Knowledge, Attitude, Practice, and Determinants of Community Health Workers' Involvement Toward NCD Prevention and Control in Northern Tanzania: A Cross-Sectional Study
ABSTRACT
Background and Aim
Globally, non-communicable diseases (NCDs) are the leading cause of preventable morbidity and premature mortality. In sub-Saharan Africa, NCDs will be the leading cause of mortality by 2030. In 2018, WHO reported that NCDs accounted for about 33% of all deaths in Tanzania. Community health workers (CHWs) are among the key stakeholders in prevention and control of NCDs. In developing countries like Tanzania, CHWs play an extensive role in prevention and control of communicable diseases, however, their simultaneous involvement toward NCDs is limited. This study aimed to determine knowledge, attitude, practice, and determinants toward CHWs' involvement in NCDs prevention and control in northern Tanzania.
Methods
This was a community-based analytical cross-sectional study in northern Tanzania enrolling 191 CHWs. Frequencies and percentages, χ2, and logistic regression tests were used to summarize categorical variables and determinants of CHWs' involvement toward NCDs prevention and control, respectively, using SPSS.
Results
Majority of participants had good knowledge (92.1%) and favorable attitude (100%). More than half (63.4%) were involved in NCD prevention and control programs of which only 26.7% and 41.4% reported to have involved in NCDs screening and community mobilization programs, respectively. Only 36.1% and 46.1% reported to have access to NCDs screening tools and to have ever attended either formal NCD seminar or training, respectively. Professional training to practice as CHW, frequency of home visits per week, involvement confidence, attendance of formal seminar or training on NCDs, and accessibility of tools for NCDs screening were determinants of CHWs' involvement in NCDs prevention and control.
Conclusion
Despite the vital role of CHWs toward NCDs prevention and control, their engagement in NCDs screening and community mobilization is still low in northern Tanzania. Professional training among in-service and newly enrolled CHWs, encouragement of weekly home visits, and NCDs' capacity-building programs in terms of skills and accessibility of screening tools should be implemented among CHWs to enhance their involvement in NCDs prevention and control.
Abbreviations
-
- CHWs
-
- community health workers
-
- CVD
-
- cardiovascular disease
-
- HIV
-
- human immunodeficiency virus
-
- LMICs
-
- low- and middle-income countries
-
- NCDs
-
- non-communicable diseases
-
- TB
-
- tuberculosis
-
- WHO
-
- World Health Organization
Definition of Key Terms
Community health workers: These are paraprofessionals or lay individuals with an in-depth understanding of the community culture and language, have received standardized job-related training of a shorter duration than health professionals, and their primary goal is to provide culturally appropriate health services to the community [1].
Non-communicable diseases: These are chronic health conditions that are not contagious to others. They include cancer, diabetes, cardiovascular diseases, and chronic lung illnesses among others [2].
NCDs prevention and control practice: This refers to the involvement in activities which aim to prevent or control different non-communicable diseases in the community. It includes either screening, health promotion programs like community education, patient referral, or patient management and monitoring (operational definition).
Premature death: This refers to the death that occurs before the average age of death in a certain population [3].
1 Introduction
The rising burden of non-communicable diseases (NCDs) and associated mortality is of public health concern, especially in low- and middle-income countries (LMICs) [4, 5]. Globally, NCDs are the leading cause of premature mortality and morbidity, even though they can be significantly prevented [6]. The World Health Organization (WHO) outlined four major NCDs as the leading causes of mortality: cardiovascular diseases (CVD), diabetes mellitus, chronic respiratory diseases, and cancers [5]. These four diseases have four potential modifiable risk factors, namely, unhealthy diet, physical inactivity, harmful alcohol use, and tobacco use, that contribute to over 80% of NCDs' premature mortality [5, 6]. Globally, about 70% of all deaths are due to NCDs, and among them, 87% occur in LMICs [7]. By reducing or eliminating the four modifiable shared risk factors, up to 80% of CVD, type 2 diabetes mellitus, and over one-third of cancers can be prevented [8]. Almost 36 million people die every year (63% of the global deaths) because of NCDs: of these, 14 million deaths are premature. LMICs contribute up to 86% of the global NCDs' premature deaths [6].
In sub-Saharan Africa, NCDs will be the leading cause of mortality by the year 2030 [9]. In Tanzania, all NCDs caused about 31% of premature deaths in the year 2012: the four main NCDs caused 16% of the deaths [10]. The cases of NCDs in Tanzania have been increasing abruptly to the extent of needing an immediate action [11]. According to the WHO, NCDs countries' profiles report of 2018, it was estimated that NCDs account for about 33% of all deaths in Tanzania [12]. Moreover, NCDs pose a catastrophic economic burden in Tanzania [13, 14]. While Community Health Workers (CHWs) may play a pivotal role in the prevention and control of NCDs, it is unfortunate that both the national NCDs Strategic Plan of 2008–2018 and 2016–2020 in Tanzania did not clearly indicate their role [15, 16]. Of note, the current Tanzania National NCD Strategic Plan of 2021–2026 embraces a multisectoral collaboration approach with the development of NCD training manuals for primary healthcare facilities [17].
CHWs have been identified as an important part of the public health workforce globally and have been mobilized to provide primary healthcare at the community and household levels [18]. These are trained individuals that assist in providing health promotion, prevention, community empowerment, administering basic curative health services, and linking local communities with health facilities within their locality with the aim being to reduce morbidity and mortality [19]. Despite their potential role in the healthcare system, their role and contributions in many countries, including Tanzania, are mostly limited to maternal and child health like their participation in the immunization of vaccine preventable diseases as well as prevention and treatment of infectious diseases like TB and HIV while majority of their tasks are highly fragmented as their program driven [20]. CHWs are mostly trained to fill the health provider gaps in health systems and healthcare delivery, especially in developing countries due to the shortage of healthcare workers which is more vivid at the primary healthcare level like in Tanzania, whereby HRH gap is at 52% of the needed staffing level by 2021. In developing countries like Tanzania, addressing the recognized major NCDs such as CVD, cancer, diabetes, and chronic respiratory diseases is necessary at the primary care level considering the rising burden of morbidity and mortality they are causing [7, 21]. Through this, different programs and action plans for NCDs are therefore being strengthened for primary prevention and control, and CHWs have the potential to offer support in the provision of primary healthcare services [22, 23]. To address the gaps in human resources for health regarding NCDs, the mobilization of CHWs shows to have promising results [24, 25]. Evidence suggests various roles like community mobilization and screening, and the relevance of CHWs in the management of different NCDs [26].
Given the pivotal role which CHWs can play in prevention and control of NCDs in their communities, a 2017 study in Uganda showed that most of them had little awareness about most NCDs, as a result, this hindered their effectiveness [27]. Another study of 2022 in Uganda reported that the majority of CHWs (75.3%) had general awareness about different NCDs [28]. Moreover, more than half of the study participants reported being involved in NCDs activities like community mobilization in their communities. Several studies have shown that the majority of CHWs had significant knowledge on prevention and control measures toward some NCDs [28, 29]. Importantly, most CHWs admitted the fact that NCDs burden is a significant public health problem and they have a key role to play in prevention and control [27, 28].
Despite the fact that there are limited studies on the proportion of CHWs engaging in the practice of NCDs prevention and control in their communities, the study in Uganda reported that 63.1% of CHWs were involved in NCDs activities even though only few of them participated in community mobilization (20.9%) and referral of patients (20.6%) [28]. Another study reported that more than half of the participants were involved in community education and counseling on cervical cancer among all NCDs [29].
In one study, CHWs reported that lack of knowledge, lack of training, and negative community perception of NCDs among community members as challenges which prevent them from being effective in addressing NCDs in their communities even though another study reported that lack of financial remuneration was not a barrier in providing NCDs-related services [27, 28]. Some studies pointed contrary that financial remuneration plays a role in CHWs participation in fighting NCDs [30, 31].
Despite other countries like India having established the role of CHWs in NCDs prevention and control, the role of CHWs in delivering primary prevention and control interventions for NCDs in Tanzania is limited [32-34]. Most CHWs are willing and wish to participate in different NCDs intervention programs but do not have knowledge on NCDs to enable them offer required preventive and control measures despite easy availability of online WHO community-based guidelines resources which includes prevention and control of NCDs [WHO Package for Essential Non-communicable (PEN) diseases interventions for primary healthcare] [35, 36]. Moreover, evidence suggests that CHWs are interested in delivering NCDs' prevention services within their communities and thus it is crucial to understand their level of knowledge, attitudes, and perceived role in addressing NCDs as part of the feasibility of involving them in the prevention and control of these diseases [37, 38]. Information on the knowledge and attitudes of CHWs regarding NCDs would provide insights into the competencies and training needs for them to perform their tasks effectively. This study will assess the involvement of CHWs in the prevention and control of NCDs in northern Tanzania with a focus on their knowledge, attitudes and practices, and finding out related determinants. Results will enable policymakers and community health-related stakeholders to formulate and implement informed interventions in providing CHWs with a conducive and enabling environment toward the prevention and control of NCDs in their communities.
2 Materials and Methodology
The reporting of this study has followed the STROBE guideline [39].
2.1 Study Design, Setting, and Population
This was a community-based analytical cross-sectional study conducted from May 2023 to September 2023 among 191 CHWs in northern Tanzania, specifically from Moshi Municipal in Kilimanjaro and Arusha Municipal in Arusha. Moshi and Arusha Municipals are urban districts located in northern Tanzania. They were purposively selected due to the presence of the most active CHWs-based programs in northern Tanzania. The eligibility criteria were: a participant who was 18 years or older during the time of the study, registered and assigned as a CHW in a study area. The exclusion criteria were: CHWs who have retired or not active.
Moshi Municipal and Arusha Municipal have 90 and 154 registered CHWs, respectively, making a total of 244. Based on the total number of CHWs in the study area, the sample size was calculated using Epi-Info statistical software and the minimum required sample size was 150. Convenience sampling technique was used to enroll participants in the study.
2.2 Data Collection Methods and Tools
An interviewer-administered questionnaire was used for data collection adapted from previous studies with already validated tools [28, 29]. The questionnaire was both in English and Swahili languages. It was tested and modified with a series of consultation from NCD and community health experts prior to actual data collection.
Trained research assistants administered the questions using an electronic tool (KOBO) with a total of 52 questions. The first section comprised questions on demographic characteristics of participants such as age, gender, level of education, and social economic status (employment); the second section assessed knowledge of CHWs on NCDs, including whether they can correctly define NCDs or know examples of such diseases, as well as if they think these diseases can be prevented and/or treated, and methods of prevention and control. Specific knowledge on causes, risk factors, and complications of different NCDs was also assessed in this section. The third section explored the attitudes of the CHWs toward NCDs and their burden in Tanzania. This was assessed using a Likert scale (Strongly agree, Agree, Neutral, Strongly disagree, and Disagree). The fourth section assessed the current involvement of CHWs in the prevention and control of NCDs. This was determined in an aspect of whether they have been involved in NCD screening, patient management, palliative care, and/or community mobilization. The level of confidence in their involvement in these activities was also assessed in this section using a Likert scale (Not confident at all, A little confident, Moderately confident, Confident, Very confident). The fifth section intended to assess on the possible factors that contributes either positively or negatively to the CHWs' involvement in NCDs prevention and control in their communities like availability of tools for NCD screening, including challenges/barriers faced based on Likert scale ranging Strongly disagree to Strongly agree in the following areas: low NCD knowledge, lack of training on NCDs, poor community perception toward NCDs, and lack of support from health workers/nearby health facility.
2.3 Study Variables
The main outcomes of interest were knowledge score, favorable attitude, and practices/involvement of CHWs in NCD prevention and control. Knowledge score was determined from the number of questions answered correctly out of the total knowledge questions. More than 50% of the questions answered correctly were translated as satisfactory knowledge. Moreover, perceived knowledge on five major NCDs was also assessed by five questions on a 4-point Likert scale where the responses, I don't know, I know a little, I know some, and I know a lot, had scores 0 through 3, respectively. The highest possible score was 15, the lowest being 0. Therefore, good perception was defined by a score of more than 50% of the highest score.
For attitude, a 5-point Likert scale was used for a total of six questions of which the score ranging from 1 for Strongly disagree to 5 for Strongly agree, thus the highest possible attitude score was 30, the lowest being 6. Attitude score more than 50% of the highest possible score was regarded as favorable attitude.
Practice (involvement of CHWs on NCD prevention and control) was determined by four major variables, which were CHWs involvement in “NCD screening,” “patient management,” “patient care,” and “community mobilization.” Of these, community mobilization was ascertained from nine different questions regarding the CHWs' frequency of discussing the common NCDs and their risk factors which were on a 5-point Likert scale where the responses Never and Always were given a score 1 and 5, respectively. The highest possible score was 45. The participant's score of more than 50% of the total was regarded as good health mobilization. The average of the four variables was then used to elicit the involvement of CHWs in the NCD prevention and control where being involved in two or more activities stated was translated as good practice.
2.4 Data Analysis
Data cleaning and analysis were performed using the SPSS, 20th version. Frequencies and percentages were used to summarize categorical variables while means/medians and standard deviations/Interquartile range for numerical variables. The two-sided χ2 test was used to determine factors associated with CHWs' involvement in NCDs prevention and control with statistical significance at p < 0.05 after which logistic regression estimated the odds ratio (OR) with the 95% confidence interval.
2.5 Ethical Approval and Consent to Participate
Ethical approval was sought from Kilimanjaro Christian Medical University College Research and Ethics Review Committee (KCMUCo-CRERC) with certificate registration number 2610. Permission letters to conduct a study were obtained from local government authorities in Moshi and Arusha Municipals. Moreover, written informed consent was obtained from each participant after explaining to them and reading the study information prior to start filling the survey so that they can make an informed decision to participate or withdraw from the study without losing their dignity. The consent information contained a description of the study purpose, risk and benefits of participation, nature of participant involvement, and confidentiality. Also, the privacy and safety of the participants' information were considered during the study by using a unique identification number instead of their names. Participation in this study was voluntary and participants were allowed to terminate their participation or not responding to a certain question willingly.
3 Results
3.1 Participants' Background Characteristics
A total of 191 CHWs met the inclusion criteria and were enrolled. Their mean age was 45 ± 12 years. Majority (146, 76.4%) were females and 115 (60.2%) were practicing in Arusha. Over half (112, 58.6%) had a working experience of < 10 years as CHW and the vast majority (177, 92.7%) admitted to have received a special training as CHW mostly by physicians (96, 50.3%) (Table 1).
| Variable | n | % |
|---|---|---|
| Sex | ||
| Male | 45 | 23.6 |
| Female | 146 | 76.4 |
| Age (years) | ||
| Mean (SD) | 45.04 (12.16) | |
| < 25 | 8 | 4.2 |
| 25–34 | 37 | 19.4 |
| 35–44 | 36 | 18.8 |
| 45+ | 110 | 57.6 |
| Area of practice | ||
| Kilimanjaro | 76 | 39.8 |
| Arusha | 115 | 60.2 |
| Education level | ||
| Primary education | 91 | 47.6 |
| Secondary education | 69 | 36.1 |
| Higher education | 31 | 16.2 |
| Working experience as CHW | ||
| < 10 years | 112 | 58.6 |
| 10+ years | 79 | 41.4 |
| Any special training as CHW? | ||
| Yes | 177 | 92.7 |
| No | 14 | 7.3 |
| Home visits per week | ||
| < 3 | 90 | 47.1 |
| 3+ | 101 | 52.9 |
| Frequency of trainings from health professionals | ||
| At least once a week | 10 | 5.2 |
| At least once a month | 23 | 12.0 |
| At least once every 2 months | 145 | 75.9 |
| At least once every 6 months | 13 | 6.8 |
| Group of health professionals from whom you receive formal teachings | ||
| Physicians | 96 | 50.3 |
| Nurses | 17 | 8.9 |
| Medical residents/students | 2 | 1.0 |
| Other CHWs | 47 | 24.6 |
| Other educators | 29 | 15.2 |
| Occupation | ||
| Not employed | 39 | 20.4 |
| Self-employed | 143 | 74.9 |
| Employed | 9 | 4.7 |
3.2 CHWs' Knowledge on NCDs' Prevention and Control
Majority of the CHWs (117, 89.7%) defined correctly what NCDs are. Most CHWs stated the examples of NCDs including diabetes (97.9%), hypertension (95.3%), and stroke (84.3%). In total, 99% of CHWs agreed that smoking affects person's health, however, only a few (7.3%) knew the cut-off points for overweight BMI, and 27.7% knew the recommended time for moderate-intensity physical activity per week. Knowledge on hypertension, diabetes, chronic obstructive pulmonary diseases (COPD), and cancer screening was also assessed. Overall, 92.1% had satisfactory knowledge scores on NCDs prevention and control (Table 2). Also, perceived general knowledge on different NCDs was assessed with most CHWs (60.2%) having poor perception on their knowledge of the medical conditions (Table 3).
| Variable | Category | n | % |
|---|---|---|---|
| NCD cannot be spread between people | True | 117 | 89.5 |
| False | 15 | 7.5 | |
| I don't know | 5 | 2.6 | |
| Examples of NCDs | Diabetes | 187 | 97.9 |
| Tuberculosis | 5 | 2.6 | |
| Asthma | 141 | 73.8 | |
| Stroke | 162 | 84.8 | |
| AIDS | 4 | 2.1 | |
| Cancer | 161 | 84.3 | |
| Malaria | 93 | 48.7 | |
| Hypertension | 182 | 95.3 | |
| I don't know | 2 | 1.0 | |
| Active smoking affects a person's health | True | 189 | 99 |
| False | 1 | 0.5 | |
| I don't know | 1 | 0.5 | |
| Smoking around others does not harm their health | True | 141 | 73.8 |
| False | 49 | 25.7 | |
| I don't know | 1 | 0.5 | |
| Smoking affects lungs | True | 190 | 99.5 |
| False | 0 | 0 | |
| I don't know | 1 | 0.5 | |
| Smoking affects the heart | True | 133 | 69.6 |
| False | 24 | 12.6 | |
| I don't know | 34 | 17.8 | |
| Source with largest amount of salt | The table salt added to food | 173 | 90.6 |
| The salt in milk, meat, and vegetables | 0 | 0 | |
| The salt in factory-made foods like bread, sausages, and canned foods | 9 | 4.7 | |
| I don't know | 9 | 4.7 | |
| Which BMI is considered as being overweight | Correct response (25–29.9) | 14 | 7.3 |
| Incorrect response | 46 | 24.1 | |
| I don't know | 131 | 68.6 | |
| Total time of moderate-intensity physical activity per week | Correct response (150 min/week) | 53 | 27.7 |
| Incorrect response | 81 | 42.4 | |
| I don't know | 57 | 29.8 | |
| Risky diet for NCDs | Junk/processed foods | 169 | 88.5 |
| Natural foods | 9 | 4.7 | |
| I don't know | 13 | 6.8 | |
| Knowledge on high blood pressure and risk factors | |||
| Effect of salt on blood pressure | Correct response (raises blood pressure) | 160 | 83.8 |
| Incorrect response | 9 | 4.7 | |
| I don't know | 22 | 11.5 | |
| High blood pressure affects the following body parts | |||
| The brain | Yes | 140 | 73.3 |
| No | 20 | 10.5 | |
| I don't know | 31 | 16.2 | |
| The kidneys | Yes | 108 | 56.5 |
| No | 31 | 16.2 | |
| I don't know | 52 | 27.2 | |
| The stomach | Yes | 27 | 14.1 |
| No | 84 | 44 | |
| I don't know | 80 | 41.9 | |
| The heart | Yes | 168 | 88 |
| No | 8 | 4.2 | |
| I don't know | 15 | 7.9 | |
| People with high blood pressure are more likely to have stroke | True | 167 | 87.4 |
| False | 4 | 2.1 | |
| I don't know | 20 | 10.5 | |
| Cardiovascular diseases risk factors | Insomnia | 146 | 76.4 |
| Running | 48 | 25.1 | |
| Stress | 177 | 92.7 | |
| Older age | 141 | 73.8 | |
| Higher BMI | 182 | 95.3 | |
| Vegetarian diet | 5 | 2.6 | |
| Smoking | 142 | 74.3 | |
| Knowledge on diabetes | |||
| Diabetes is when there is chronically high blood sugar | True | 157 | 82.2 |
| False | 13 | 6.8 | |
| I don't know | 21 | 11 | |
| Signs and symptoms of diabetes type 2 | Frequent urination | 180 | 94.2 |
| Increased thirst | 145 | 75.9 | |
| Loss of appetite | 103 | 53.9 | |
| Weight loss | 160 | 83.8 | |
| Fatigue | 171 | 89.5 | |
| I don't know | 9 | 4.5 | |
| The following is not a complication of Diabetes | Damage to the heart | 106 | 55.5 |
| Loss of vision | 140 | 73.3 | |
| Loss of memory | 131 | 68.6 | |
| Loss of sensation to the feet | 135 | 70.7 | |
| Damage to the kidneys | 122 | 63.9 | |
| Erectile dysfunction | 133 | 69.6 | |
| Poor healing of wounds | 138 | 72.3 | |
| I don't know | 12 | 6.3 | |
| Knowledge on COPD | |||
| Causes of COPD | Air pollution | 167 | 87.4 |
| Chronic asthma | 145 | 75.9 | |
| Genetics | 123 | 64.4 | |
| Smoking | 172 | 90.1 | |
| Recurrent lung infections | 128 | 67 | |
| I don't know | 13 | 6.8 | |
| Signs and symptoms of COPD | Cough | 174 | 81.1 |
| Leg swelling | 109 | 57.1 | |
| Shortness of breath | 175 | 91.6 | |
| Fatigue | 160 | 83.8 | |
| Sputum production | 160 | 83.8 | |
| I don't know | 12 | 6.3 | |
| Knowledge on cancer screening | |||
| Medical condition screened with pap test | Sexually transmitted infections | 9 | 4.7 |
| Cervical cancer | 40 | 20.9 | |
| Ovarian cancer | 7 | 3.7 | |
| Pregnancy | 3 | 1.6 | |
| Syphilis | 6 | 3.1 | |
| I don't know | 150 | 78.5 | |
| When to undergo a pap test for asymptomatic average-risk women | Correct response (21 years) | 25 | 13.1 |
| Incorrect response | 19 | 9.9 | |
| I don't know | 147 | 77 | |
| How often should women who had two normal pap tests continue having the test? | Correct response (2–3 years) | 8 | 4.2 |
| Incorrect response | 32 | 16.8 | |
| I don't know | 151 | 79.1 | |
| Can cervical cancer be prevented by vaccine? | Yes | 156 | 81.7 |
| No | 14 | 7.3 | |
| I don't know | 21 | 11 | |
| At what age should a woman start screening for breast cancer regularly? | Correct response (30–40 years) | 39 | 20.4 |
| Incorrect response | 109 | 57.1 | |
| I don't know | 43 | 22.5 | |
| At what age should a man start screening for prostate cancer? | Correct response (above 45) | 85 | 44.5 |
| Incorrect response | 56 | 29.3 | |
| I don't know | 50 | 26.2 | |
| Overall NCDs knowledge | Satisfactory Knowledge | 176 | 92.1 |
| Poor Knowledge | 15 | 7.9 | |
| Variable | Category | n | % |
|---|---|---|---|
| High blood pressure | I know a little | 99 | 51.8 |
| I know some | 50 | 26.2 | |
| I know a lot | 30 | 15.7 | |
| I don't know | 12 | 6.3 | |
| Myocardial infarction | I know a little | 88 | 46.1 |
| I know some | 45 | 23.6 | |
| I know a lot | 12 | 6.3 | |
| I don't know | 46 | 24.1 | |
| Stroke | I know a little | 82 | 42.9 |
| I know some | 39 | 20.4 | |
| I know a lot | 29 | 15.2 | |
| I don't know | 41 | 21.5 | |
| Diabetes | I know a little | 87 | 45.5 |
| I know some | 38 | 19.9 | |
| I know a lot | 56 | 29.3 | |
| I don't know | 10 | 5.2 | |
| Chronic obstructive pulmonary diseases (COPD) | I know a little | 81 | 42.2 |
| I know some | 46 | 24.1 | |
| I know a lot | 25 | 13.1 | |
| I don't know | 39 | 20.4 | |
| General perceived knowledge of NCDs | Good Perception | 76 | 39.8 |
| Poor Perception | 115 | 60.2 |
3.3 CHWS' Attitudes Toward NCD Burden, Prevention, and Control
Majority (152, 79.6%) of the CHWs agreed that NCDs are now common among Tanzanians including CVDs, diabetes, and cancer. In total, 99.5% of the CHWs agreed that early detection of NCDs plays an important role in their prevention and control. Most of the CHWs (97.9%) agreed that they have a very important role to play in NCDs' prevention and control in their communities (Table 4). Generally, all CHWs (100%) had favorable attitude.
| Statement | Strongly agree (%) | Agree (%) | Neutral (%) | Disagree (%) | Strongly disagree (%) |
|---|---|---|---|---|---|
| NCDs are common among Tanzanians | 58 (30.4) | 94 (49.2) | 8 (4.2) | 28 (14.7) | 3 (1.6) |
| Cardiovascular diseases are becoming more common in Tanzania | 64 (33.5) | 117 (61.3) | 4 (2.1) | 6 (3.1) | 0 (0) |
| Diabetes is becoming more common in Tanzania | 75 (39.3) | 108 (56.5) | 4 (2.1) | 4 (2.1) | 0 (0) |
| Cancer is becoming more common in Tanzania in general | 77 (40.3) | 99 (51.8) | 7 (3.7) | 7 (3.7) | 1 (0.5) |
| Early detection plays an important role in NCDs prevention and control | 94 (49.2) | 96 (50.3) | 1 (0.5) | 0 (0) | 0 (0) |
| As a community health worker, I have a very important role to play in NCDs prevention and control in my community | 71 (37.2) | 116 (60.7) | 4 (2.1) | 0 (0) | 0 (0) |
| Attitudes toward NCDs burden, prevention, and control | n | % | |||
|---|---|---|---|---|---|
| Favorable attitude | 191 | 100 | |||
| Unfavorable attitude | 0 | 0 |
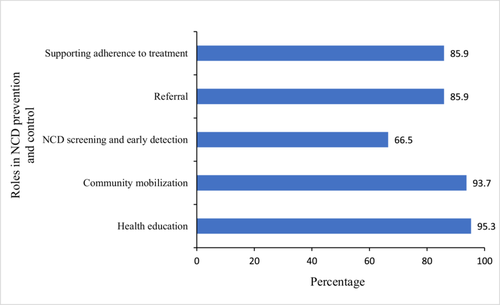
Figure 1 highlights the roles which CHWs identified they can play in prevention and control of NCDs. The vast majority (95.3% and 93.7%) identified that they have a role to play in providing health education and community mobilization, respectively, while 66.5% believed they had a role to play in NCD screening and early detection.
3.4 CHWs' Practice Involvement, Enabling Factors, and Challenges Toward NCDs Prevention and Control
Overall, 63.4% of the CHWs were involved in at least one of the activities related to NCDs prevention and control. The activities include NCD screening (26.7%), patient management (12.0%), patient care (41.9%), and health mobilization whereby 41.4% had good mobilization. Community health mobilization was ascertained from the questions regarding their frequency of discussing NCD-related topics (responses are depicted in the table) (Table 5).
| Variable | Categories | n | % |
|---|---|---|---|
| NCDs prevention and control activities involved | NCDs screening | 51 | 26.7 |
| Patient management | 23 | 12.0 | |
| Patient care | 80 | 41.9 | |
| Frequency of discussing NCD-related topics in your community | |||
| Harms of smoking | Never | 7 | 3.7 |
| Rarely | 29 | 15.2 | |
| Sometimes | 20 | 10.5 | |
| Often | 93 | 48.7 | |
| Always | 42 | 22 | |
| Harms of alcohol | Never | 9 | 4.7 |
| Rarely | 20 | 10.5 | |
| Sometimes | 16 | 8.4 | |
| Often | 91 | 47.6 | |
| Always | 55 | 28.8 | |
| Healthy nutrition | Never | 4 | 2.1 |
| Rarely | 16 | 8.4 | |
| Sometimes | 30 | 15.7 | |
| Often | 78 | 40.8 | |
| Always | 63 | 33 | |
| Physical activity | Never | 6 | 3.1 |
| Rarely | 26 | 13.6 | |
| Sometimes | 26 | 13.6 | |
| Often | 82 | 42.9 | |
| Always | 51 | 26.7 | |
| Weight control | Never | 7 | 3.7 |
| Rarely | 30 | 15.7 | |
| Sometimes | 28 | 14.7 | |
| Often | 84 | 44 | |
| Always | 42 | 22 | |
| Cervical cancer screening | Never | 36 | 18.8 |
| Rarely | 27 | 14.1 | |
| Sometimes | 18 | 9.4 | |
| Often | 67 | 35.1 | |
| Always | 43 | 22.5 | |
| Breast cancer screening | Never | 49 | 25.7 |
| Rarely | 39 | 20.4 | |
| Sometimes | 16 | 8.4 | |
| Often | 59 | 30.9 | |
| Always | 28 | 14.7 | |
| Prostate cancer screening | Never | 67 | 35.1 |
| Rarely | 60 | 31.4 | |
| Sometimes | 20 | 10.5 | |
| Often | 35 | 18.3 | |
| Always | 9 | 4.7 | |
| Colon cancer | Never | 133 | 69.6 |
| Rarely | 28 | 14.7 | |
| Sometimes | 10 | 5.2 | |
| Often | 9 | 4.7 | |
| Always | 11 | 5.8 | |
| General mobilization | Good Mobilization | 79 | 41.4 |
| Poor Mobilization | 112 | 58.6 | |
| Involvement in NCDs prevention and control | Yes | 121 | 63.4 |
| No | 70 | 36.6 | |
| Level of confidence in accurately doing the following as a CHW | |||
| NCD screening | Not confident at all | 42 | 22 |
| A little confident | 21 | 11 | |
| Moderately confident | 33 | 17.3 | |
| Confident | 66 | 34.6 | |
| Very confident | 29 | 15.2 | |
| Patient management | Not confident at all | 88 | 46.1 |
| A little confident | 20 | 10.5 | |
| Moderately confident | 23 | 12 | |
| Confident | 40 | 20.9 | |
| Very confident | 20 | 10.5 | |
| Patient care (including palliative care) | Not confident at all | 48 | 25.1 |
| A little confident | 17 | 8.9 | |
| Moderately confident | 25 | 13.1 | |
| Confident | 62 | 32.5 | |
| Very confident | 39 | 20.4 | |
| Level of confidence in accurately counseling community members about the following topics | |||
| Harms of smoking | Not confident at all | 3 | 1.6 |
| A little confident | 8 | 4.2 | |
| Moderately confident | 32 | 16.8 | |
| Confident | 82 | 42.9 | |
| Very confident | 66 | 34.6 | |
| Harms of alcohol | Not confident at all | 4 | 2.1 |
| A little confident | 9 | 4.7 | |
| Moderately confident | 25 | 13.1 | |
| Confident | 84 | 44 | |
| Very confident | 69 | 36.1 | |
| Healthy nutrition | Not confident at all | 4 | 2.1 |
| A little confident | 11 | 5.8 | |
| Moderately confident | 22 | 11.5 | |
| Confident | 80 | 41.9 | |
| Very confident | 74 | 38.7 | |
| Physical activity | Not confident at all | 6 | 3.1 |
| A little confident | 10 | 5.2 | |
| Moderately confident | 25 | 13.1 | |
| Confident | 87 | 45.5 | |
| Very confident | 63 | 33 | |
| Weight control | Not confident at all | 7 | 3.7 |
| A little confident | 16 | 8.4 | |
| Moderately confident | 24 | 12.6 | |
| Confident | 86 | 45 | |
| Very confident | 58 | 30.4 | |
| Cervical cancer screening | Not confident at all | 36 | 18.8 |
| A little confident | 16 | 8.4 | |
| Moderately confident | 24 | 12.6 | |
| Confident | 86 | 45 | |
| Very confident | 58 | 30.4 | |
| Breast cancer screening | Not confident at all | 55 | 28.8 |
| A little confident | 23 | 12 | |
| Moderately confident | 29 | 15.2 | |
| Confident | 45 | 23.6 | |
| Very confident | 39 | 20.4 | |
| Prostate cancer screening | Not confident at all | 82 | 42.9 |
| A little confident | 26 | 13.6 | |
| Moderately confident | 23 | 12 | |
| Confident | 40 | 20.9 | |
| Very confident | 20 | 10.5 | |
| Colon cancer | Not confident at all | 123 | 64.4 |
| A little confident | 23 | 12 | |
| Moderately confident | 17 | 8.9 | |
| Confident | 17 | 8.9 | |
| Very confident | 11 | 5.8 | |
| General confidence in involvement toward NCD prevention and control | High Confidence | 133 | 69.6 |
| Low Confidence | 58 | 30.4 | |
| Enabling factors | |||
| Ever attended a seminar or formal training on NCDs | Yes | 88 | 46.1 |
| No | 103 | 53.9 | |
| Years Past NCDs' Seminar or formal training. | < 2 | 45 | 51.1 |
| 2+ | 43 | 48.9 | |
| Accessibility of tools/materials for any of the following | |||
| NCD Screening | Yes | 69 | 36.1 |
| No | 122 | 63.9 | |
| Patient Management | Yes | 381 | 19.9 |
| No | 153 | 80.1 | |
| Palliative Care | Yes | 92 | 48.2 |
| No | 99 | 51.8 | |
| Challenges faced in your involvement in different activities in your community toward NCDs prevention and control | |||
| Lack/insufficient knowledge on NCDs prevention and control | Yes | 161 | 84.3 |
| No | 30 | 15.7 | |
| Poor support from health providers (health facilities) | Yes | 99 | 51.8 |
| No | 92 | 48.2 | |
| Lack of good remuneration | Yes | 148 | 77.5 |
| No | 43 | 22.5 | |
| Negative community perception on NCDs | Yes | 129 | 67.5 |
| No | 62 | 32.5 | |
| Lack of community trust in CHWs skills on NCDs prevention and control | Yes | 96 | 50.3 |
| No | 95 | 49.7 | |
CHWs' level of confidence in their involvement in these activities was also assessed by 12 different questions on a 5-point Likert scale where the majority (69.6%) had high confidence (determined by those with a score of more than 50% of the total score) (Table 5).
In total, 53.9% of the CHWs had ever attended a seminar or formal training on NCDs with half of them (51.1%) attending within the last year. Majority of the CHWs experienced difficulty in accessing tools to facilitate their involvement in the NCD prevention and control activities with only 36.1% having access to tools for NCD screening (Table 5).
Among many challenges the CHWs face in their involvement in different activities of NCD prevention and control, majority identified insufficient knowledge on NCDs' prevention and control (84.3%) and lack of good remuneration (77.5%) as two major challenges (Table 5).
3.5 Determinants of the CHWs' Involvement in NCDs Control and Prevention Activities
CHWs' involvement on NCD prevention and control was significantly associated with whether they have attended any special training (p < 0.001), home visits per week (p = 0.003), general confidence toward their involvement in NCD prevention and control (p < 0.001), attendance on a seminar or formal training (p < 0.001), and accessibility for tools of NCD screening (p < 0.001) (Table 6).
| Variable | Practice | p | COR (95% CI) | p | |
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Sex | 0.22 | ||||
| Male | 32 (71.1) | 13 (28.9) | |||
| Female | 89 (61.0) | 57 (39.0) | |||
| Age | 0.64 | ||||
| < 25 | 4 (50) | 4 (50) | |||
| 25–34 | 21 (56.8) | 16 (43.2) | |||
| 35–44 | 24 (66.7) | 12 (33.3) | |||
| 45+ | 72 (65.5) | 38 (34.5) | |||
| Education level | 0.59 | ||||
| Primary education | 55 (60.4) | 36 (39.6) | |||
| Secondary education | 47 (68.1) | 22 (31.9) | |||
| Higher education | 19 (61.3) | 12 (38.7) | |||
| Working experience as CHW | 0.55 | ||||
| < 10 | 69 (61.6) | 43 (38.4) | |||
| 10+ | 52 (65.8) | 27 (34.8) | |||
| Any special training as CHW? | < 0.001* | ||||
| Yes | 119 (67.2) | 58 (32.8) | 12.31 (2.67–56.82) | 0.001* | |
| No | 2 (14.3) | 12 (85.7) | 1 | ||
| Home visits per week | 0.003* | ||||
| < 3 | 47 (52.2) | 43 (47.8) | 1 | ||
| 3+ | 74 (73.3) | 27 (26.7) | 2.51 (1.37–4.59) | 0.003* | |
| Occupation | 0.57 | ||||
| Not employed | 23 (59) | 16 (41) | |||
| Self-employed | 91 (63.6) | 52 (36.4) | |||
| Employed | 7 (77.8) | 2 (22.2) | |||
| Overall knowledge | 0.05 | ||||
| Good Knowledge | 115 (65.3) | 61 (34.7) | |||
| Poor Knowledge | 6 (40) | 9 (60) | |||
| General perceived knowledge | 0.14 | ||||
| Good Perception | 53 (69.7) | 23 (30.3) | |||
| Poor Perception | 68 (59.1) | 47 (40.9) | |||
| General confidence toward NCD prevention and control | < 0.001* | ||||
| High confidence | 107 (80.5) | 26 (19.5) | 12.93 (6.28–27.07) | < 0.001* | |
| Low confidence | 14 (24.1) | 44 (75.9) | 1 | ||
| Seminar/formal training on NCD | < 0.001* | ||||
| Yes | 71 (80.7) | 17 (19.3) | 4.43 (2.3–8.53) | < 0.001* | |
| No | 50 (48.5) | 53 (51.5) | 1 | ||
| Accessibility of tools for NCD screening | < 0.001* | ||||
| Yes | 64 (92.8) | 5 (7.2) | 14.6 (5.5–38.8) | < 0.001* | |
| No | 57 (46.7) | 65 (53.3) | 1 | ||
| Challenges faced in your involvement in different activities in your community toward NCDs prevention and control | |||||
| Lack/insufficient of knowledge on NCDs prevention and control | |||||
| Yes | 105 (65.2) | 56 (34.8) | |||
| No | 16 (53.3) | 14 (46.7) | 0.22 | ||
| Poor support from health providers (health facilities) | |||||
| Yes | 61 (61.6) | 38 (38.4) | |||
| No | 60 (65.2) | 32 (34.8) | 0.61 | ||
| Lack of good remuneration | |||||
| Yes | 92 (62.2) | 56 (37.8) | |||
| No | 29 (67.4) | 14 (32.6) | 0.53 | ||
- Abbreviations: COR = crude odds ratio; CI = confidence interval.
- * p < 0.05.
In crude analysis, CHWs who received special training were 12 times more likely to be involved in NCD prevention and control activities (OR = 12.31, 95% CI 2.67, 56.82); those who make more than two home visits per week were 3 times as likely to be involved (OR = 2.51, 95% CI 1.37, 4.59); those with high confidence toward their involvement also were almost 13 times likely of being involved in NCD prevention and control activities (OR = 12.93, 95% CI 6.28, 27.07). Furthermore, those who attended any seminar or formal training on NCD were 4 times more likely to be involved in NCD prevention and control activities (OR = 4.43, 95% CI 2.3, 8.53); and those who had access to tools for NCD screening were almost 15 times as likely to be involved (OR = 14.6, 95% CI 5.5, 38.8) (Table 6).
4 Discussion
The aim of this study was to determine knowledge, attitude, practice, and determinants toward CHWs' involvement in NCDs prevention and control in northern Tanzania. Study findings show that majority of CHWs in northern Tanzania have general knowledge on different NCDs while all of them had favorable attitude toward the burden of NCDs in Tanzania and their involvement as among stakeholders. While more than half of CHWs (63.4%) were found to have been involved themselves in NCDs prevention and control activities, only 26.7% and 46.1% of CHWs were involved in screening activities and had attended NCDs-related training or seminar, respectively.
More than half of CHWs had good overall knowledge of different NCDs and had been involved in prevention and control activities as it has been reported in several studies done in Uganda [28, 29]. Moreover, most of the CHWs had favorable attitude toward the burden of NCDs in their communities and the role they can play as it was found in previous studies [27, 28]. This portrays interest, willingness, and readiness of CHWs to involve themselves in NCDs prevention and control activities which is a key step in ensuring healthcare for all and sustainability in terms of availability of primary healthcare services at the community level. This will not only enhance early prevention and control of NCDs but also will enable community members to access routine screening, respective health counseling and referrals, community-based treatment, and palliative care support for different NCDs for free at no cost while at home. Furthermore, this might significantly reduce NCDs economic burden in Tanzania and enhance health-seeking behaviors such as routine health checkups against NCDs and related complications among community members [13, 14]. On the other hand, the finding that only 46.1% had attended NCDs-related training contradicts with the fact that the majority had good overall NCDs knowledge. This might be attributed to reporting and self-desirability bias as this conclusion was based on self-reported knowledge.
Investing in CHWs as a community-based strategy for NCD prevention and control is a cost-effective approach that delivers significant benefits [19, 24-26]. In India, delivery of home-based screening for NCDs by trained CHWs was found to be feasible and acceptable [34]. While screening for NCDs and their respective complications is the key in early detection and control of different NCDs, it is only nearly a quarter of CHWs (26.7%) in northern Tanzania have been involved in screening activities. This might be due to the finding that only 36.1% of participants reported to have access to NCDs screening tools.
Despite the fact that majority of CHWs had good overall knowledge of NCDs (92.1%), favorable attitude on NCDs burden and their involvement (100%) and overall practice involvement confidence (69.6%), still on assessing the enabling factors for their involvement in NCDs prevention and control, only less than half (46.1%) reported to have attended a training or seminar on NCDs while 36.1%, 19.9%, and 48.2% reported to have access to tools for NCDs' screening, patient management, and palliative care, respectively. These findings highlight the possible areas of interventions to facilitate the CHWs' involvement in NCD prevention and control.
Regarding challenges faced by CHWs toward their involvement in NCDs prevention and control practice, one study reported poor remuneration as a barrier while another study reported contrary findings [27, 28, 30, 31]. This study found that despite the fact that poor remuneration was reported by majority CHWs as a barrier toward their involvement in NCDs prevention and control practice, but it was not statistically a significant determinant. Most CHWs reported inadequate NCD knowledge, negative community perception toward NCDs as among challenges toward their involvement in NCDs prevention and control as reported in a study in Uganda [28]. Of note, one of the striking findings is that lack of sufficient knowledge of NCD prevention and control was the major challenge acknowledged by 84.3% of the CHWs, however, the overall knowledge was seen to be high which is contrary to the expectations. This discrepancy could be attributed to the reporting and self-desirability bias credited by the self-reporting nature of the study.
Among statistically significant determinants of CHWs involvement toward NCDs prevention and control; access to NCDs screening tools, professional training to practice as CHWs, frequency of home visits per week, CHW's involvement confidence, NCDs special training or seminar attendance and access to screening tools were strongly associated with CHWs involvement in NCDs prevention and control activities. This might be due to the fact that all these factors directly enable CHWs and increase the chances of their participation.
4.1 Strength and Limitation of the Study
To the best of our knowledge, this is the first study evaluating the role of community healthcare workers in NCD prevention and control in Tanzania, providing valuable insights into their knowledge, attitudes, and involvement. The study was also conducted in areas with the most active CHWs programs in northern Tanzania. This makes the findings more reflective of the status among CHWs in terms of the study aim. Furthermore, it has been conducted amidst the abrupt increase of NCDs cases in Tanzania. The desired sample size was achieved and proper analysis methods were deployed. This has enhanced the precision and power of the study.
On the other hand, self-reported knowledge and involvement of CHWs in NCD prevention and control might have been subjected to reporting and self-desirability bias which might have affected the study findings. Supplementing the study findings with a qualitative aspect would strengthen the findings and the conclusion drawn. This has not been done with this study.
5 Conclusion and Recommendation
CHWs are useful toward prevention and control of different NCDs. Majority of CHWs showed overall good knowledge, favorable attitude, and high involvement in NCDs prevention and control in northern Tanzania. However, only a few of them were involved in community mobilization and screening of different NCDs. Their limited involvement is attributed secondary to several factors including inability to access NCDs screening tools and lack of training tailored to NCDs–CHWs context.
Several CHWs-based programs tailored against NCDs should be implemented to maximize CHWs involvement and effectiveness toward NCDs prevention and control in their local communities. Public health stakeholders, including respective government institutions, should design and implement capacity-building programs among CHWs in terms of trainings for both skills and knowledge acquisition. This should also be incorporated in the national NCDs strategic plans. NCDs training manuals developed in Tanzania for primary healthcare facilities should also be applied toward CHWs. On top of that, these programs should ensure accessibility of tools for screening, patient management, and palliative care among CHWs. Health facilities should work in partnership and harmony locally with CHWs in enabling their involvement toward NCDs prevention and control.
Additionally, professional training to practice as a CHWs should be prioritized in both in service and new enrolled CHWs. This will enhance their knowledge toward their role as CHWs and their involvement in NCDs prevention and control. Since the WHO have made the prevention and control practice guideline (PEN) available to enable CHWs involvement in NCDs prevention and control practice, this guideline should be incorporated among CHWs professional trainings and made available to every CHWs in Swahili format.
Author Contributions
Harold L. Mashauri: conceptualization, data curation, formal analysis, methodology, investigation, project administration, writing – original draft, visualization. Cornel M. Angolile: data curation, methodology, investigation, formal analysis, writing – original draft, visualization. Florida J. Muro: conceptualization, methodology, investigation, formal analysis, writing – review and editing, supervision. All authors have read and approved the final version of the manuscript.
Acknowledgments
We acknowledge local authorities in northern Tanzania for providing us with permission and assistance during conduction of this study. Moreover, we acknowledge Dr. Ntuli Kapologwe for reviewing the final draft of this manuscript. This study was funded by a Joint Non-Communicable Diseases Grant offered by Muhimbili University of Health and Allied Sciences (MUHAS) and Tanzania Diabetes Association (TDA) in Tanzania in 2023. Funders had no involvement in any of the following: study design, data collection, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
Ethics Statement
Ethical approval was sought from Kilimanjaro Christian Medical University College Research and Ethics Review Committee (KCMUCo-CRERC) with certificate registration number 2610. Permission letters to conduct a study were obtained from local government authorities in Moshi and Arusha Municipals.
Consent
Written informed consent was obtained from each participant after explaining to them and reading the study information prior to start filling the survey so that they can make an informed decision to participate or withdraw from the study without losing their dignity.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The lead author Harold L. Mashauri affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
Data Availability Statement
Harold L. Mashauri had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis. Data collected during this study are available from the corresponding author upon a reasonable request.