Epidemiology of Myopia Occurrence, Development, and Correction in Primary School Students in China: A Retrospective Cohort Study
Lin-ya Qiu and Ya-juan Pu contributed equally to this study.
ABSTRACT
Background
The purpose of this study is to assess the occurrence, progression, and correction of myopia in primary school students in China over the past few years.
Methods
This longitudinal cohort study was based on a 5-year follow-up sample of first-year students enrolled in 2019. Data were collected from students' regular physical examinations conducted between September and December every year.
Results
A total of 6790 primary students were included in this analysis, of whom 3658 (53.8%) were boys. The spherical equivalent of students' binocular vision demonstrated a marked annual decline. The myopia rate gradually escalated from 23.4% in Grade 1 to 80.1% in Grade 5. The largest increase, amounting to 30%, occurred during the grade 1–2. A negative correlation was found between the spherical equivalent values and students' height, particularly among girls in grades 4 and 5. In grades 4 and 5, the rate of myopia among girls was approximately 5% higher than that among boys. Among students with moderate to severe myopia, the rate of spectacle wear for vision correction were 21.9%, 47.9%, 58.0%, 67.1%, and 71.5% in grades 1–5, respectively. Among students with spectacle wear, the rate of those with qualified vision correction reaching about 85%.
Conclusions
Over 5 years from 2019 to 2023, the myopia rate among observed primary school students, particularly moderate and severe cases, has been alarmingly high, with inadequate vision correction. Additionally, myopia rates differ among students of various genders and heights.
1 Background
Myopia has become a preeminent ocular problem and evolved into a pressing health concern. High-degree myopia is one of the leading causes of visual impairment and blindness globally [1, 2]. Over the past few decades, the prevalence of myopia has witnessed a dramatic increase, rendering it a crucial global public health issue [3, 4]. Childhood myopia is associated with a longer course of disease, faster progression of myopia, and a higher risk of developing severe myopia and myopic macular degeneration [5]. A study on children with high-degree myopia in China found that approximately 20% progress to myopic macular degeneration [6], which is in a concerning condition. Myopia can also affect a child's growth and development, academic skills, and mental health. Studies have shown that myopia leads to reduced control of moving objects, affects fine and gross motor skills, puts pressure on the entire musculoskeletal system, and hinders normal growth and development in children [7]. Given the prominent role of vision in perceiving and understanding the environment, impairment of this sensory modality may adversely affect psychological well-being, leading to anxiety, depression, or self-esteem issues [8, 9].
The overall myopia prevalence in children and adolescents in China was 36.6% in 2020 [10]. In response to the COVID-19 pandemic, China implemented outbreak prevention and control measures such as school closures and online teaching during 2020 and 2022. Measures implemented in response to COVID-19 may potentially impact the visual development of students [11]. The precise onset and extent of these impacts are yet to be investigated. Spectacle wear is the most important means of correcting vision. Whether students with moderate to severe myopia can receive timely vision correction remains to be further explored. Most of the previous studies on myopia in Chinese children were cross-sectional design, this design has limitations when exploring factors that change over time, such as height and weight. This study adopts a cohort design, aiming to understand the epidemiological characteristics of the occurrence, development and correction of myopia among Chinese primary school students who have experienced the COVID-19 pandemic. It also endeavors to explore the differences in myopia occurrence among students of different genders and those at varying stages of height–weight development.
2 Objects and Methods
2.1 Study Design and Population Selection
Students who received consecutive 5-year visual acuity and growth assessments were selected from the first-grade freshmen of 44 primary schools in Suzhou who enrolled in 2019 to form a retrospective cohort. Students with missing data in terms of age, gender, or any of the assessments were excluded. The guardians of the participants have all signed informed consent forms. All processes in this study followed the Declaration of Helsinki and its later updated versions. This study obtained ethical approval from Gusu District Center for Disease Control and Prevention and complies with the ethical management regulations of the institution and the country.
2.2 Assessment and Quality Control
Testing and assessment were carried out from September to December each year from 2019 to 2023 at participants' schools. Height and weight were measured using electronically calibrated equipment that has achieved metrological certification. Ocular refractive parameters such as spherical equivalent (SE) were detected by an automatic refractor (Topcon, RM-800) in accordance with the instrument's operating specifications. Visual acuity is assessed using the 5-point recording method. The 5-point recording method is a logarithmic-value approach, which describes visual acuity by subtracting the logarithm of the visual angle from 5. The formula for calculation is L = 5−LogMAR. A score of 5 indicates normal visual acuity, while a score of 0 represents no light perception. During the assessment, under specified lighting conditions, the subject covers one eye and varies the distance by taking steps to identify the “E” characters of different sizes on the standard visual acuity chart, thereby obtaining the corresponding visual-acuity parameters [12, 13].
The assessment team, composed of pediatricians and ophthalmologists from the Children's Hospital who have undergone standardized training, conducts annual preservice training. Health professionals and technicians from the hospital's Quality Control team and the Center for Disease Control and Prevention are responsible for on-site quality assurance of measurements, ensuring compliance with examination protocols.
2.3 Definition and Group
An SE less than −0.5D was defined as myopia, which was classified as follows: mild myopia, with −3.0 D < SE < −0.5 D; moderate myopia, with −6.0 D ≤ SE ≤ −3.0 D; and severe myopia, with SE < −6.0 D. The qualified visual acuity correction was defined as that the visual acuity of students suffering from myopia was not lower than 4.8 (5-point recording method) after wearing spectacles.
Using the age-specific parameters of the overall Chinese adolescents as the evaluation system, the heights and Body Mass Index (BMI) of the participants were classified. In accordance with China's “WS/T 423-2022” and “WS/T 612-2018”, the participants' heights were divided into four grades: low level, mid, high, and top. Based on China's “WS/T 423-2022” and “GB/T 31178-2014”, the participants' BMIs were classified as emaciation, normal, overweight, and obesity.
2.4 Statistics and Analysis
SAS 9.4 was used for statistical analysis. Count data were expressed as percentages (%). The repeated-measures analysis of variance was used to compare the SE at different time points. A trend χ2 test was used for rate changes. The rates of spectacle wear between genders were compared using logistic regression to correct for myopia severity. Two-sided tests were used for all comparisons, with p < 0.05 indicating statistical significance.
3 Results
A total of 6790 students were included in this analysis, with 3658 (53.8%) being boys. The mean age at the first visual acuity test was 6.78 ± 0.31 years. The median SE of the right eye decreased from 0.25 D (IQR, 0.00~0.75) in Grade 1 to −1.25 D (IQR, −2.50~−0.25) in Grade 5 (p < 0.001, Figure 1A,C), and that of the left eye decreased from 0.25 D (IQR, 0.00~0.75) in Grade 1 to −1.00 D (IQR, −2.50~−0.25) in Grade 5 (p < 0.001, Figure 1B,D). The myopia rate of either eye was 23.4% in grade 1, with the largest increase (30.2%) occurring in Grade 2, when myopia reached 53.6%, subsequently increasing at a rate of about 10% per year (p < 0.001). By Grade 5, myopia rate reached 80.1%, with moderate to severe myopia rate reaching 23.7% (Figure 2A).


There was no significant difference in myopia prevalence between boys and girls in grades 1, 2 and 3. However, by grades 4 and 5, the myopia rate among girls was approximately 5% higher than that among boys, mainly due to a higher percentage of mild myopia (p < 0.05, Figure 2A). There was no statistically significant difference in myopia prevalence among students of different weight levels (p > 0.05, Figure 2B).
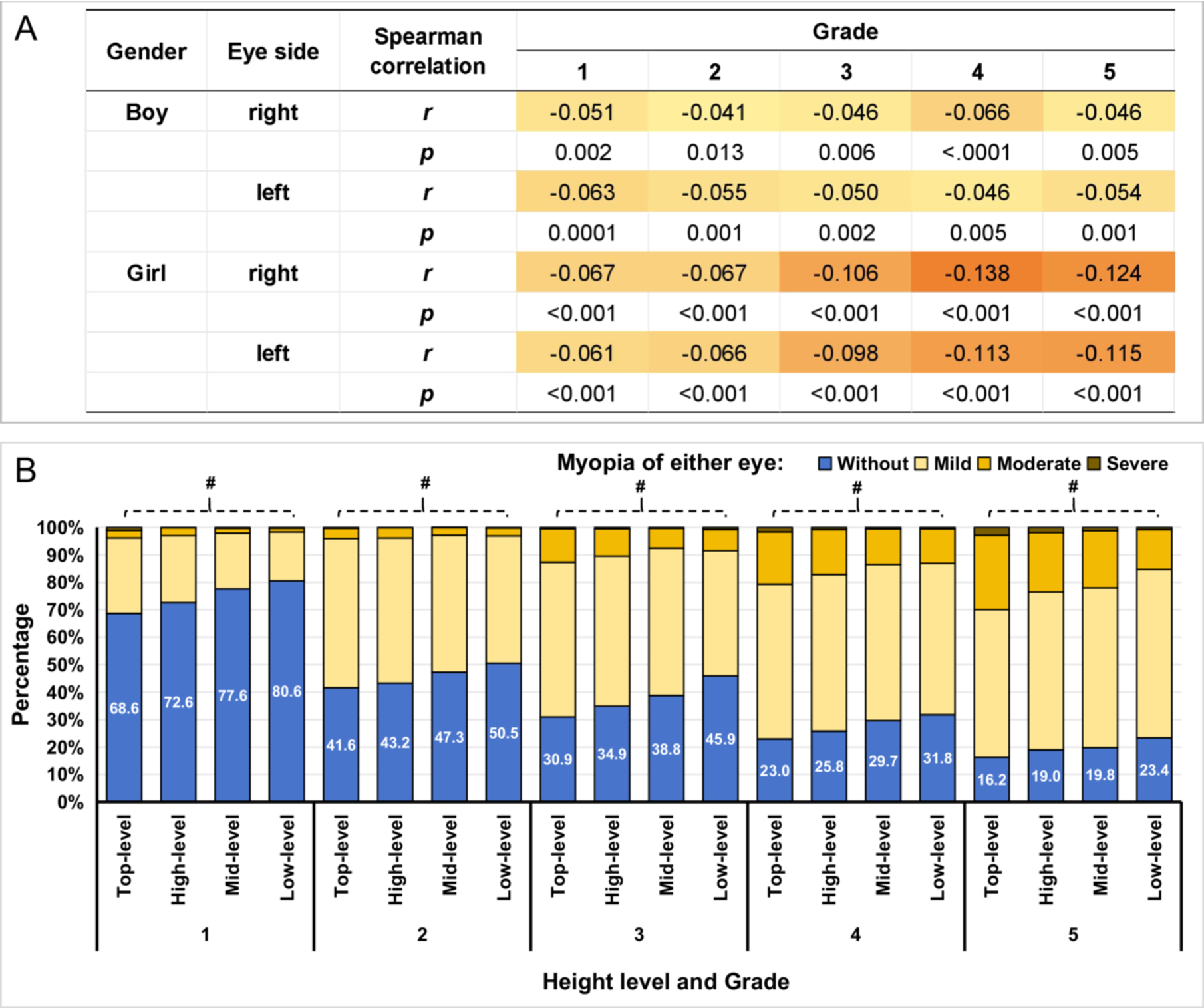
There was a negative statistical low correlation between students' height values and SE. Especially among girls, this negative low correlation became stronger as the grade increased (p < 0.05, Figure 3A). After classifying height into grades, students with higher height grades had a higher myopia rate and more severe myopia (p < 0.05, Figure 3B).
Among students with moderate to severe myopia, despite a notable increase in the rate of spectacle wear for vision correction, this proportion remained relatively low. Specifically, the rates were 21.9%, 47.9%, 58.0%, 67.1%, and 71.5% in Grades 1–5, respectively (Trend test p < 0.001, Figure 4A). For students with mild myopia, the rate of spectacle wear for vision correction rose from 5.5% in Grade 1 to 17.3% in Grade 5 (Trend test p < 0.001, Figure 4A). After adjusting for myopia severity, there was no statistically significant difference in spectacle wear between boys and girls (p > 0.05).
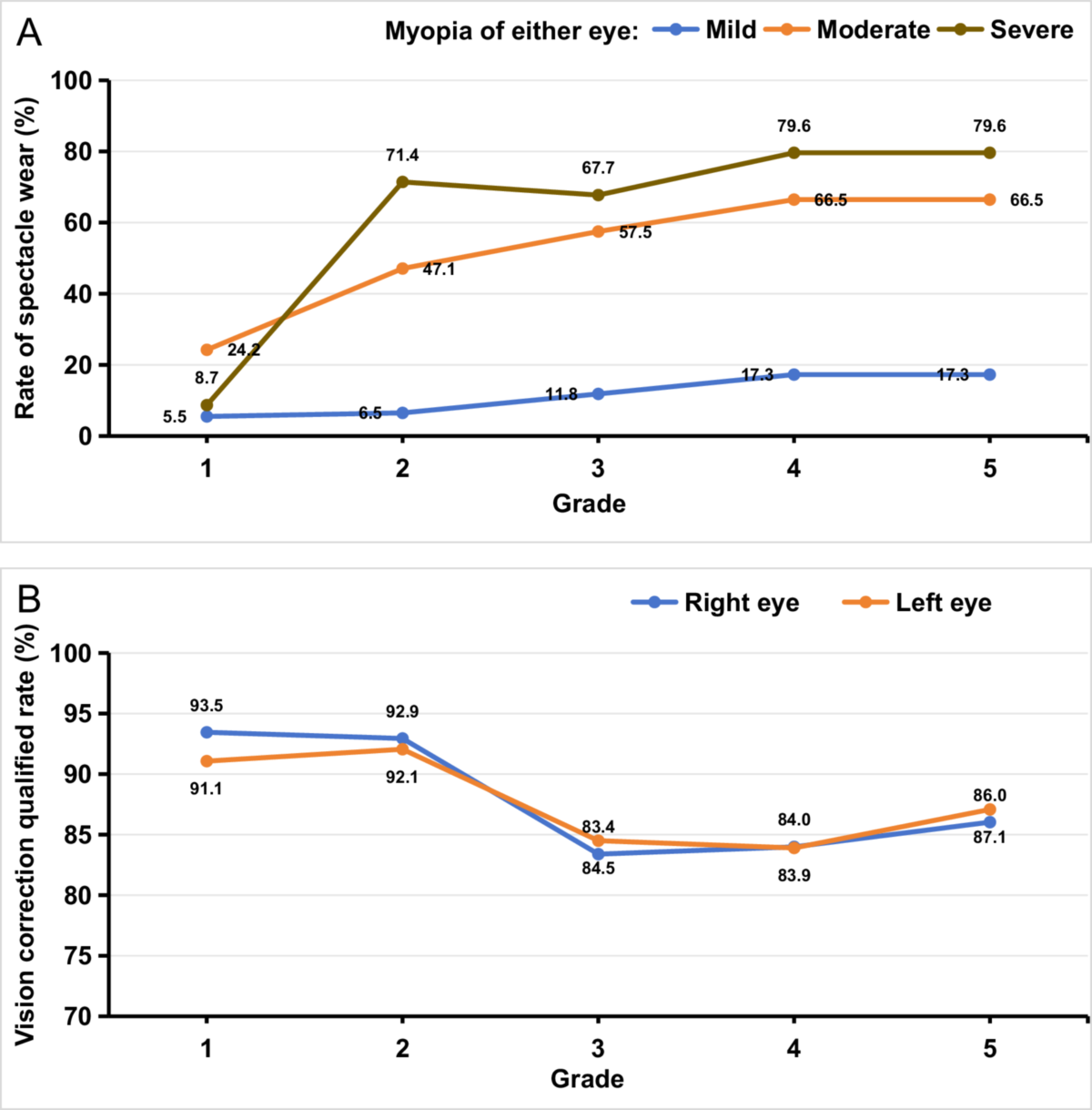
Among students with spectacle wear for vision correction, the rate of those with qualified vision correction exceeded 90% in grades 1 and 2. However, in the grades 3, 4, and 5, the qualified rate of vision correction was lower, approximately 85% (p < 0.05, Figure 4B).
4 Discussion
This cohort study found that the prevalence of myopia among first-grade primary school students was already significant. After 5 years of study, these students have a very high myopia rate, especially the rate of moderate to severe myopia. This situation is quite worrying. This indicates that myopia screening and intervention should be conducted at an earlier age, and the effectiveness of current intervention strategies should be improved. When compared with the myopia rates of primary school children in China a decade ago, as well as those in Europe and Australia [6, 14], the myopia rates in both first-grade and senior-grade students in the present study were significantly higher. In recent years, the academic pressure on Chinese primary school students has been increasing [15]. Poor eye-use habits caused by students' academic pressure are one of the main reasons for the high myopia incidence rates. Studies on myopia development have found that competitive pressures and educational expectations lead children to spend more time engaged in near visual activities [16]. The visual fatigue caused by long hours of study, both in school and during extracurricular periods, along with a lack of sufficient outdoor activities at long visual distances, are the main causes of myopia development. Additionally, the widespread use of electronic devices and urban night light exposure has significantly contributed to the increase in the incidence of myopia in children at a younger age [17].
Previous studies have observed that the most significant increase in myopia incidence among primary students typically occurs between grades 2 and 4 [6, 18]. In contrast, this study identified the most significant increase during the transition from grade 1 to grade 2 (corresponding to vision screening periods from September 2019 to December 2019 and September 2020 to December 2020). Due to the COVID-19 outbreak, the students in this study engaged in online video-based learning from February 2020 to September 2020. Despite regulatory controls over individual video lecture durations, prolonged cumulative exposure to screen-based educational content still demonstrated substantial risks to ocular health. Therefore, it is reasonable to infer that long-term video-based learning is one of the reasons for the sharp increase in myopia rate among grade 1 and grade 2 students. This highlights the importance of implementing preventive strategies against secondary harms arising from public health interventions when addressing emerging infectious disease outbreaks.
In a nationwide cross-sectional study of China, no association was found between myopia prevalence and overweight and obesity in boy subjects aged 6–17 years and in girl subjects aged 11–17 years [19]. In this study, no difference in myopia rate was observed among students of different weight levels. However, it was noted that among senior grade students, the myopia rate was higher in girls than in boys. This difference may be attributed to several factors: first, girls spend more time engaging in close visual activities, such as reading and writing, and participating more in indoor activities and tutorials, with less outdoor activity [20, 21]. Secondly, in the senior grades, the differences in growth and development between boys and girls become more pronounced. Physiological factors dictate that girls reach puberty earlier than boys, and the associated growth spurt and hormonal changes during puberty may affect eye growth, thereby influencing myopia development. Research suggests that changes in hormone levels during puberty may be associated with an increase in eye axis length [22, 23]. Specifically, children with a rapid axial length growth trajectory experienced a more rapid decline in uncorrected visual acuity [24]. Further analysis also revealed that there is a negative low correlation between height and SE in this study, especially a stronger negative correlation among senior-grade girls.
The proportion of moderate to severe myopia students who wear glasses to correct vision is not high, especially in the lower grade students, this situation is surprising and worrying. This may be related to insufficient frequency of myopia screening and a lack of awareness of the role of wearing spectacles. The necessity of using spectacles for correcting low myopia remains controversial. The main points of contention include whether wearing glasses inhibits the eye's natural adjustment, whether it effectively prevents the progression of myopia, and balancing the immediate and long-term impacts on the quality of life of children and adolescents [25-27]. Regardless, timely screening and detection, followed by the implementation of effective measures to prevent myopia progression, are crucial. Given the accessibility of myopia screening technology and equipment, it is necessary to establish and improve the mechanisms for high-frequency screening of students by school health professionals.
When interpreting the results of this study, several limitations should also be noted: Firstly, being a retrospective study, it is prone to potential information bias. Secondly, the study failed to conduct an investigation into each student's eye-using habits and the influence of genetic factors on myopia. Thirdly, it should be noted that the sample of this study was restricted to data from developed cities in eastern China. Finally, due to the methodology used and the definition of myopia, there may be a potential overestimation of the myopia rate.
In summary, over 5 years from 2019 to 2023, the myopia rate among primary school students, particularly moderate and severe cases, has been alarmingly high, with inadequate vision correction. Additionally, myopia rates differ among students of various genders and heights.
Author Contributions
Lin-ya Qiu: conceptualization, data curation, methodology, formal analysis, software, writing – original draft, writing – review and editing. Ya-juan Pu: data curation, writing – original draft, writing – review and editing, resources. Xin-peng Yang: data curation and investigation. Wei-hua Zhou: supervision. Xiao-xue Yu: methodology and formal analysis. Jun-peng Jiang: resources. Yan Wang: supervision. Hua-qing Liu: conceptualization, data curation, methodology, software, supervision, writing – review and editing, validation.
Acknowledgments
The authors have nothing to report.
Ethics Statement
All processes in this study followed the Declaration of Helsinki and its later updated versions. This study obtained ethical approval from Gusu District Center for Disease Control and Prevention and complies with the ethical management regulations of the institution and the country.
Consent
The participants' guardians have all signed informed consent forms.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The lead authors, Lin-ya Qiu and Ya-juan Pu, affirm that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
Data Availability Statement
The data used in this study can be obtained upon authorization from the corresponding author.




