal BP as opposed to conventional target BPs. If such a study could prove a benefit in the form of lower risk of AF in patients reaching an optimal BP without unacceptable risks or negative side effects, this could change clinical practice. More intensive BP monitoring and intervention strategies targeted at individuals with nonoptimal BP could be implemented. Strict BP control could also have other benefits, as shown by the SPRINT study, where aiming for a target SBP of < 120 mmHg, as opposed to < 140 mmHg, leads to a lower risk of cardiovascular events and death from any cause [21]. However, it is important not to overshoot the target as orthostatic hypotension, common in patients with antihypertensive treatment, has been linked to increased all-cause mortality [22].
4.2 Possible Pathophysiological Mechanisms
The mechanism explaining the association between BP and the risk of incident AF has not been fully elucidated, but several possible mechanisms have been suggested. Hypertension can contribute to atherosclerosis, which can cause myocardial infarction. History of myocardial infarction is a known risk factor for AF [23]. Hypertension can cause left ventricular hypertrophy. This can lead to increased diastolic filling pressure due to impaired diastolic function of the left ventricle. The increased diastolic filling pressure leads to an increased volume of the left atrium, which is associated with incident AF [24]. Hypertension is closely linked to arterial stiffness [25]. It has been shown that in turn, a higher degree of arterial stiffness is associated with a larger left atrial diameter [26]—which in itself could predispose to AF development [27]. In patients with hypertension, P-wave peak time and P-wave dispersion may be useful to assess the risk of incident AF [28]. Conceivably, these measures reflect left atrial parameters.
Increased activity in both the sympathetic nervous system and the renin-angiotensin-aldosterone system are other possible mechanisms explaining the association between an increased BP and AF risk [24, 29]. There may be differences between individuals in the association between elevated BP and risk of AF, and also in the relative importance of the different factors contributing to AF development [30]. Left ventricular filling pressure can be assessed by left atrial strain, and a lower left atrial reservoir strain has been associated with incident AF [31]. Factors such as high BP can give rise to an atrial substrate for AF due to, for example, fibrosis and dilation [32]. AF can then be triggered by electrical discontinuation in the myocardium due to, for example, cardiac ischemia or anatomical factors. Examples of anatomical factors are the properties of the endothelium and the myocytes of the pulmonary veins. The atrial substrate for AF can then perpetuate the arrythmia [32].
4.3 Strengths and Limitations
The large cohort size, the long follow-up period and the use of time-updated covariates are key strong points of the present study. Together, these factors increase the reliability of our findings and lower the risk of type 2 errors. We were also able to perform stratified analyses with acceptable statistical power. Our population-based study design increases study generalizability. All middle-aged individuals residing in the area were invited to the health examinations, which had a participation rate of 54.7% in 1990 and 62.5% in 2006 [13]. The individuals who participated are representative of the total population in the study area [12]. However, the population-based design introduces an element of heterogeneity, which can limit the generalizability of the study results to specific patient groups. Our method of ascertaining AF diagnoses was previously validated, and a diagnosis of AF in the Swedish National Patient Registry has a positive predictive value of 96.5% [11]. All data were collected before the AF event, which eliminates the risk of recall bias. As this is an observational study, no causal relationships can be established. Our analyses were adjusted for cardiovascular risk factors. As the studied cardiovascular risk factors differed between individuals with optimal BP, normal BP, high normal BP, and hypertension (Supporting Information S1: Table S2), it is essential to take these into account when analyzing the association between BP and AF risk. Furthermore, all adjustment variables, except physical activity and diabetes, were associated with AF risk in our study population in a fully adjusted model (Supporting Information S1: Table S4). However, there is a remaining risk of residual confounding in our study, since we did not include conditions such as valvular heart disease and sleep apnea syndromes in our multivariable analyses. A limitation of our study was that no ECG screening was performed. As such, there is a risk that asymptomatic AF was overlooked. If it did not result in, for example, an irregular pulse noted at a health examination or if it was not otherwise detected within routine healthcare. Thus, the generalizability of our results to persons with undetected asymptomatic AF is uncertain.
Our study cohort consisted of middle-aged individuals followed for a median of 11.3 years, and the median age at the end of follow-up was 60 years and the results of our study may not be generalizable to other age groups. Most likely, the lower incidence of AF seen in our study is related to the fact that the participants of our study were, on average, younger than those of other studies of AF incidence [1, 33]. A substantial proportion of our large study population had participated in repeat health examinations, enabling us to analyze the association between BP and AF risk with time-updated variables. A limitation of our study is the 10-year interval between health examinations. This means that the BPs recorded at the health examinations may inadequately reflect the BP of the participants over time. More frequent BP measurements would have been valuable.
The method of measuring BP matters when assessing AF risk. In a study of patients with treated hypertension, clinic, daytime, nighttime, and 24-h SBP were significantly associated with an increased risk of incident AF, but when adjusting this analysis for various covariates, clinic SBP was no longer associated with increased risk of incident AF, whereas the ambulatory BP measurements were still associated with incident AF [34]. Furthermore, an association between daytime, nighttime, and 24-h SBP and AF risk, but no significant association between clinic SBP and AF risk in adjusted models, was found in a European cohort study [35]. It would have been preferable if our study had included ambulatory BP measurements as well as the BP measurements made at the primary health care centers.
5 Conclusion
There is an increased risk of AF in middle-aged individuals with normal BP and high normal BP compared to those with optimal BP. This emphasizes the importance of the association between BP and AF risk.
Author Contributions
Cecilia Johansson: conceptualization, data curation, formal analysis, funding acquisition, project administration, visualization, and writing – original draft. Lars Johansson: conceptualization, formal analysis, funding acquisition, project administration, supervision, writing – review and editing. Marie Eriksson: formal analysis, project administration, supervision, writing – review and editing. Jonas Andersson: formal analysis, project administration, supervision, writing – review and editing. Marcus M Lind: conceptualization, formal analysis, project administration, resources, supervision, writing – review and editing.
Acknowledgments
We acknowledge the Västerbotten Intervention Programme, Västerbotten County Council, the Foundation for Medical Research in Skellefteå and the Heart Foundation of Northern Sweden. C.J. received grants for this study from Västerbotten County Council, the Foundation for Medical Research in Skellefteå and the Heart Foundation of Northern Sweden. Västerbotten County Council participated in the collection of data. The funding sources had no other role in study design, analysis, and interpretation of data, in the writing of the article, or in the decision to submit the article for publication.
Ethics Statement
The study was approved by the Regional Ethics Review Board, Umeå, Sweden (approval number 2015–50–31 M).
Consent
All participants provided informed consent.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The lead author, Marcus M. Lind, affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
Data Availability Statement
The data analyzed in the study consists of third-party health data from VIP and their use has been approved by the Regional Ethics Review Board, Umeå, Sweden (approval number 2015–50–31 M). According to Swedish legislation, data cannot be made available for use beyond what has been approved by the ethical review board. Therefore, the data cannot be made publicly available. Data may be made available from the Biobank Research Unit, Umeå University, upon reasonable request by researchers who meet the criteria for access to confidential data according to Swedish laws and regulations.




