The Effects of Hyperkyphosis on Gait Parameters in Older Adults: A Systematic Review
ABSTRACT
Background and Aims
Hyperkyphosis, which affects 20%–40% of older adults, is characterized by excessive thoracic curvature and is linked to impaired mobility. Age-related gait changes further complicate this issue, but studies on the relationship between hyperkyphosis and gait parameters have yielded inconsistent results. Focused research is essential to clarify this relationship and develop effective interventions.
Methods
This systematic review examined the effects of hyperkyphosis on gait in older adults ( ≥ 60 years), adhering to PRISMA 2020 guidelines (PROSPERO registration: CRD42024597304). Observational studies were included, while interventions and studies involving younger populations were excluded. Databases (PubMed, Web of Science, Scopus, CINAHL, Cochrane) were systematically searched. Two independent reviewers screened articles, extracted data, and assessed the risk of bias using validated JBI tools (cohort and cross-sectional checklists). Studies were categorized as high-, moderate-, or low-quality ( ≥ 75%, 50%–74%, and < 50% scores, respectively). Discrepancies were resolved through consensus. Results were synthesized qualitatively, focusing on methodological strengths and limitations.
Results
Nineteen studies focusing on older adults with hyperkyphosis were analyzed, highlighting diverse methods for measuring kyphosis and gait parameters. The findings indicated hyperkyphosis adversely affects gait characteristics, including walking speed, step time, and overall mobility. A strong association was found between increased age, reduced muscle mass, and impaired gait performance.
Conclusion
This review underscores the detrimental impact of hyperkyphosis on gait parameters in older adults, emphasizing the need for standardized measurement protocols and early clinical identification. Targeted interventions are essential to enhance gait performance in this population.
Summary
-
What's Known: Hyperkyphosis is associated with impaired gait parameters such as walking speed, stride length, and balance, contributing to mobility limitations in older adults.
-
What's New: This review highlights a significant association between hyperkyphosis severity and decreased gait performance. It identifies that posture-related parameters (e.g., trunk inclination) directly impact gait stability and increase the risk of falls.
-
Clinical Implications: Identifying and addressing hyperkyphosis may improve gait parameters, enhancing balance, mobility, and quality of life for older adults. Tailored interventions can mitigate hyperkyphosis-related declines in functional independence and fall risk.
1 Introduction
Hyperkyphosis, defined by an excessive forward curvature of the thoracic spine, is a common condition affecting approximately 20%–40% of older adults. Recent studies classify it as a geriatric syndrome [1]. Although the precise causes and consequences of hyperkyphosis remain incompletely understood, it is well-established that the condition worsens with age. While vertebral osteoporosis is often considered a major contributing factor, only about one-third of individuals with advanced hyperkyphosis exhibit vertebral fractures or reduced bone mineral density. This suggests that other factors, such as muscle weakness, genetic predisposition, and environmental influences, likely contribute to its onset and progression [2, 3].
Hyperkyphosis is associated with numerous adverse health outcomes, including impaired pulmonary and physical function, increased fall risk, and balance deficits. These complications often lead to vertebral fractures due to excessive spinal pressure, as well as fall-related fractures in other body parts. Additionally, hyperkyphosis contributes to loss of independence, negative impacts on physical appearance, and social and psychological challenges. It has also been linked to an increased risk of premature mortality [2, 3].
In older adults, gait patterns undergo significant alterations, with nearly 35% of those over 70 experiencing gait disorders [4]. These age-related changes include slower walking speeds, a wider base of support, and a cautious gait pattern, with walking speed declining by approximately 1% annually after age 60 [5]. In individuals with hyperkyphosis, additional postural changes—such as forward head posture, thoracic kyphosis, and loss of lumbar lordosis—contribute to an increased base of support, slight knee flexion, and trunk forward lean, resulting in compensatory hip flexion [5, 6]. These factors drive degenerative processes in the spine and hip joints, shift the body's center of mass forward, and alter the range of motion and alignment of lower extremity joints. Consequently, gait becomes further impaired, increasing risks of falls, disability, and reduced quality of life [5, 7, 8].
Given the effects of hyperkyphosis on gait, numerous studies have explored this relationship, often yielding conflicting findings. One study found that forward trunk tilt reduces both walking speed and total distance traveled, suggesting that hyperkyphosis may adversely affect walking endurance in older adults [9]. In contrast, another study comparing healthy older adults with those diagnosed with hyperkyphosis reported no significant differences between the groups' walking speed, cadence, step width, or step length. The only notable difference was a higher hip extension moment during the early stance phase in the hyperkyphotic group [10]. Additionally, some research demonstrated that individuals with hyperkyphosis required more time to complete the Timed Up and Go (TUG) test [11, 12], while other studies found no such association [13]. Furthermore, although some studies identified a link between increased kyphotic angle and slower walking speeds [14, 15], others failed to confirm this relationship [6, 16]. A systematic review and meta-analysis exclusively focusing on women with hyperkyphosis examined the association between physical performance and hyperkyphosis. It revealed that more severe hyperkyphosis correlated inversely with overall physical performance and back extensor muscle strength, but no significant relationship was observed with walking speed. Notably, this study's exclusive focus on women precluded gender comparisons and limited the evaluation of hyperkyphosis's impact on gait parameters or their assessment methods [17].
Although hyperkyphosis is highly prevalent and exerts significant effects on gait in older adults, further research is critical to fully elucidate this relationship. The inconsistent findings highlight the necessity for targeted investigations into how hyperkyphosis influences specific gait parameters. Addressing these gaps will advance the development of effective interventions to improve mobility, reduce fall risk, and enhance quality of life in affected individuals.
2 Methods
2.1 Protocol and Registration
This systematic review investigated the effects of hyperkyphosis on gait in older adults, adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines. These guidelines were followed to systematically identify, evaluate, and synthesize relevant studies. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42024597304) to ensure transparency and minimize bias.
2.2 Eligibility Criteria
Eligibility Criteria: Articles published in any language up to the end of October 2024 were considered for this systematic review. Only studies involving participants aged 60 years and older with a diagnosis of thoracic hyperkyphosis—evaluated using any standardized method—were included. Additionally, studies were required to examine the relationship between thoracic hyperkyphosis and at least one gait parameter in clinical or laboratory settings. Observational study designs, including cross-sectional, cohort, and case-control studies, were accepted without imposing restrictions on the specific gait parameters assessed.
Exclusion Criteria: Studies were excluded if they involved participants younger than 60 years or focused solely on interventions (e.g., exercise or medical treatments) targeting gait improvement in individuals with hyperkyphosis. Additionally, studies that did not report gait parameters were omitted. Research involving patients with Scheuermann's kyphosis, concurrent scoliosis and kyphosis, or lumbar hyperkyphosis was also excluded.
2.3 Information Sources and Search Strategy
The search strategy for this systematic review was meticulously designed to identify relevant studies examining the effects of hyperkyphosis on gait in older adults. We searched several databases, including PubMed, Web of Science, Scopus, CINAHL, and the Cochrane Library. Our search utilized a combination of keywords and Medical Subject Headings (MeSH) terms related to hyperkyphosis, gait, and older adults. The specific search strategy is detailed in Table 1, outlining the terms used, the Boolean operators applied, and any filters set to refine the search results.
| Number | Databases | Search strategy | Number of articles retrieved |
|---|---|---|---|
| 1 | Pubmed | (“kyphosis”[Title/Abstract] OR “hyperkyphosis”[Title/Abstract] OR “flexed posture”[Title/Abstract] OR “spinal kyphosis”[Title/Abstract] OR “thoracic kyphosis”[Title/Abstract] OR “excessive kyphosis”[Title/Abstract] OR “kyphotic posture”[Title/Abstract] OR “dowager's hump”[Title/Abstract] OR “hunchback”[Title/Abstract]) AND (“aging”[Title/Abstract] OR “elderly”[Title/Abstract] OR “older adults”[Title/Abstract] OR “seniors”[Title/Abstract] OR “geriatrics”[Title/Abstract] OR “gerontology”[Title/Abstract] OR “advanced age”[Title/Abstract] OR “aged population”[Title/Abstract] OR “older individuals”[Title/Abstract]) AND (“gait”[Title/Abstract] OR “walking”[Title/Abstract] OR “locomotion”[Title/Abstract] OR “gait analysis”[Title/Abstract] OR “walking pattern”[Title/Abstract] OR “gait parameters”[Title/Abstract] OR “walking parameters”[Title/Abstract] OR “gait assessment”[Title/Abstract] OR “gait abnormalities”[Title/Abstract] OR “step length”[Title/Abstract] OR “stride length”[Title/Abstract] OR “step width”[Title/Abstract] OR “foot angle”[Title/Abstract] OR “toe out angle”[Title/Abstract] OR “cadence”[Title/Abstract] OR “walking speed”[Title/Abstract] OR “cycle time”[Title/Abstract] OR “stride time”[Title/Abstract] OR “step time”[Title/Abstract] OR “stance time”[Title/Abstract] OR “swing time”[Title/Abstract] OR “single support time”[Title/Abstract] OR “double support time”[Title/Abstract] OR “joint angles”[Title/Abstract] OR “pelvic tilt”[Title/Abstract] OR “trunk movement”[Title/Abstract] OR “ground reaction forces”[Title/Abstract] OR “joint moments”[Title/Abstract] OR “joint power”[Title/Abstract] OR “Timed Up and Go Test”[Title/Abstract] OR “TUG”[Title/Abstract] OR “6-Minute Walk Test”[Title/Abstract] OR “6MWT”[Title/Abstract] OR “10-Meter Walk Test”[Title/Abstract] OR “10MWT”[Title/Abstract] OR “kinetic”[Title/Abstract] OR “kinematic”[Title/Abstract] OR “motion capture”[Title/Abstract] OR “optoelectronic motion capture”[Title/Abstract] OR “Vicon system”[Title/Abstract] OR “Qualisys”[Title/Abstract] OR “inertial measurement units”[Title/Abstract] OR “IMU sensors”[Title/Abstract] OR “Xsens”[Title/Abstract] OR “Delsys Trigno”[Title/Abstract] OR “force plates”[Title/Abstract] OR “Kistler force plate”[Title/Abstract] OR “pressure mats”[Title/Abstract] OR “Tekscan”[Title/Abstract]) | 175 |
| 2 | Scopus | (TITLE-ABS-KEY (kyphosis OR hyperkyphosis OR “flexed posture” OR “spinal kyphosis” OR “thoracic kyphosis” OR “excessive kyphosis” OR “kyphotic posture” OR “dowager's hump” OR hunchback) AND TITLE-ABS-KEY (aging OR elderly OR “older adults” OR seniors OR geriatrics OR gerontology OR “advanced age” OR “aged population” OR “older individuals”) AND TITLE-ABS-KEY (gait OR walking OR locomotion OR “gait analysis” OR “walking pattern” OR “gait parameters” OR “walking parameters” OR “gait assessment” OR “gait abnormalities” OR “step length” OR “stride length” OR “step width” OR “foot angle” OR “toe out angle” OR cadence OR “walking speed” OR “cycle time” OR “stride time” OR “step time” OR “stance time” OR “swing time” OR “single support time” OR “double support time” OR “joint angles” OR “pelvic tilt” OR “trunk movement” OR “ground reaction forces” OR “joint moments” OR “joint power” OR “timed up and go test” OR tug OR “6-minute walk test” OR 6mwt OR “10-meter walk test” OR 10mwt OR kinetic OR kinematic OR “motion capture” OR “optoelectronic motion capture” OR “vicon system” OR qualisys OR “inertial measurement units” OR “imu sensors” OR xsens OR “delsys trigno” OR “force plates” OR “kistler force plate” OR “pressure mats” OR tekscan)) | 478 |
| 3 | Web of Science | TS = (kyphosis OR hyperkyphosis OR “flexed posture” OR “spinal kyphosis” OR “thoracic kyphosis” OR “excessive kyphosis” OR “kyphotic posture” OR “dowager's hump” OR hunchback) AND TS = (aging OR elderly OR “older adults” OR seniors OR geriatrics OR gerontology OR “advanced age” OR “aged population” OR “older individuals”) AND TS = (gait OR walking OR locomotion OR “gait analysis” OR “walking pattern” OR “gait parameters” OR “walking parameters” OR “gait assessment” OR “gait abnormalities” OR “step length” OR “stride length” OR “step width” OR “foot angle” OR “toe out angle” OR cadence OR “walking speed” OR “cycle time” OR “stride time” OR “step time” OR “stance time” OR “swing time” OR “single support time” OR “double support time” OR “joint angles” OR “pelvic tilt” OR “trunk movement” OR “ground reaction forces” OR “joint moments” OR “joint power” OR “Timed Up and Go Test” OR TUG OR “6-Minute Walk Test” OR 6MWT OR “10-Meter Walk Test” OR 10MWT OR kinetic OR kinematic OR “motion capture” OR “optoelectronic motion capture” OR “Vicon system” OR Qualisys OR “inertial measurement units” OR “IMU sensors” OR Xsens OR “Delsys Trigno” OR “force plates” OR “Kistler force plate” OR “pressure mats” OR Tekscan) |
786 |
| 4 | CINAHL | ((“kyphosis” OR “hyperkyphosis” OR “flexed posture” OR “spinal kyphosis” OR “thoracic kyphosis” OR “excessive kyphosis” OR “kyphotic posture” OR “dowager's hump” OR “hunchback”) AND (“aging” OR “elderly” OR “older adults” OR “seniors” OR “geriatrics” OR “gerontology” OR “advanced age” OR “aged population” OR “older individuals”) AND (“gait” OR “walking” OR “locomotion” OR “gait analysis” OR “walking pattern” OR “gait parameters” OR “walking parameters” OR “gait assessment” OR “gait abnormalities” OR “step length” OR “stride length” OR “step width” OR “foot angle” OR “toe out angle” OR “cadence” OR “walking speed” OR “cycle time” OR “stride time” OR “step time” OR “stance time” OR “swing time” OR “single support time” OR “double support time” OR “joint angles” OR “pelvic tilt” OR “trunk movement” OR “ground reaction forces” OR “joint moments” OR “joint power” OR “Timed Up and Go Test” OR “TUG” OR “6-Minute Walk Test” OR “6MWT” OR “10-Meter Walk Test” OR “10MWT” OR “kinetic” OR “kinematic” OR “motion capture” OR “optoelectronic motion capture” OR “Vicon system” OR “Qualisys” OR “inertial measurement units” OR “IMU sensors” OR “Xsens” OR “Delsys Trigno” OR “force plates” OR “Kistler force plate” OR “pressure mats” OR “Tekscan”)) |
136 |
| 5 | Cochrane library | (((TI “kyphosis” OR TI “hyperkyphosis” OR TI “flexed posture” OR TI “spinal kyphosis” OR TI “thoracic kyphosis” OR TI “excessive kyphosis” OR TI “kyphotic posture” OR TI “dowager's hump” OR TI “hunchback”) OR (AB “kyphosis” OR AB “hyperkyphosis” OR AB “flexed posture” OR AB “spinal kyphosis” OR AB “thoracic kyphosis” OR AB “excessive kyphosis” OR AB “kyphotic posture” OR AB “dowager's hump” OR AB “hunchback”)) AND ((TI “aging” OR TI “elderly” OR TI “older adults” OR TI “seniors” OR TI “geriatrics” OR TI “gerontology” OR TI “advanced age” OR TI “aged population” OR TI “older individuals”) OR (AB “aging” OR AB “elderly” OR AB “older adults” OR AB “seniors” OR AB “geriatrics” OR AB “gerontology” OR AB “advanced age” OR AB “aged population” OR AB “older individuals”)) AND ((TI “gait” OR TI “walking” OR TI “locomotion” OR TI “gait analysis” OR TI “walking pattern” OR TI “gait parameters” OR TI “walking parameters” OR TI “gait assessment” OR TI “gait abnormalities” OR TI “step length” OR TI “stride length” OR TI “step width” OR TI “foot angle” OR TI “toe out angle” OR TI “cadence” OR TI “walking speed” OR TI “cycle time” OR TI “stride time” OR TI “step time” OR TI “stance time” OR TI “swing time” OR TI “single support time” OR TI “double support time” OR TI “joint angles” OR TI “pelvic tilt” OR TI “trunk movement” OR TI “ground reaction forces” OR TI “joint moments” OR TI “joint power” OR TI “Timed Up and Go Test” OR TI “TUG” OR TI “6-Minute Walk Test” OR TI “6MWT” OR TI “10-Meter Walk Test” OR TI “10MWT” OR TI “kinetic” OR TI “kinematic” OR TI “motion capture” OR TI “optoelectronic motion capture” OR TI “Vicon system” OR TI “Qualisys” OR TI “inertial measurement units” OR TI “IMU sensors” OR TI “Xsens” OR TI “Delsys Trigno” OR TI “force plates” OR TI “Kistler force plate” OR TI “pressure mats” OR TI “Tekscan”) OR (AB “gait” OR AB “walking” OR AB “locomotion” OR AB “gait analysis” OR AB “walking pattern” OR AB “gait parameters” OR AB “walking parameters” OR AB “gait assessment” OR AB “gait abnormalities” OR AB “step length” OR AB “stride length” OR AB “step width” OR AB “foot angle” OR AB “toe out angle” OR AB “cadence” OR AB “walking speed” OR AB “cycle time” OR AB “stride time” OR AB “step time” OR AB “stance time” OR AB “swing time” OR AB “single support time” OR AB “double support time” OR AB “joint angles” OR AB “pelvic tilt” OR AB “trunk movement” OR AB “ground reaction forces” OR AB “joint moments” OR AB “joint power” OR AB “Timed Up and Go Test” OR AB “TUG” OR AB “6-Minute Walk Test” OR AB “6MWT” OR AB “10-Meter Walk Test” OR AB “10MWT” OR AB “kinetic” OR AB “kinematic” OR AB “motion capture” OR AB “optoelectronic motion capture” OR AB “Vicon system” OR AB “Qualisys” OR AB “inertial measurement units” OR AB “IMU sensors” OR AB “Xsens” OR AB “Delsys Trigno” OR AB “force plates” OR AB “Kistler force plate” OR AB “pressure mats” OR AB “Tekscan”)) |
76 |
2.4 Study Selection
The study selection process began with thoroughly screening all identified articles based on their titles and abstracts to determine their relevance to the review topic. This initial assessment was carried out by two independent reviewers, Z. G. and M. A., to reduce bias and ensure a detailed evaluation. Subsequently, the full texts of studies considered potentially eligible were carefully examined against the established eligibility criteria. Any disagreements between the reviewers about whether to include or exclude specific studies were resolved through open discussions and consensus.
2.5 Data Extraction
Data extraction was performed systematically using a standardized form to ensure consistency and accuracy. Two independent reviewers, Z. G. and M. A., extracted essential information from the included studies, focusing on participant demographics, measures of kyphosis, and gait parameters. Discrepancies between reviewers were resolved through discussion and consensus. The summarized data are presented in Table 2, offering a concise overview of the findings from each study.
| No. | Author | Study design | Follow-up period | Aim | Participant | Mean of age | Threshold for hyperkyphosis | Kyphosis measurement tools | Measured relevant conditions | Gait measurement tool | Clinical or laboratory method | Gait parameters measured | Result | Total score of the STROBE checklist |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sakamitsu et al. 2007 [9] | Cross sectional | — | To examine how the degree of kyphotic spinal deformity affects balance and walking ability in elderly individuals. | 28 (5 males, 23 females) | 78.2 ± 5.2 years (Males: 75.8 ± 4.3 years; Females: 78.7 ± 5.3 years) | — | Spinal Mouse (Idiag AG, Switzerland) | Height, weight, BMI, primary diagnoses (degenerative spinal disease, knee osteoarthritis, cervical spondylotic myelopathy). | Stopwatch (for 10-meter walking time and 3-minute walking distance) | Clinical | Walking speed (10-meter walking time), Temporal walking endurance (3-minute walking distance) Functional |
The results revealed significant correlations between kyphosis and gait parameters. Specifically, a positive correlation was found between kyphosis angles (overall inclination angle and thoracolumbar angle) and 10-meter walking time (r = 0.69 and r = 0.68, respectively). Conversely, a negative correlation was observed between kyphosis and 3-minute walking distance (r = −0.55 for overall inclination angle and r = −0.69 for thoracolumbar angle). Overall, greater kyphotic deformity was associated with slower walking speed and reduced endurance. | 17/22 |
| 2 | Kurokawa et al. 2010 [10] | Cross sectional | — | To analyze the gait characteristics of elderly individuals with kyphosis using kinematic and kinetic data, and compare these results with healthy elderly individuals. | 24 (13 males and 11 females) | 69.6 ± 5.8 years | — | Flexible ruler (C7 to L4) | Height, weight, no history of orthopedic or central nervous system disorders | 3D motion analysis system (VICON) with 12 infrared cameras and 6 force plates (AMTI) | Laboratory | Joint angles in the lower limbs (hip, knee, ankle) and trunk Kinematic, Joint moments (hip flexion/extension, knee flexion/extension, ankle plantar flexion) and ground reaction forces Kinetic |
No significant differences between the kyphotic and healthy groups in terms of walking speed, cadence, stride length, or stance time. The kyphotic group demonstrated significantly larger hip extension moments during the early stance phase, as well as increased pelvic rotation and posterior pelvic tilt during the gait cycle. Peak joint moment waveforms differed, showing larger peaks in lower limb joint moments in the kyphotic group. |
16/22 |
| 3 | Katzman et al. 2011 [11] | Cohort | 4.4 years | To determine whether increasing kyphosis angle was independently associated with poorer mobility as measured by the (TUG), after controlling for other risk factors. | 2777 females | 68.2 ± 6 years | — | Debrunner Kyphometer | Age, body mass index (BMI), self-reported health status, grip strength, change in total hip bone mineral density (BMD), and the number of vertebral fractures | Stopwatch (For Timed Up and Go Test (TUG)) | Clinical | Walking Speed Temporal and Mobility Functional |
The mean change in kyphosis angle was 3.9 ± 8.6° over 4 years. There was a significant association where for every 5° increase in kyphosis, TUG performance times increased by 0.02 s (p < 0.001). | 20/22 |
| 4 | Katzma et al. 2011 [12] | Cross sectional | — | To assess the association between kyphosis and mobility TUG test independent of osteoporosis | 3108 females | 68.2 years | Kyphosis angle ≥ 47.6°. | Debrunner Kyphometer | Age, height, weight, BMI, grip strength, hip BMD, vertebral fractures, smoking status | Stopwatch (For TUG) | Clinical | Walking Speed Temporal and Mobility Functional |
For each standard deviation (11.9°) increase in kyphosis, there was an increase of 0.11 s in TUG time (p = 0.02) after adjusting for confounders like age, BMI, grip strength, vertebral fractures, and total hip BMD. Kyphosis was an independent contributor to decreased mobility, with higher kyphosis angles correlated with slower TUG performance times. | 22/22 |
| 5 | Pimentel et al. 2011 [13] | Cross sectional | — | To compare the degree of thoracic kyphosis, respiratory muscle strength, and functional capacity in elderly women with and without osteoporosis. | 30 females | 66.8 ± 5.5 years | > 37.1° for hyperkyphosis. | Computer assisted photogrammetry (AUTOCAD-R14) | Height, weight, MIP, MEP, physical activity levels, TUG, 6-MWT | Stopwatch (For TUG, 6-Minute Walk Test [6-MWT]) | Clinical | Walking Speed Temporal and Mobility Functional, Walking endurance Functional |
No significant difference in TUG performance between women with and without osteoporosis. Significant difference in 6-MWT performance, with osteoporotic women covering a shorter distance, indicating reduced cardiorespiratory capacity in this group. |
20/22 |
| 6 | Eum et al. 2013 [14] | Cross sectional | 18 months | To determine the association of increased kyphosis with declines in mobility, balance, and disability among community-living older adults. | 620 | 79.2 ± 5.4 years | — | flexicurve ruler | Age, gender, race, education, body mass index (BMI), self-rated health, comorbidities (heart disease, diabetes, stroke), pain (back and knee), and falls self-efficacy. | Stopwatch (For Short Physical Performance Battery (SPPB)) | Clinical | Walking Speed Temporal and Mobility Functional |
Greater kyphosis was significantly associated with lower SPPB scores in women (β = −0.09, p = 0.01), while no significant associations were found with balance (BBS) or self-reported disability. | 19/22 |
| 7 | Katzman et al. 2013[16] | Cohort | 15 years | To assess whether greater magnitudes of kyphosis are associated with declines in self-reported and objectively measured physical function over time in older women. | 1072 females | 69.3 ± 4 years | Cobb angle of ≥ 50°. | Cobb angle | Age, race, education level, overall health status, and medical history, Health behaviors, anthropometric measures, bone health. | Stopwatch (For 6-meter walking test) | Clinical | Walking Speed Temporal |
In multivariate analyses, each 10° increment of kyphosis was associated with: 0.01 m/s additional decline in gait speed (p = 0.07). A significant increase of 0.32 s in the time taken to complete five chair stands (p = 0.004). | 20/22 |
| 8 | Katzman et al. 2015 [15] | Cross sectional | — | To investigate the relationship between hyperkyphosis and physical function in older men. | 2363 males |
79 years | ≥ 4 blocks. | block method | Height, weight, bone mineral density, ankle brachial index | Stopwatch (For 6-MWT) | Clinical | Walking Speed Temporal and Walking endurance Functional |
Men with hyperkyphosis demonstrated a 1.8-fold increased likelihood of being in the lowest quartile for walking speed, highlighting a significant association between hyperkyphosis and impaired lower extremity physical function. | 22/22 |
| 9 | Alin et al. 2016 [18] | Cross sectional | — | To investigate the relationship between spinal curvature (specifically thoracic kyphosis and lumbar lordosis) and balance performance in elderly women at high risk of osteoporotic fractures. | 94 females | 85 years | Kyphotic Index (KI) ≥ 13. | Flexicurve ruler | Height in young adulthood and current height (to calculate height loss), Bone density (via Hologic 4500 scanner), Downton Fall Risk Index (DFRI) scores, History of fractures, physical activity levels, and medication | Stopwatch (For Timed Gait Speed Tests) | Clinical | Walking Speed Temporal |
The study found that women with hyperkyphosis exhibited improved performance in gait tests. Specifically, these women were more likely to complete a greater number of tandem steps, suggesting that hyperkyphosis may affect gait through compensatory mechanisms related to spinal curvature. | 19/22 |
| 10 | Lorbergs et al. 2017 [6] | Cohort | 3.4 years | To evaluate the association between thoracic kyphosis and physical function. | 1100 (604 females, 496 males) | 61 years | — | Cobb angle | Age, height, weight, smoking, follow-up time, vertebral fractures, prevalent spinal degeneration, quick walking speed, chair-stand time, grip strength, self-reported impairments. | Stopwatch (For Quick walking speed) | Clinical | Walking Speed Temporal |
Thoracic kyphosis was not associated with physical function in women or men, even in those aged 65 and older. There were no significant differences in walking speed, grip strength, chair stand time, or self-reported physical impairment between individuals with and without severe kyphosis. | 22/22 |
| 11 | Demarteau et al. 2019 [19] | Cross sectional | — | To investigate the relationship between spinal posture and mobility with 3D-accelerometry-based gait analysis, functional performance, and fall-risk in aging adults. | 121 | 60.43 | > 40° for hyperkyphosis | SpinalMouse® (Idiag, Fehraltorf, Switzerland). | Height and weight, Muscle performance, History of falls, |
DynaPort MiniMod (3D piezoresistive accelerometer). | Clinical | Walking speed, step time asymmetry Temporal, cranio-caudal step/stride regularity, medio-lateral step and stride regularity Spatial |
The study found that participants in the increased fall-risk group (OFR) exhibited significantly slower walking speeds and lower step and stride regularity compared to controls. Increased trunk inclination and decreased sacral extension mobility were correlated with worse gait performance, and these factors served as predictors of fall-risk in older adults. | 20/22 |
| 12 | Kamata et al. 2019 [20] | Cross sectional | — | To examine the spino-pelvic-lower extremity alignment during walking in patients with spinal kyphosis and clarify factors influencing trunk anterior inclination. | 26 (21 females, 5 males) | 66 years | — | Cobb angle | Height, weight, Trunk Tilting Angle, Sacral Slope (SS), Lumbar Lordosis (LL) | A 3D motion capture system (MAC3D system; Motion Analysis Corporation) | Laboratory | Trunk and pelvic anterior inclination angles, hip joint angle, and knee joint angle Kinematic |
The change in the trunk anterior inclination angle during the 3-minute walking session ranged from −1.7° to 19.7°, with a median increase of 5.4°. Two groups were identified: those with a significant change ( ≥ 5°) in trunk inclination and those with minimal change ( < 5°). Significant differences in pelvic anterior inclination angles were observed between these groups, with strong correlations between changes in trunk and pelvic inclination angles. | 20/22 |
| 13 | Sugai et al. 2019 [21] | Cohort | 4 years | To investigate the association between muscle strength, mobility, and the progression of hyperkyphosis in elderly individuals. | 403 (230 females, 173 males) | — | Number of blocks ≥ 3. | Block method | Handgrip strength, sex, age, marital status, educational background, smoking status, drinking status, history of life-threatening diseases, knee joint pain, back pain, predicted body mass index (pBMI), bone stiffness. | Stopwatch (For TUG) | Clinical | Walking Speed Temporal and Mobility Functional |
Low handgrip strength ( < 26 kg in men, < 18 kg in women) and low mobility ( > 13.5 s) were independently associated with kyphosis progression. These findings were consistent after adjusting for age, sex, baseline block number, bone stiffness, and other covariates. Kyphosis progression was more common in men, older participants, and those with more advanced kyphosis at baseline. Participants with weak handgrip strength or low mobility had a higher likelihood of kyphosis progression. |
19/22 |
| 14 | Kantha et al. 2021 [22] | Cross sectional | — | To investigate the relationship between body composition and balance performance in older adults with hyperkyphosis. | 30 (28 females, 2 males) | 66.9 ± 5.8 | > 40° for hyperkyphosis. | SpinalMouse | Body composition (BMC, muscle mass, BMI, fat mass). | Motion analysis system (VICON Bonita) | Laboratory | Walking Speed Temporal, Step Length Spatial, Center of Mass–Center of Pressure Inclination Angle Kinematic |
Bone mineral content (BMC) was positively correlated with gait speed and step length, while muscle mass was positively correlated with step length, inclination angle at heel strike (Inc-HS), and reaching distance. However, body mass index (BMI) and fat mass were not significantly associated with balance performance. These findings suggest that BMC and muscle mass are key factors influencing walking and reaching performance in older adults with hyperkyphosis. | |
| 15 | Li et al. 2021 [17] | Cross sectional | — | To investigate the prevalence and effects of thoracic hyperkyphosis on physical performance in Chinese community-dwelling older adults. | 395 (307 females, 88 males) | 68.6 years | > 40° for hyperkyphosis. | Manual inclinometer | Age, gender, marital status, education level, health-related information (spine surgery history, chronic illnesses, daily exercise intensity, BMI) | Stopwatch (For 6MWT, Farsi Version of Functional Gait Assessment (FGA) |
Clinical | Walking Speed Temporal and Walking endurance Functional, Mobility Functional |
Thoracic hyperkyphosis is highly prevalent among Chinese community-dwelling older adults and is associated with impaired balance, gait, and cardiopulmonary function. | 22/22 |
| 16 | Fukuoka et al. 2022 [23] | Cross sectional | — | To determine whether hyperkyphosis and upper extremity tasks were independently associated with the 6MWT in community. | 99 (71 females, 28 males) | 70.1 ± 6.1 years | Cobb angle of ≥ 50°. | Cobb angle | Age, height, weight, BMI, vertebral fractures | Stopwatch (For 6MWT) | Clinical | Walking Speed Temporal and Walking endurance Functional |
Upper extremity function, as assessed by the book lift task, was a significant predictor of 6MWT performance in older adults with hyperkyphosis. Additionally, sociodemographic factors (age, height) and the number of prescribed medications were contributing factors. However, no significant association was found between the Cobb angle of kyphosis and 6MWT distance. These findings highlight the multifactorial influences on physical performance in older adults with hyperkyphosis. | 18/22 |
| 17 | Fukuoka et al. 2022 [24] | Cross sectional | — | To investigate the relationship between the severity of hyperkyphosis and 6MWT distance in older adults. | 112 (67 females, 45 males) | 69.8 ± 6.3 years | Cobb angle of ≥ 40°. | Cobb angle | Age, height, weight, BMI, vertebral fractures, number of prescribed medications | Stopwatch (For 6MWT) | Clinical | Walking Speed Temporal and Walking endurance Functional |
No significant association was found between kyphosis (Cobb angle) and 6MWT distance. However, height, weight, and medication use were significant predictors of 6MWT performance, with taller height, lower weight, and fewer medications linked to better outcomes. This highlights the multifactorial influences on physical function in older adults with hyperkyphosis. | 19/22 |
| 18 | Koel et al. 2022 [25] | Cohort | 2 years | To investigate the association between kyphosis angle and physical performance in older adults. | 1220 (720 females, 500 males) | 72.9 ± 5.7 years | Cobb angle of ≥ 50°. | Cobb angle | Age, sex, education, alcohol intake, smoking, fractures, osteoporosis, vitamin D, physical activity, balance, hand grip strength, Mini-Mental State Examination (MMSE), Geriatric Depression Scale (GDS) | Stopwatch | Clinical | Walking Speed Temporal |
A larger kyphosis angle was independently associated with poorer physical performance, particularly in women aged 77 and older, with a stronger effect on balance and muscle strength than gait speed. The relationship was unidirectional, and physical activity did not mediate this association. Early detection and treatment may help preserve physical function in this population. | 20/22 |
| 19 | Amatachaya et al. 2023 [26] | Cross sectional | — | To explore the ability of C7 wall distance (C7WD) to indicate mobility deficits in older adults with thoracic hyperkyphosis. | 104 | 74.1 ± 7.4 years | Cobb angle of ≥ 40°. | Cobb angle and C7 wall distance (C7WD) | Age, sex, education, alcohol intake, smoking | Stopwatch (For TUG, 10-Meter Walk Test (10MWT), 6MWT) |
Clinical | Walking Speed Temporal and Mobility Functional, Walking endurance Functional |
Participants with thoracic hyperkyphosis had significantly poorer mobility. A C7WD ≥ 7.8 cm predicted mobility deficits with high sensitivity (71%–92%), specificity (75%–94%), and area under the curve ( > 0.80). C7WD is a reliable, noninvasive marker for detecting mobility impairments in older adults with thoracic hyperkyphosis. | 21/22 |
2.6 Tool and Procedure for Risk-of-Bias Assessment
For this systematic review, the methodological quality and risk of bias of the included observational studies were assessed using the Joanna Briggs Institute (JBI) Critical Appraisal Tools. Separate checklists were applied for cohort and cross-sectional studies. The JBI Checklist for Cohort Studies consists of 11 items, while the JBI Checklist for Cross-Sectional Studies includes 8 items. Two independent reviewers (Z. G. and M. A.) conducted the quality assessments, scoring each item as either 1 (met) or 0 (not met).
The total score for each study was calculated as a percentage of the maximum possible score. Studies were categorized into three quality levels: high quality ( ≥ 75% of criteria met), moderate quality (50%–74% of criteria met), and low quality ( < 50% of criteria met). By PRISMA guidelines and the Cochrane Handbook, no studies were excluded based on quality scores; all studies—regardless of quality—were retained for qualitative synthesis [18]. Any discrepancies between the reviewers were resolved through discussion to reach a consensus. This process ensured a rigorous and transparent evaluation, emphasizing key methodological factors such as sample representativeness, measurement validity, and statistical analysis.
2.7 Ethical Considerations
This systematic review synthesizes data exclusively from previously published studies and does not require separate ethical approval by international guidelines for secondary research [19]. The study adhered to the PRISMA 2020 statement to ensure methodological transparency and rigor [20]. While no ethical approval code was issued by the Ethical Committee of the University of Social Welfare and Rehabilitation Sciences, all included studies were required to have obtained ethical clearance and informed consent in their original research. Academic integrity was maintained through proper citation practices and plagiarism checks, aligning with established norms for systematic reviews [19, 20].
2.8 Synthesis of Results
The results of the included studies were synthesized qualitatively, focusing on the main outcomes of interest, such as gait parameters, the severity of hyperkyphosis, and their relationship in older adults. These outcomes were compared across the studies to identify patterns and variations. The data were categorized based on the study design and the type of gait assessment (clinical vs. laboratory-based), allowing for a structured comparison of the findings. Key results were summarized in tables (Table 2) to provide an overview of the study characteristics and findings, facilitating an overall understanding of the effects of hyperkyphosis on gait in this population.
3 Results
3.1 Study Selection
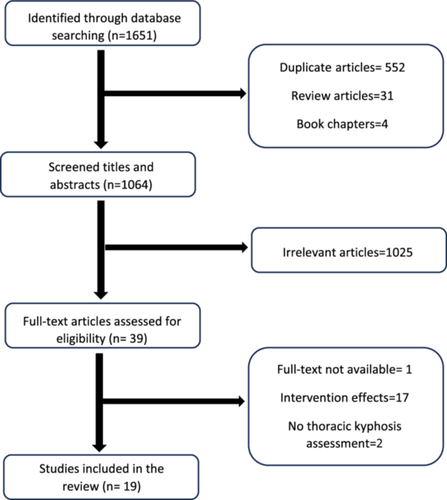
The study selection process involved a systematic search using keywords across five databases, yielding a total of 1551 articles. After removing 552 duplicates, 31 review articles, and 4 book chapters, the titles and abstracts of the remaining articles were screened for relevance based on predefined criteria, which resulted in the exclusion of 1025 articles. Subsequently, 39 articles were selected for full-text assessment. Notably, two studies were originally published in Japanese, one in German, and one in Portuguese. These non-English articles were initially translated into English using Google Translate, and the respective language expert subsequently confirmed their accuracy and clarity. After careful evaluation, 19 studies were included in the final analysis. This selection process is visually represented in the PRISMA flow diagram (Figure 1).
3.2 Study Characteristics
A total of 19 studies were included in the systematic review, comprising a mix of cross-sectional and cohort designs. All studies focused on older adults aged 60 years and above with a diagnosis of hyperkyphosis. The key outcomes assessed included gait parameters and the severity of hyperkyphosis. A summary of the studies, including sample sizes and main findings, is provided in Table 2.
3.3 Tool and Procedure for Risk-of-Bias Assessment
The methodological quality assessment using the JBI Critical Appraisal Tools revealed variations in study quality. Among the five cohort studies, scores ranged from 8/11 to 10/11 (73%–91%). No studies were excluded due to low quality, as per PRISMA principles; however, all included studies met at least moderate quality thresholds [18]. One study was rated as high quality [16], while the remaining four were classified as moderate quality [6, 11, 22, 26]. The most common limitations were incomplete adjustment for confounders (Item 6), as none of the studies adequately controlled for variables such as comorbidities, physical activity, or medications affecting balance and walking. Additionally, four of the five studies had insufficient reporting on follow-up completeness (Items 9 and 10), with missing details on participant retention, reasons for attrition, and handling of missing data [6, 11, 22, 26]. These gaps limit the ability to assess long-term functional decline and kyphosis progression. Detailed quality assessment results for cohort studies are presented in Table 3.
| No. | Author's name and year | JBI checklist items for cohort studies | Overall score | Comments | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||||
| 1 | Katzman et al. 2011 [11] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | 8 (72.7%) Moderate quality | Lack of baseline mobility status confirmation, Unreported reasons for 13% attrition, Missing data exclusion without imputation. |
| 2 | Katzman et al. 2013 [16] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | 10 (90.9%) High quality | No confirmation of participants' baseline physical function. |
| 3 | Lorbergs et al. 2017 [6] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | 8 (72.7%) Moderate quality | No confirmation of participants' baseline physical function, Loss to follow-up details were not provided, 3.4 years may be insufficient to detect long-term functional decline. |
| 4 | Sugai et al. 2019 [26] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | 8 (72.7%) Moderate quality | Participants with severe kyphosis included; no confirmation of absence of progression at baseline, 4 years may not capture long-term kyphosis progression. |
| 5 | Koel et al. 2022 [27] | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | 8 (72.7%) Moderate quality | No confirmation of absence of physical performance decline at baseline, 2 years may not capture long-term kyphosis progression or physical decline. |
Among the 14 cross-sectional studies, scores ranged from 5/8 to 8/8 (63%–100%) [9, 10, 12-15, 21, 23-29]. Twelve studies were rated as high quality [9, 10, 12-15, 21, 23, 25, 27-29], while two were of moderate quality [10, 26]. The primary methodological issues included inadequate justification for sample size (Item 5) in five studies [9, 10, 21, 24, 28] and unclear statistical methods (Item 6) in seven studies [9, 10, 13, 21, 26-28]. Some studies lacked detailed inclusion/exclusion criteria, failed to report demographic diversity, or did not confirm participants' baseline physical function. Furthermore, in several cases, statistical analyses relied solely on group comparisons without applying multivariable adjustments to control for potential confounders. These methodological limitations may affect the generalizability and validity of the findings. A detailed summary of the quality assessment for cross-sectional studies is provided in Table 4.
| No. | Author's name and year | JBI checklist items for cross-sectional studies | Overall score | Comments | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||||
| 1 | Sakamitsu et al. 2007 [9] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | 6 (75%) High quality | No adjustment for comorbidities, physical activity, or medications affecting balance/walking. |
| 2 | Kurokawa et al. 2010 [10] | Yes | No | Yes | Yes | No | No | Yes | Yes | 5 (62.5%) Moderate quality | Missing details on inclusion/exclusion criteria and demographic diversity, No adjustment for BMI, physical activity, or comorbidities affecting gait. |
| 3 | Katzman et al. 2011 [12] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 4 | Pimentel et al. 2011 [13] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 7 (87.5%) High quality | No advanced strategies (e.g., multivariate analyses) were employed to control for potential confounding factors. |
| 5 | Eum et al. 2013 [14] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 6 | Katzman et al. 2015 [15] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 7 | Alin et al. 2016 [29] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | 7 (87.5%) High quality | While potential confounders were identified and measured, the study did not clearly state or implement strategies (e.g., multivariable adjustments) to control for these confounders in the analysis. |
| 8 | Demarteau et al. 2019 [28] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 9 | Kamata et al. 2019 [21] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | 6 (75%) High quality | Confounding factors (e.g., age, gender, comorbidities) were not identified or adjusted for; analyses relied solely on group comparisons and correlations without multivariable control. |
| 10 | Kantha et al. 2021 [25] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | 6 (75%) High quality | The study did not clearly identify potential confounding factors, nor did it state any strategies (e.g., multivariate analysis) to control for them. |
| 11 | Li et al. 2021 [24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 12 | Fukuoka et al. 2022 [20] | Yes | Yes | Yes | Yes | No | No | Yes | No | 5 (62.5%) Moderate quality | Adjusted for age, height, medication, and upper extremity function; lacked adjustment for comorbidities and physical activity. Used multivariate regression but omitted effect sizes and CIs. Missing data handling not reported; assumed complete case analysis without sensitivity analysis. |
| 13 | Fukuoka et al. 2022 [23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
| 14 | Amatachaya et al. 2023 [22] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8 (100%) High quality | |
3.4 Main Outcomes
3.4.1 Hyperkyphosis: Measurement Tools and Thresholds
In the studies included in this review, kyphosis angle measurement methods were categorized into two groups: laboratory-based and clinical methods. The gold standard for kyphosis assessment is the Cobb angle derived from radiographic imaging, which was utilized in seven studies [6, 16, 23, 24, 26, 28, 30]. The Cobb angle is measured by drawing intersecting lines along the superior and inferior endplates of the vertebrae encompassing the kyphotic curve; the angle formed by these lines reflects the degree of spinal curvature. Among these studies, three established a hyperkyphosis threshold at an angle greater than 50° [16, 26, 30], while two studies defined hyperkyphosis as exceeding 40° [23, 24].
In the remaining studies, several clinical measurement methods were employed. Three studies utilized the Spinal Mouse, a noninvasive device that objectively tracks spinal curvature by rolling along the surface of the spine [9, 21, 29]. Two of these studies set the hyperkyphosis threshold at angles exceeding 40° [21, 29]. Additionally, three studies employed the Flexicurve Ruler, a flexible tool that conforms to the spine's shape to trace the kyphotic curve. This curve is used to calculate the Kyphotic Index, which represents the ratio of the height of the curve to its length [10, 14, 27]. One study utilizing the Flexicurve defined hyperkyphosis with a Kyphotic Index greater than 13° [27]
Two studies used the Debrunner Kyphometer, a clinical instrument designed for direct measurement of kyphosis angles at specific vertebral points [11, 12]. One of these studies classified hyperkyphosis as an angle exceeding 47.6° [12]. Moreover, two studies applied the Block Method, which assesses kyphosis by measuring the number of blocks required to fill the space between the spine and a flat surface [15, 22]. One study defined hyperkyphosis as necessitating more than three blocks [22], while the other set the threshold at more than four blocks [15].
One study employed a Manual Inclinometer, a device that measures spinal curvature angles by placing it directly on the patient's back. This study established the threshold for hyperkyphosis at greater than 40° [25]. Another study utilized Computer-Assisted Photogrammetry, a technique that captures images of the spine for curvature analysis through specialized software, with a hyperkyphosis threshold set at 37.1° [13]. Finally, one study implemented the Wall Distance Test, which measures the distance between the wall and the patient's head while standing against the wall; hyperkyphosis was indicated when the occiput failed to contact the wall. Notably, this study combined the Wall Distance Test with Cobb angle measurements obtained through radiographic imaging, providing a comprehensive assessment of kyphotic severity [23].
These diverse methods underscore the range of approaches employed to assess kyphosis severity, reflecting varying thresholds for defining hyperkyphosis.
3.5 Measurement of Gait Parameters
In the 19 studies reviewed, gait data from a total of 13,726 participants were analyzed. The methods used to assess gait parameters in these studies can be broadly categorized into two groups: laboratory-based and clinical methods [31]. Laboratory methods, such as 3D motion analysis systems and force plates, provide highly accurate and detailed gait measurements [32], while clinical methods, including timed walking tests and performance-based assessments, offer more accessible but less precise measures [33].
3.5.1 Laboratory Methods for Assessing Gait Parameters
One of the key methods for assessing gait in the reviewed studies is using a 3D motion analysis system, which provides detailed kinematic and kinetic data. Two studies employed the VICON system, which uses 12 infrared cameras and 6 force plates (AMTI) with a sampling frequency of 120 Hz. According to Clinical Gait Analysis Research Society guidelines, infrared reflective markers were placed on 34 anatomical points. This setup allowed for the analysis of joint angles and moments in the lower limbs (hip, knee, ankle), trunk angles, and ground reaction forces during walking. Participants walked along a 10-m path at their self-selected speed, and steady-state gait cycles were analyzed [10, 21].
In the first study, kinetic and kinematic data, including joint angles and moments, were assessed. No significant differences were found between the hyperkyphotic and healthy groups in terms of walking speed, cadence, stride length, or stance time. However, the hyperkyphotic group demonstrated increased hip extension moments during the early stance phase and greater pelvic rotation and posterior pelvic tilt throughout the gait cycle, with larger joint moment peaks observed in the lower limb joints compared with the healthy group [10].
In the second study, similar gait parameters were measured, focusing on walking speed, step length, and the center of mass–center of pressure (COM-COP) inclination angle. The COM-COP inclination angle, an indicator of postural stability, represents the angle between the body's center of mass (COM) and the point of pressure exerted on the ground (center of pressure, COP) during walking or standing. This measure helps assess the body's alignment and balance, as a greater inclination angle may indicate a forward-leaning posture often observed in hyperkyphosis. Results showed a positive correlation between bone mineral content (BMC) and both gait speed and step length, while muscle mass was positively associated with step length, COM-COP inclination at heel strike, and reaching distance. In contrast, body mass index (BMI) and fat mass were not significantly linked to walking performance. These findings highlight the influence of BMC and muscle mass on gait and balance in older adults with hyperkyphosis [21].
Another study used a 3D motion capture system (MAC3D system; Motion Analysis Corporation), with markers placed on 21 anatomical landmarks. This study measured trunk and pelvic anterior inclination angles, hip joint angle, and knee joint angle during a 3-minute walking test on a 5-m walkway. It identified two groups: those with significant changes in trunk inclination ( ≥ 5°) and those with minimal changes ( < 5°). A strong correlation between trunk and pelvic anterior inclination was observed, suggesting that increased trunk inclination is a key feature of hyperkyphotic gait, with implications for balance and mobility [28].
3.5.2 Clinical Methods for Assessing Gait Parameters
Clinical methods for gait assessment are practical, accessible tools used to evaluate gait in older adults, particularly when advanced lab-based technologies are unavailable. These methods rely on standardized performance tests and functional assessments to provide insights into aspects like walking speed and mobility. Although less precise than lab-based systems, they are widely used due to their ease of application and cost-effectiveness, making them ideal for large-scale studies and routine clinical use [34].
In this review, 16 of 19 studies used clinical methods to assess gait in individuals with hyperkyphosis [6, 9, 11-16, 22-27, 29, 30]. These assessments typically measured five key gait parameters: Temporal, Spatial, Functional, Kinematic, and Kinetic parameters.
Temporal parameters: These involve the measurement of time-related aspects of gait, such as gait speed, cadence (steps per minute), stride time, and step time. Temporal measures provide insight into the rhythm and pace of walking, which hyperkyphosis can particularly affect [35].
Spatial parameters: These include variables like step length, stride length, and step width. Spatial measures capture the dimensions of an individual's gait pattern and can reflect balance and stability during walking [36].
Functional parameters: Functional assessments focus on the overall performance of gait and mobility, such as the ability to walk a certain distance or perform a task involving walking (e.g., the TUG test). These tests assess how gait affects daily life activities and are crucial for understanding functional limitations in individuals with hyperkyphosis [37].
Kinematic parameters: Kinematics refers to the body's motion during walking, such as joint angles and limb movements. Although typically measured more accurately in laboratory settings, clinical assessments may provide estimates of trunk, hip, knee, and ankle movements during gait [38].
Kinetic parameters: These refer to the forces generated during walking, such as ground reaction forces and joint moments. While kinetic measures are more challenging to capture in clinical settings, some functional tests and wearable sensors can indirectly assess kinetic changes in gait [38].
Overall, the studies examined primarily assessed temporal, spatial, and functional parameters, providing valuable insights into gait characteristics in individuals with hyperkyphosis.
3.5.2.1 Temporal Parameters
3.5.2.1.1 Speed of Walking
Speed of walking is a key gait parameter that indicates an individual's mobility and functional capacity. It is influenced by factors such as age and physical condition and provides insights into balance and fall risk, especially in older adults [5]. Generally, increased walking speed correlates with better mobility and independence, while reduced speed may indicate mobility issues or conditions like hyperkyphosis [39].
In the studies reviewed, 16 out of 19 studies employing clinical methods utilized both direct and indirect approaches to assess gait speed [6, 9, 11-16, 22-27, 29, 30]. The methods for measuring walking speed are summarized in Table 5. One study used a stopwatch to evaluate speed as participants walked as quickly as possible over a distance of 3 m back and forth. This direct measurement approach provided immediate feedback on walking performance [30].
| No. | Measurement method | Description | Type | Number of studies | References |
|---|---|---|---|---|---|
| 1 | 10 Meter Walking Time | Time taken to walk 10 meters. | Direct | 1 | [9] |
| 2 | 10 Meter Walking Test | Standard test to measure walking speed over 10 meters. | Direct | 1 | [22] |
| 3 | 6 Meter Walking Test | Time taken to walk 6 meters. | Direct | 1 | [16] |
| 4 | 6 Minute Walking Test | Distance covered in 6 minutes of walking. | Indirect | 6 | [13, 15, 20, 22-24] |
| 5 | 3 Minute Walking Distance | Distance covered in 3 minutes of walking. | Indirect | 1 | [9] |
| 6 | Timed Up and Go (TUG) | Time to rise, walk 3 meters, turn, walk back, and sit down. | Indirect | 5 | [11-13, 22, 26] |
| 7 | Short Physical Performance Battery | A series of tests including gait speed, balance, and strength assessments. | Direct/Indirect | 1 | [14] |
| 8 | Timed Gait Speed Test | Measures gait speed over a short, predetermined distance. | Direct | 1 | [29] |
| 9 | Quick Walking Speed | Evaluates walking speed during a short walk at a comfortable pace. | Direct | 1 | [6] |
| 10 | DynaPort MiniMod | Utilizes accelerometer data to assess gait speed and patterns. | Direct | 1 | [28] |
Additionally, six of the studies implemented the 6-Minute Walk Test (6MWT), which measures the distance an individual can walk in 6 min. This test assesses endurance and functional mobility, providing valuable information about walking speed over a longer duration [13, 15, 23-26].
Furthermore, five studies used the TUG test, which measures the time it takes for a participant to rise from a chair, walk 3 m, turn around, walk back, and sit down. The TUG test effectively assesses mobility and can indirectly indicate walking speed, particularly in older adults [11-13, 22, 23].
Collectively, results from various studies employing methods such as the 10-Meter Walking Test (10-MWT), Short Physical Performance Battery (SPPB), Timed Gait Speed, and DynaPort MiniMod indicated a relationship between increasing kyphosis and decreased walking speed [7, 9, 14, 15, 27, 29]. However, one study utilizing the 6-Meter Walking Test did not find this association [16]. Additionally, another study investigating quick walking speed found no correlation between kyphosis and walking speed, although a significant relationship was identified between advancing age and decreased walking speed [6].
3.5.2.1.2 Step Time
Step Time is a key temporal gait parameter that refers to the duration it takes for one foot to complete a step during walking [40]. It plays a crucial role in understanding gait rhythm and stability, as irregular step times can signal balance or coordination issues, particularly in older adults or individuals with musculoskeletal conditions like hyperkyphosis [39].
In one reviewed study, step time was assessed using a 3D piezoresistive accelerometer (DynaPort MiniMod) placed on the sacrum. Participants walked along an 18-m corridor, and the data were used to calculate gait parameters. The study results indicated that older adults with a more pronounced stooped posture exhibited shorter step times, reflecting compromised gait performance. Reduced spinal mobility, particularly lower sacral extension mobility, was significantly associated with shorter step times. These findings suggest that limited spinal flexibility negatively impacts step time, leading to decreased walking stability and potentially increasing the risk of falls [29].
3.5.2.2 Spatial Parameters
3.5.2.2.1 Cranio-Caudal Step/Stride
Cranio-caudal step/stride regularity refers to the consistency of vertical (head-to-tail) movement during walking. It is an important indicator of gait stability and coordination. Symmetry and regularity in cranio-caudal movement help ensure smooth and stable walking patterns, which are particularly crucial in older adults to reduce the risk of falls. When this regularity is disrupted, it may indicate balance or coordination issues [41].
In one of the reviewed studies using the DynaPort MiniMod accelerometer, cranio-caudal step/stride regularity was assessed. The results showed that elderly participants with hyperkyphosis had significantly worse cranio-caudal step/stride regularity, reflecting compromised gait stability. Reduced sacral extension mobility was also strongly related to poorer regularity, which further indicates a negative impact on walking stability [29].
3.5.2.2.2 Medio-Lateral Step/Stride
Medio-lateral step/stride regularity refers to the consistency of lateral (side-to-side) movement during walking. This parameter is critical for assessing gait stability and balance, especially in older adults. Irregularities in medio-lateral movement can indicate potential issues with coordination or balance, which may increase the risk of falls [42].
In a study utilizing the DynaPort MiniMod accelerometer to evaluate this parameter, results showed that older adults with hyperkyphosis had significantly lower medio-lateral step and stride regularity [29]. This reduced regularity is associated with compromised mobility and balance. The findings indicate that limited lateral stability in individuals with hyperkyphosis can negatively impact their overall gait performance, contributing to an increased risk of falls. Furthermore, the study highlighted that lower medio-lateral regularity was correlated with decreased performance in various gait features and physical activities, emphasizing the importance of maintaining spinal and postural health to support gait stability [29].
3.5.2.3 Functional Parameters
3.5.2.3.1 Endurance
Endurance in the context of gait refers to an individual's ability to sustain physical activity over an extended period. It is a crucial aspect of functional mobility, especially in older adults, as it directly impacts their independence and overall quality of life [43].
A commonly used measure to assess endurance is the 6MWT, which evaluates the distance an individual can walk in 6 min. This test provides insights into cardiovascular fitness, muscular strength, and overall endurance. It is particularly valuable in clinical settings for monitoring changes in an individual's functional status over time. In the studies reviewed, six of them utilized the 6MWT to assess endurance among participants [13, 15, 23-26]. Additionally, one study employed the 3-Minute Walking Distance Test, which assesses the distance walked in 3 min and serves as a quicker alternative to the 6MWT [9].
Based on the results from various studies, a relationship was observed between hyperkyphosis and reduced endurance in some cases [9, 13, 15, 23, 25]. However, three studies indicated that this relationship was not statistically significant, suggesting the need for further investigation to clarify the potential impact of hyperkyphosis on endurance outcomes in older adults [9, 24, 26].
3.5.2.3.2 Mobility
Mobility refers to the ability to move freely and easily, which is essential for performing daily activities and maintaining independence, particularly in older adults. It encompasses various aspects of physical function, including balance, coordination, and the capacity to navigate different environments [44].
In the reviewed studies, five utilized the TUG test to assess mobility [11-13, 22, 23]. Among these, four studies found that individuals with hyperkyphosis exhibited poorer performance compared with their counterparts [11, 12, 22, 23]. However, one study reported no significant difference in mobility between healthy older adults and those with hyperkyphosis [13].
Additionally, one study employed the Farsi Version of the Functional Gait Assessment (FGA), which evaluates gait and balance under various conditions. This study found that individuals with hyperkyphosis demonstrated poorer performance on the FGA, indicating compromised mobility [25].
Another study utilized the SPPB, which assesses lower extremity function through a series of tasks, including standing balance and gait speed. Results from this study indicated a significant association between the kyphosis index and poorer performance on the SPPB, with women showing lower scores compared with men among the elderly participants [14].
3.5.3 Impact of Age on Gait Parameters
In one study that assessed walking speed using the Quick Walking Speed Test, it was found that older age was significantly associated with slower walking speed [6]. Similarly, another study utilizing the DynaPort MiniMod also reported that increased age correlated with reduced gait speed [29]. Additionally, a third study indicated that as age increased, the time required to complete the TUG test also increased [12]. Age itself is a known risk factor for hyperkyphosis [25], and in another study, younger individuals with hyperkyphosis demonstrated better performance in the 6MWT compared with their older counterparts [26].
3.5.4 Impact of Gender on Gait Parameters
In one study examining the influence of gender, a significant association was found between higher kyphosis index and poorer performance on the SPPB, as well as reduced walking speed, but only in women. No such association was observed in men [14]. Another study reported that men experienced a significant progression in kyphosis over a 4-year follow-up period, which negatively impacted their gait parameters. This progression highlights the potential gender differences in how kyphosis affects mobility over time [22].
3.5.5 Impact of Demographic and Health Factors on Gait Parameters
One study found that BMC positively correlated with walking speed and step length [21]. Additionally, muscle mass demonstrated a positive relationship with step length, center of pressure, and inclination angle during heel strike [21]. Another study indicated that lower age, greater height, lighter weight, and faster upper limb function positively impacted performance in the 6MWT among individuals with hyperkyphosis [26]. Furthermore, research has shown that taller stature, lower weight, and fewer medications contributed to better performance in the 6MWT for these individuals [24]. Another investigation highlighted that reduced grip strength, vertebral fractures, a BMI over 25, and total hip bone mineral density within the osteoporotic range were associated with prolonged times in the TUG test [12].
4 Discussion
Based on the findings of this systematic review, hyperkyphosis in older adults significantly impacts gait parameters, such as walking speed, stride length, and endurance, which are critical for maintaining balance and mobility. Our review highlighted that hyperkyphosis is strongly associated with mobility limitations in this population. Addressing postural deformities like hyperkyphosis through targeted interventions is essential for improving gait performance among older adults. Our results align with prior systematic reviews, such as Roghani et al. [17], which highlighted the association between hyperkyphosis and physical function decline in older females. However, unlike their meta-analysis, which found no significant relationship between hyperkyphosis severity and walking speed, our review identified a negative correlation. This discrepancy may stem from differences in included populations (e.g., our inclusion of both genders vs. their female-only cohort) and heterogeneity in gait assessment methodologies across studies [17]. Furthermore, a systematic review conducted in 2025 on the impact of hyperkyphosis on balance reported that hyperkyphosis negatively affects dynamic balance. This effect may, in turn, disrupt gait parameters and contribute to mobility impairments [45].
4.1 Standardization Challenges in Hyperkyphosis Diagnosis
While various methods are available to assess kyphosis, there is no universal threshold for diagnosing hyperkyphosis in older adults, making comparisons across studies challenging. Age-related physiological and anatomical changes—such as reduced intervertebral disc height, vertebral wedging, and diminished muscular support—contribute to the progressive development of kyphotic posture [46], further complicating the establishment of standardized diagnostic criteria. Generally, the thoracic kyphosis angle increases with age, rising by approximately 3° per decade after age 40 [2].
Despite the Cobb angle being recognized as the gold standard for measuring kyphosis, no definitive cutoff exists to distinguish normal kyphosis from hyperkyphosis. Some studies suggest thresholds between 40° and 50°, while others define hyperkyphosis as a Cobb angle exceeding 50°. This lack of standardization, combined with inherent measurement errors of 3–5°, poses significant challenges in ensuring diagnostic consistency and comparability across studies. Additionally, variations in kyphosis assessment techniques—ranging from radiographic Cobb angle measurements to noninvasive methods like the flexicurve ruler—further contribute to inconsistencies in diagnosis, particularly in older adults with altered spinal biomechanics [3]. Given these limitations, early detection of kyphosis is crucial, particularly in its initial stages, to enable timely interventions to prevent further progression and mitigate its impact on functional mobility and overall quality of life [30].
4.2 Biomechanical and Physiological Explanations
Hyperkyphosis induces significant biomechanical and physiological alterations that impair gait in older adults. Postural deviations, including increased thoracic kyphosis, reduced lumbar lordosis, and compensatory cervical hyperextension, shift the body's center of mass anteriorly, necessitating compensatory knee flexion and pelvic retroversion to maintain balance [9, 30]. This anterior shift disrupts sagittal alignment, increasing mechanical stress on the spine, hips, and knees, which accelerates degenerative processes such as osteoarthritis [10]. Biomechanical analyses reveal that individuals with hyperkyphosis exhibit elevated knee extension moments and diminished hip abduction moments during gait. These imbalances disrupt weight distribution across the pelvis and upper body, leading to inefficient gait patterns, heightened joint loading, and compensatory muscle fatigue [10, 47].
Additionally, neuromuscular control is compromised due to altered proprioceptive input from the spine and lower extremities, resulting in medio-lateral instability during walking [48]. This instability correlates with impaired postural control mechanisms, such as delayed muscle activation and reduced trunk coordination, which may explain the elevated fall risk observed in this population [2, 48]. For instance, Demarteau et al. demonstrated that medio-lateral step regularity was significantly reduced in hyperkyphotic individuals, reflecting compromised dynamic balance during gait [29].
4.3 The Effect of Hyperkyphosis on Gait Parameters
Hyperkyphosis adversely impacts key gait parameters, including walking speed, stride length, and balance. Studies report that walking speeds below 1.0 m/s—a threshold linked to limited community ambulation—are prevalent among older adults with hyperkyphosis [5]. These reductions are attributed to decreased stride length, cadence, and muscle strength, particularly in the ankle, knee, and hip joints [5, 47]. Compensatory mechanisms, such as increased hip and knee flexion, exacerbate muscular fatigue and reduce gait efficiency [10, 30]. For instance, individuals with hyperkyphosis exhibit 15% slower walking speeds and 20% shorter stride lengths compared to controls, alongside poorer medio-lateral step regularity [29]. Similarly, each 5° increase in kyphosis angle prolongs TUG test times by 0.02 s, underscoring the relationship between kyphosis severity and mobility decline [11].
Comparative analyses highlight inconsistencies in the literature. While some cohort studies report no association between kyphosis and walking speed [6], others observe significant correlations between hyperkyphosis and impaired balance, gait speed, and endurance in community-dwelling older adults [25]. These discrepancies may arise from variations in measurement methods (e.g., Cobb angle vs. flexicurve ruler) and participant characteristics, such as gender and comorbidities. For example, women with hyperkyphosis demonstrate weaker back extensor strength and greater physical performance declines compared to men, likely due to higher osteoporosis prevalence and vertebral fracture rates [14, 25].
4.4 Influence of Gender and Other Risk Factors on Kyphosis and Gait
The development and progression of hyperkyphosis and its impact on gait are influenced by multiple risk factors, including comorbidities (e.g., osteoporosis), lifestyle, and biological determinants [1]. Gender-specific differences are particularly notable, with women being disproportionately affected. Studies indicate that women exhibit weaker back extensor muscle strength compared to men, which contributes to spinal instability and kyphosis progression [9, 11]. Postmenopausal women face elevated risks due to estrogen deficiency, which accelerates bone loss and vertebral fractures—key drivers of hyperkyphosis [16, 25]. For example, longitudinal data from the Study of Osteoporotic Fractures) revealed that women with vertebral fractures have a 2.1-fold higher risk of severe kyphosis (Cobb angle > 50°) compared to those without fractures [16].
The combined effects of muscle weakness and vertebral fractures in women exacerbate gait impairments. Reduced paraspinal muscle mass correlates with slower walking speeds and poorer balance, as demonstrated in a cohort of 1072 older women [16]. These deficits are compounded by anterior shifts in the center of mass, leading to compensatory gait adaptations such as increased hip flexion [10, 25]. Consequently, women with hyperkyphosis are at higher risk of mobility limitations and falls compared to men [9, 23]. In contrast, hyperkyphosis in men is often associated with occupational strains or age-related sarcopenia rather than vertebral fractures [6]. While men also exhibit gait adaptations (e.g., reduced stride length), they generally maintain better dynamic balance, likely due to greater baseline muscle mass [6, 12].
4.5 Clinical Implications
This review highlights the necessity of early detection and standardized assessment of hyperkyphosis in older adults to preserve gait function and mobility. Clinicians should adopt validated tools like the Cobb angle or flexicurve ruler to measure kyphosis severity, facilitating timely interventions objectively. Targeted exercises, including spinal extensor strengthening and balance training, can improve postural alignment and gait stability, reducing fall risk [6, 16, 25].
Women, particularly those with osteoporosis or vertebral fractures, may benefit from gender-specific strategies, such as bone density monitoring (via DXA) and resistance training to mitigate muscle weakness [14, 25]. Integrating gait assessments, such as the TUG test, into routine evaluations can identify mobility impairments early. Assistive devices (e.g., posture braces) and multidisciplinary care involving physiotherapists and geriatricians may enhance functional outcomes [23]. Addressing hyperkyphosis holistically through tailored interventions can improve balance, walking capacity, and quality of life, ultimately lowering the burden of fall-related disabilities in aging populations [5, 30].
4.6 Limitations and Future Research Suggestions
4.6.1 Limitations of the Current Review
Heterogeneity in gait assessment methods (e.g., laboratory vs. clinical tools) and the lack of uniform reporting standards for gait parameters further reduced the ability to perform quantitative meta-analyses. Finally, the exclusion of studies focusing on lumbar hyperkyphosis or combined spinal deformities (e.g., kyphoscoliosis) limits the generalizability of findings to populations with isolated thoracic hyperkyphosis.
4.6.2 Limitations of the Included Studies
This systematic review identifies several limitations in the existing literature. First, significant variation in the methodologies and quality of the included studies affects the findings' comparability and reliability. Furthermore, the predominance of cross-sectional study designs restricts the ability to establish causal relationships between hyperkyphosis and gait parameters. Additionally, many studies failed to adequately control for confounders such as comorbidities, physical activity levels, medications affecting balance, and socioeconomic factors, which may bias the observed associations. Finally, the lack of standardized criteria and precise thresholds for defining hyperkyphosis leads to inconsistencies in measurement and interpretation, further obstructing a clear understanding of the relationship between hyperkyphosis and gait dynamics.
4.6.3 Recommendations for Future Research
In light of these limitations, future research should prioritize establishing standardized diagnostic criteria and measurement thresholds for hyperkyphosis. It is also essential to explore how various factors, including gender, muscle strength, and other physiological attributes, influence hyperkyphosis and gait parameters, thereby enriching our understanding of this condition. Addressing the limitations of clinical methods, which may lack the precision found in laboratory techniques, is crucial. Incorporating innovative technologies, such as wearable sensors, could enhance data accuracy and provide valuable insights into the biomechanical implications of hyperkyphosis. Future studies should investigate the effects of hyperkyphosis on lower extremity joints—specifically the hip, knee, and ankle—along with their associated kinematic and kinetic changes. Additionally, examining the impact of compensatory strategies employed by individuals with hyperkyphosis on gait parameters could yield important insights into mobility and stability. This information will enable practitioners to evaluate the effects of various interventions on gait parameters, ultimately improving treatment strategies for older adults with hyperkyphosis.
5 Conclusion
In conclusion, this systematic review emphasizes the substantial impact of hyperkyphosis on gait parameters in older adults, notably reducing walking speed, stride length, and endurance, which are vital for balance and mobility. The lack of standardized measurement methods and threshold definitions complicates comparisons across studies. Key findings highlight the importance of early identification and targeted interventions for hyperkyphosis. Additionally, recognizing the biomechanical implications and factors such as age and gender are crucial for formulating effective strategies to improve gait performance and mitigate fall risk in this vulnerable population.
Author Contributions
Zeinab Gasavi Nezhad: resources, data curation, software, formal analysis, methodology, validation, visualization, writing – review and editing, writing – original draft, investigation, conceptualization. Steven A. Gard: writing – review and editing, visualization, validation. Mokhtar Arazpour: writing – review and editing, data curation, formal analysis, project administration, supervision, validation, visualization.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The lead author, Zeinab Gasavi Nezhad, affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article and its tables. All authors have read and approved the final version of the manuscript. Zeinab Gasavi Nezhad had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.