The relationship between corona disease anxiety and sleep disturbances and suicidal ideation in medical staff: The mediating role of resiliency and cognitive flexibility: A cross-sectional study
Abstract
Background and Aims
Medical staff have experienced anxiety, sleep disturbances, and suicide due to the COVID-19 epidemic. Thus, this study examined the relationship between corona disease anxiety, sleep problems, and suicidal ideation in medical staff and how resiliency and cognitive flexibility mediate it.
Methods
This descriptive-analytical cross-sectional study examined medical staff. In 2022, participants were affiliated with Hamadan University of Medical Sciences, Iran educational and treatment centers. Sampling was done at primary COVID-19 treatment centers. Data was collected using validated instruments. Ethics were observed during data collecting.
Results
Path analysis was employed to test hypotheses. Analysis showed significant positive relationships between Corona disease anxiety and sleep disturbances (p = 0.001, β = 0.438) and suicidal ideation (p = 0.001, β = 0.310). Conversely, negative and significant associations were identified between resiliency and cognitive flexibility with sleep disturbances and suicidal ideation.
Conclusions
The study illustrates how medical staff's psychological health is linked to COVID-19. High Corona disease anxiety causes sleep disturbances and suicidal thoughts. Resilience and cognitive flexibility modulated Corona disease anxiety, sleep problems, and suicidal thoughts. The comprehensive study focuses on medical staff mental health issues, suggesting targeted solutions.
1 INTRODUCTION
The COVID-19 pandemic was a major tragedy that affected the world and challenged governmental, economic, and health care systems due to widespread contagious diseases. Its unknown nature, rapid spread, and resulting casualties caused significant anxiety among citizens.1 Health care workers at the forefront of the battle against this disease soon faced high workloads, psychological pressure, and doubled stress.2 Additionally, the infection and high mortality rate among health care personnel engaged in community care, along with shortages of facilities and equipment and the prolonged duration of the pandemic, jeopardized the health status and well-being of medical staff.3 Reports emerged from various parts of the world about depression, anxiety, irritability, mood swings, sleep disturbances, and suicide stemming from COVID-related anxiety among health care workers.4-6 Corona disease anxiety is common among health care personnel and potentially impacts their well-being and health.7 This anxiety became so prevalent that a scale was exclusively designed to measure its effects on individuals.8
One significant consequence of corona disease anxiety is sleep disturbances; sleep disturbances are a prominent sign in individuals with depression and were previously considered secondary manifestations of primary depression symptoms.9, 10 However, Numerous long-term research has shown that sleeplessness is a separate risk factor for young, middle-aged, and older people to experience acute or chronic depression, which can be the root cause of suicidal thoughts. This bidirectional relationship between sleep disturbances and depression has led to the perspective that sleep disturbances are not just an initial sign of depression but rather a predictive indicator.11 Another crucial consequence of anxiety is suicide; numerous studies have demonstrated a link between suicidal thoughts and suicide attempts with anxiety. Research suggests that the experience of anxiety can significantly increase the risk of suicide.12
As mentioned, anxiety can lead to sleep disturbances and increase vulnerability to suicidal thoughts or actions. Therefore, corona disease anxiety could potentially be equally impactful. Moreover, anxiety-induced sleep disturbances can serve as a precipitating factor for suicide. Given the direct relationship between sleep disturbances and depression, individuals with suicidal thoughts or suicide attempts have been found to experience significant levels of anxiety and depression accompanied by sleep disturbances.13 Sleep disturbances are among the top 10 warning signs of suicide.14 Studies have shown that prescribing sleep medications is associated with reducing the risk of suicide in patients with sleep disorders.15 It is anticipated that suicidal behaviors may increase due to the COVID-19 pandemic, although currently, evidence of suicide among health care workers, as a vulnerable population, exists.16 However, some factors may act as mediators. Resiliency is one of the most critical psychological factors that can help individuals cope with challenges and crises, safeguarding their mental health against stressors and anxiety-inducing conditions.17 Resiliency refers to the ability to learn, manage, and adapt to challenging circumstances and respond flexibly to daily life pressures, which aids individuals in protecting their well-being, happiness, and meaningful life against internal and external stressors.18 From a psychological perspective, resilient individuals possess adaptability and social and communication skills. When confronted with challenges and stressful situations, they approach problems more efficiently in thinking and acting.18 Another essential variable is cognitive flexibility. Cognitive flexibility refers to an individual's capacity to shift between mental states and adapt to new or changing environments.19 Evidence suggests that cognitive flexibility is related to psychological well-being and vulnerability to various disorders, including anxiety, depression, and general distress.20 The rapid spread of the coronavirus, lack of equipment and facilities, human resource shortages, the virus's unknown nature, and the prolonged epidemic have made health care workers more vulnerable to corona disease anxiety.4 Due to high workloads, long shifts, and anxiety, reports of sleep disturbances, depression, anxiety, and suicide among health care workers have been published worldwide.12, 13
Aljaberi and colleagues' research found a correlation between the coronavirus pandemic and various psychological issues like depression, anxiety, and insomnia.5, 10 Moreover, in an academic inquiry, Sabah et al. elucidated that family communication can serve as a mediator for resilience and familial functioning amid the challenges posed by the coronavirus pandemic.21
However, why are some individuals more vulnerable while others exhibit better resistance in these circumstances? Why are some less affected by external stressors, experience less anxiety, have fewer sleep disruptions, are less prone to depression, and think less about suicide? In this context, the roles of two critical psychological factors, resiliency and cognitive flexibility, must be explored. Despite a comprehensive literature review, no research has been conducted to answer these questions.
Therefore, the present study aims to investigate the relationship between corona disease anxiety, sleep disturbances, and suicidal ideation and the exact mediating roles of resiliency and cognitive flexibility.
2 MATERIALS AND METHODS
2.1 Study design and participants
This study adopted a descriptive-analytical cross-sectional design. This design allows for a comprehensive assessment of the relationships between corona disease anxiety, sleep disturbances, suicidal ideation, resiliency, and cognitive flexibility in medical staff, offering insights into their interconnections within a specific timeframe. All studies were approved by the ethics committee of Islamic Azad University, Hamedan branch, and were performed following the Declaration of Helsinki.
2.2 Sample size
200 participants were selected based on the number of variables, with a stratified sampling approach of 40 individuals for each variable (1 predictor, 2 criterion, and 2 mediator variables).22
2.3 Sampling and procedures
The target population was medical staff, including nurses, nurse assistants, and physicians, employed in educational and treatment centers affiliated with Hamedan University of Medical Sciences in 2022. The sampling procedure involved the purposive selection of three primary COVID-19 treatment centers, namely Sina, Shahid Beheshti, and Besat Hospitals, which served as the main patient care facilities for COVID-19 patients in Hamedan.
Subsequently, medical staff members working in sections dedicated to COVID-19 patient care were chosen as study participants. The inclusion criteria encompassed being employed in one of the educational and treatment centers affiliated with Hamadan University of Medical Sciences, having experienced the COVID-19 pandemic crisis in COVID-19 wards, expressing willingness to participate, and having an age range of 18−65 years. Exclusion criteria included opting not to continue participation, incomplete questionnaire responses, and use of psychiatric medications.
Through ward officials' coordination, a trained psychologist visited the desired centers to gather information and interviewed doctors and nurses. Following a brief discussion and assessment of the entry and exit requirements, he provided them with questionnaires to fill out. The research employed several validated tools for data collection. Ethical considerations were upheld by providing participants with a clear explanation of research objectives and data confidentiality. The designated questionnaires were administered to eligible participants in collaboration with hospital authorities. Adequate time was allocated for questionnaire completion, after which the data were entered into relevant software for analysis.
2.4 Ethical considerations
This research has been approved by the Research and Ethics Council of the Islamic Azad University, Hamadan branch, with the ethics code IR.IAU.H.REC.1401.011.
2.5 Research tools
- 1.
Demographic Information Checklist: Gender, age, marital status, degree of education, employment history, occupation, hospital name, and other details are covered in this checklist.
- 2.
Corona Disease Anxiety Scale (CDAS): Developed and validated for assessing coronavirus-related anxiety in Iran, this tool comprises 18 items categorized into psychological (items 1−9) and physical symptoms (items 10−18). Responses are scored on a 4-point Likert scale (0−3), yielding scores ranging from 0 to 54. A higher score indicates higher anxiety levels. The tool demonstrated high reliability (Cronbach's alpha α = 0.919) and good validity with the GHQ-28 questionnaire.23
- 3.
Pittsburgh Sleep Quality Index: This questionnaire, finalized in 1980, assesses sleep disturbances over the past month. It consists of 9 core questions, including open-ended, short-answer, and multiple-choice questions. It encompasses seven domains and has been validated in the Persian version, showing satisfactory reliability (Cronbach's alpha coefficient of 0.77 for screening, and 0.80 overall).24, 25
- 4.
Beck Scale for Suicidal Ideation: Developed in 1979, this 19-item self-report questionnaire assigns scores from 0 to 2 for each question. Scores range from 0 to 38, assessing attitudes and plans related to suicide. It demonstrates high reliability and validity in both the original study and Persian version, with various reliability coefficients reported.26, 27
- 5.
Connor-Davidson Resilience Scale (CD-RISC): A 25-item questionnaire on a 5-point scale, measuring resilience. It showed good reliability in the study (Cronbach's alpha α = 0.87) and has been normalized in Iran for various groups, demonstrating acceptable reliability and Cronbach's α coefficients of 0.77 and 0.90.28, 29
- 6.
Cognitive Flexibility Questionnaire: Developed by Dennis and Vander Wal in 2010, this questionnaire comprises 20 questions assessing cognitive flexibility in clinical and nonclinical settings. It demonstrated good concurrent and convergent validity in both the original study and in Iran.30, 31
2.6 Statistical analysis
Data were analyzed using descriptive methods, such as frequency tables and graphs, and inferential statistics including correlation and regression analyses in SPSS-26 and path analysis in AMOS-24 were used to examine the data and test hypotheses.
3 RESULTS
Participants characteristics were shown in Table 1. The age range was 19-50 years old and most of them were females (112, 61.50%), single (102, 56%), and Bachelor's degree (117, 64.3%).
| Age | Frequency | Percentage |
|---|---|---|
| Less than 25 years old | 74 | 40.7 |
| 25–30 years old | 42 | 23.1 |
| 30–35 years old | 19 | 10.4 |
| More than 35 years old | 47 | 25.8 |
| Total | 182 | 100 |
| Gender | Frequency | Percentage |
| Female | 112 | 61.5 |
| Male | 70 | 38.5 |
| Total | 182 | 100 |
| Marital status | Frequency | Percentage |
| Single | 102 | 56 |
| Married | 78 | 42.9 |
| Divorced | 2 | 1.1 |
| Total | 182 | 100 |
| The level of education | Frequency | Percentage |
| Diploma | 24 | 13.2 |
| Associate degree | 10 | 5.5 |
| Bachelor's degree | 117 | 64.3 |
| Master's degree | 16 | 8.8 |
| Doctoral degree | 15 | 8.2 |
| Total | 182 | 100 |
Eighteen participants (9.9%) were doctors, 121 (66.5%) were nurses, and 24 (13.2%) were caregivers or assistant caregivers. Additionally, six people (3.3%) were involved in the services department, and 13 (1.7%) worked in other departments. Sixty-two candidates (34%) were working at Besat Hospital, 60 (33%) were at Sina Hospital, and 60 (33%) were at Shahid Beheshti Hospital. One hundred sixty-nine people (92.9%) had a history of COVID-19 infection, and 13 (7.1%) had no COVID-19 infection.
Table 2 presents the mean and SD of the corona disease anxiety, resiliency, cognitive flexibility, sleep disturbances, and suicidal ideations of participants as well as correlation these variables. Participants scored an average of 12.51 ± 6.39 on the corona disease anxiety, 64.25 ± 16.25 on the resiliency, 63.29 ± 18.91 on the cognitive flexibility, 8.68 ± 3.03 on the sleep disturbances and 2.89 ± 4.74 on the suicidal ideations.
| Research variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Corona disease anxiety | − | ||||
| 2. Resiliency | −0.32** | − | |||
| 3. Cognitive flexibility | −0.39** | 0.12 | − | ||
| 4. Sleep disturbances | 0.42** | −0.43** | −0.39** | − | |
| 5. Suicidal ideations | 0.29** | −0.40** | −0.28** | −0.29** | − |
| Mean | 12.51 | 64.25 | 63.29 | 8.68 | 2.89 |
| SD | 6.39 | 16.26 | 18.91 | 3.03 | 4.74 |
- ** p < 0.01.
The data was declared normal because the skewness and kurtosis values for all variables were between −1 and +1. Hence, Pearson's correlation coefficient values were reported.
As presented in Table 2 the relationships are expected in the directions such that corona disease anxiety was negatively associated with cognitive flexibility (r = −0.39, p < 0.001) and resiliency and negatively associated with sleep disturbance (r = −0.42, p < 0.001) and suicidal ideations (r = −0.29, p < 0.001).
This study used the path analysis method to test research hypotheses. For this purpose, a model was designed in which both direct and mediated (by the resiliency and cognitive flexibility) relationships between corona disease anxiety and suicidal ideations and sleep disturbance were depicted. The model fitness was evaluated using the path analysis method, AMOS 24.0 software, and maximum likelihood estimation. Table 3 shows the fitness indices of the path model such as goodness fit index (GFI), adjusted goodness fit index (AGFI), comparative fit index (CFI), and root mean square error of approximation (RMSEA).
| Fitness indicators | Model | Cut-offa |
|---|---|---|
| Chi-square | 0.91 | - |
| Freedom degree | 2 | - |
| b | 0.46 | <3 |
| GFIc | 0.998 | <0.90 |
| AGFId | 0.985 | <0.850 |
| CFIe | 1.00 | <0.90 |
| RMSEAf | 0.007 | >0.08 |
- Abbreviations: AGFI, adjusted goodness fit index; CFI, comparative fit index; GFI, goodness fit index; RMSEA, root mean square error of approximation.
- a Cut-offs based on Klein's perspective (2016).
- b Normed chi-square.
- c Goodness fit index.
- d Adjusted goodness fit index.
- e Comparative fit index.
- f Root mean square error of approximation.
Table 3 indicates that all fitness indices resulting from path analysis support an acceptable fitness of the model to the collected data (χ2/df = 0.46, GFI = 1.00, GFI = 0.998, AGFI = 0.996, and RMSEA = 0.007). Therefore, it can be concluded that the research model fits well with the collected data.
Before interpreting the results of the Standardized Model Coefficients for the Mediation Model several assumptions were evaluated.
First, inspection of the normal probability plot of standardized residuals as well as the scatterplot of standardized residuals against standardized predicted values indicated that the assumptions of normality, linearity and homoscedasticity of residuals were met. Second, the skewness and kurtosis of the Mahalanobis distance were obtained as 2.14 and 6.80, respectively, indicating that the skewness and kurtosis values of the relevant information are outside the range of ±2. Therefore, the box plot of the Mahalanobis distance information was drawn, the data corresponding to two participants formed multivariate outliers. Third, relatively high tolerances for both predictors in the Standardized Model Coefficients for the Mediation Model, indicated that multicolinearity would not interfere with our ability to interpret the outcome of the MRA.
Table 4 shows that the indirect path coefficient between Corona disease anxiety and sleep disturbances (p = 0.001, β = 0.197), and the indirect path coefficient between Corona disease anxiety and suicidal ideations (p = 0.001, β = 0.206), are positive and significant. This indicates that cognitive resiliency and flexibility mediate the relationship between Corona disease anxiety and sleep disturbances and COVID-19 anxiety and suicidal ideations as well. Since the research model had two mediators (cognitive resiliency and flexibility), the unique contribution of each of them in the relationship between the independent and dependent variables was not determined. Therefore, the proposed Baron and Kenny formula was used to determine the unique role of each mediator in the relationship between the independent and dependent variables.
| Sleep disturbances | Suicidal ideations | Resiliency | Cognitive flexibility | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | B | p | β | SE | B | p | β | SE | B | p | β | SE | B | p | |
| Direct | ||||||||||||||||
| Corona anxiety | 0.081 | 0.023 | 0.241 | 0.002 | 0.055 | 0.046 | 0.104 | 0.223 | −0.575 | 0.111 | −0.325 | 0.001 | −0.914 | 0.127 | −0.437 | 0.001 |
| Resiliency | −0.049 | 0.012 | −0.257 | 0.001 | −0.110 | 0.022 | −0.369 | 0.001 | ||||||||
| Cognitive flexibility | −0.042 | 0.013 | −0.258 | 0.001 | −0.049 | 0.024 | −0.196 | 0.03 | −0.049 | 0.012 | −0.257 | 0.001 | ||||
| Indirect | ||||||||||||||||
| Corona anxiety | 0.066 | 0.015 | 0.197 | 0.001 | 0.108 | 0.026 | 0.206 | 0.001 | ||||||||
| Total | ||||||||||||||||
| Corona anxiety | 0.148 | 0.023 | 0.438 | 0.001 | 0.163 | 0.034 | 0.310 | 0.001 | ||||||||
The use of Baron and Kenny's formula showed that the path coefficient between Corona disease anxiety and suicidal ideations through resiliency (p = 0.001, β = 0.099), the path coefficient between COVID-19 anxiety and sleep disturbances through resiliency (p = 0.001, β = 0.086), the path coefficient between COVID-19 anxiety and suicidal ideations through cognitive flexibility (p = 0.001, β = 0.088), and the path coefficient between COVID-19 anxiety and sleep disturbances through cognitive flexibility (p = 0.001, β = 0.114) are positive and significant. Based on above mentioned, it was concluded that among health care workers, resiliency and cognitive flexibility mediate the relationship between COVID-19 anxiety and suicidal ideations, and sleep disturbances in a positive and significant way.
Figure 1 shows that the sum of squared multiple correlations for sleep disturbances and suicidal ideations variables equals 0.30 and 0.25, respectively. This indicates that Corona disease anxiety, cognitive flexibility, and resiliency explain 30% and 25% of the variance in sleep disturbances and suicidal ideations in the medical treatment field.
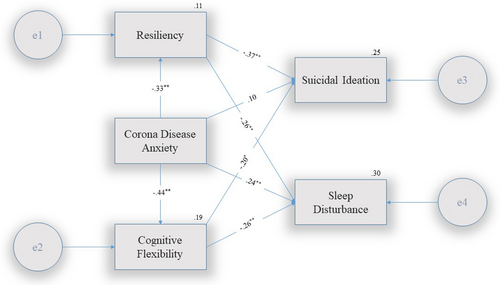
Figure 1 illustrates the structural model of the study in explaining the relationship between Corona disease anxiety, sleep disturbances, and suicidal ideations based on the mediating role of resiliency and cognitive flexibility.
4 DISCUSSION
The outcomes of this investigation unveiled a noteworthy correlation between Corona disease anxiety and sleep disturbances in health care personnel directly engaged in COVID-related activities. These findings align with the research outcomes of Akbarpour and Bakul.32, 33 A cross-sectional study in Bangladesh involving 211 university students and employees in 2021 illustrated a significant association between Corona disease anxiety and sleep disturbances among this group.33 Similarly, a cross-sectional study in Iran conducted on 1223 participants through online questionnaires in 2021 revealed a substantial linkage between COVID-19 fear and depression, anxiety, and insomnia. It was noteworthy that the intensity of insomnia was notably elevated in individuals aged above 50.32
These findings can be elucidated by recognizing that Corona disease anxiety triggers mechanisms analogous to those observed in other anxiety disorders, leading to repercussions such as insomnia, the onset of depressive symptoms, hypervigilance, and more.34 The experience of chronic stress activates components of the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS).35 Prolonged engagement of the sympathetic system and the HPA axis contributes to the emergence of depressive symptoms, fatigue, and sleep disorders, thereby potentially heightening enduring vulnerabilities in immune and cognitive functions36 and it also has a detrimental effect on quality of life.37 As a result, health care personnel during the pandemic face not only immediate risks of sleep disturbances but also long-term ramifications, including the potential for adverse health outcomes such as cancer.
Additionally, the findings underscored a significant correlation between Corona disease anxiety and suicidal ideation. In the context of existing literature, these results resonate with the outcomes of various past studies, including Farooq, Eleftheriou, and Ma.38-40 A comprehensive systematic review was undertaken by Farooq and colleagues, encompassing 38 studies with 120,076 participants, which exposed significantly higher rates of suicidal thoughts and suicide attempts during the COVID-19 pandemic compared to pre-pandemic figures within the general population. The review highlighted factors such as diminished social support, physical exhaustion, health care workers' vulnerability, sleep disturbances, quarantine, loneliness, and mental health struggles as pivotal risk components for suicidal ideation.39
These insights can be explicated by recognizing that the global prevalence of COVID-19 and its ramifications have engendered substantial transformations in psychological and social landscapes. Individuals grapple with apprehensions about the disease, seclusion, ambiguity, and lifestyle upheavals, collectively contributing to heightened anxiety and stress. Health care professionals working directly with individuals navigating these challenges are at the forefront of assisting them.38 Suicidal ideation signifies psychological imbalances, with anxiety potentially amplifying its occurrence.13 Thus, it can be hypothesized that heightened Corona disease anxiety indirectly increases suicidal ideation among health care personnel.
Furthermore, the results spotlighted an inverse correlation between resiliency and suicidal ideation. Resilience was a mediator in the nexus between coronavirus anxiety and suicidal ideation. These findings coalesce with the conclusions of Seidler et al.41 and Zhang et al.42 A study centered on 700 Australian men deploying online questionnaires during the 2020 COVID-19 pandemic disclosed that interpersonal relationships, resilience, and coping strategies could act as protective factors against suicidal ideation.41 Similarly, research conducted in China in 2022 involving 12,917 students examined suicidal ideation, resilience, social support, and depressive symptoms, revealing a significant inverse connection between resiliency and suicidal ideation.42
These insights can be attributed to clinical staff encountering elevated psychological and social pressures while engaging with individuals in critical and daunting scenarios. These circumstances might instigate suicidal ideation due to the influence of psychological trauma and heightened stress. As a psychological trait, resilience equips individuals to navigate stress and adversity, thereby upholding their mental well-being. Consequently, individuals exhibiting elevated resilience levels are less susceptible to experiencing suicidal ideation. Resiliency is a buffer against the adverse impacts of stressors, mitigating the onset of depressive symptoms, exhaustion, and despair, potentially as a protective shield against suicidal ideation.43
Regarding the relationship between resiliency and sleep disturbances, this study uncovered that individuals with higher resilience encounter fewer sleep disturbances. Furthermore, resiliency mediated the connection between Corona disease anxiety and sleep disturbances. These findings harmonize with the research by Pappa, Matsumoto, and Bozdag.44-46 In a comprehensive review by Pappa et al., exploring the repercussions of sleep disturbances on health care workers, the research identified risk factors such as young age, female gender, health concerns, and frontline responsibilities. Moreover, the pivotal role of resilience in mitigating vulnerability and averting enduring physical and psychological outcomes was underscored.46 A Turkish study involving 214 health care workers in 2020 evidenced the positive impact of adequate sleep on enhancing resilience. This implies that improving sleep quality, life contentment, and positive emotions can enhance health care workers' resilience. Consequently, a plausible bidirectional connection exists between sleep disturbances and resilience.44
Exploring these results entails acknowledging the substantial modifications experienced by individuals in their daily lives during the COVID-19 pandemic. Apprehensions related to the disease, social isolation, work-related distress, economic fluctuations, and the prevalence of distressing news can all lead to heightened anxiety and physiological responses, including sleep disturbances. Individuals may grapple with various sleep issues, such as recurrent night awakenings, difficulties falling asleep, and nightmares, significantly impacting daily functioning and mental well-being.33 On the other hand, resilience plays a pivotal role in safeguarding mental health against stressors, moderating the adverse effects of anxiety encounters.47 Those with elevated resilience levels tend to employ more effective strategies for managing and controlling their anxiety. In essence, resilience is a defense mechanism against anxiety, diminishing its detrimental impact. Drawing from the outcomes of this study and existing research, it is plausible to suggest a bidirectional relationship between resiliency and sleep disturbances, where heightened resilience lessens sleep disturbances and sleep disorders, which diminishes resilience. However, a definitive cause-and-effect relationship has yet to be established, as other unexamined variables in our study or the reviewed literature may offer further clarity.
Examining the relationship between cognitive flexibility and suicidal ideation unveiled a negative correlation between cognitive flexibility and suicidal ideation. Cognitive flexibility further mediated the linkage between Corona disease anxiety and suicidal ideation. These findings are in accord with studies conducted by MacPherson et al.48 and Hausman.48, 49 A study involving 87 U.S. military veterans with alcohol use disorder and post-traumatic stress disorder probed the relationship between cognitive flexibility, self-harming behaviors, suicidal ideation, and impulsivity. The findings established that higher cognitive flexibility is linked to diminished impulsive behaviors and suicidal ideation in this group.49
Unpacking these insights based on the research background, it can be posited that factors such as intrusive negative thoughts and emotions, inaccurate risk assessment, hasty decisions, and persistent anxiety and depression contribute to the genesis of suicidal ideation.50 Conversely, the role of cognitive flexibility in organizing thoughts and beliefs and adapting them to new and unforeseen circumstances should not be underestimated. Accordingly, participants who faced high occupational stress, direct exposure to COVID-19 patients, and challenging situations during the pandemic crisis and displayed elevated cognitive flexibility exhibited lower suicidal ideation scores. Conversely, those with lower cognitive flexibility reported higher suicidal ideation scores. Essentially, individuals adept at adapting their thoughts and perspectives to stress-inducing scenarios and selecting effective anxiety management strategies are more likely to reduce suicidal ideation. Therefore, cognitive flexibility might mediate the relationship between coronavirus anxiety and suicidal ideation. One of the pivotal medications for mitigating suicidal ideation is ketamine. Ketamine promptly curtails suicidal ideation within an hour of administration, with effects extending up to a week. Current evidence underscores diverse mechanisms for ketamine's anti-suicidal efficacy, including its impact on neuroplasticity, the reward system, and pain processing.51 Neuroplasticity, synonymous with neural plasticity or brain plasticity, embodies the brain's adaptability through structural and functional modifications. Studies support the link between cognitive flexibility and neuroplasticity.52 Indications suggest that ketamine elicits neural plasticity in brain networks, contributing to its antidepressant and anti-suicidal effects.53 Given ketamine's influence on neuroplasticity, its mitigation of suicidal ideation, and the robust correlation between neuroplasticity and cognitive flexibility,52 neuroplasticity could potentially constitute a shared factor between ketamine's effects and cognitive flexibility in reducing suicidal ideation. This revelation paves the way for novel avenues in future research.
Exploring the relationship between cognitive flexibility and sleep disturbances unveiled a negative correlation between cognitive flexibility and sleep disturbances. Additionally, cognitive flexibility mediated the link between coronavirus anxiety and sleep disturbances. These findings aligned with the outcomes of studies conducted by Olsson and Roberge54, 55 while contrasting with the results of investigations by Chen and Tucker.56, 57 A significant correlation emerged between sleep disturbances and cognitive brain activities in a study encompassing 911 cancer survivors in the United States from 2013 to 2016. This observation indicates a bidirectional association between sleep and cognitive functions such as attention, processing speed, memory, and cognitive flexibility. This study linked Lower cognitive flexibility scores with sleep disturbances.54 Conversely, a study conducted in China in 2020 on 204 children assessed the relationship between cognitive activities and sleep quality. While a significant connection between memory and sleep quality emerged, no substantial association between sleep and cognitive flexibility was evident.56
Unpacking these findings necessitates acknowledging that cognitive models of sleep disturbances propose that persistent effortful rumination to initiate sleep and maladaptive beliefs are among the primary contributors to sleep disturbances.58 On the other hand, cognitive flexibility entails shifting from entrenched patterns of thought to novel perspectives, transcending stereotypical responses, and accommodating novel scenarios.19 Thus, individuals capable of recalibrating their beliefs or habits when circumstances warrant it are deemed cognitively flexible, potentially yielding more effective responses amid stressors and pressure, akin to health care workers grappling with the COVID-19 pandemic. Scrutinizing existing research, it becomes apparent that incongruous outcomes exist concerning the association between cognitive flexibility and sleep disturbances, warranting further comprehensive investigation. Moreover, it is worth considering the impact of the Corona disease anxiety experience on brain neuroplasticity and its subsequent ramifications for cognitive flexibility and sleep disturbances. Research has indicated that chronic anxiety influences brain neuroplasticity by inducing repetitive loops, curbing neural adaptability, and diminishing cognitive flexibility.59 These findings reinforce the connection between heightened cognitive flexibility and augmented neural adaptability, reducing susceptibility to anxiety.41 Sleep disturbances might function as indicators of neuroplasticity disruptions, which could disrupt various neural regulatory mechanisms. In this context, treating sleep disturbances may bolster natural sleep processes and fortify the stress response system, neural inflammation, and brain plasticity. Additionally, enhancing cognitive flexibility and augmenting brain plasticity could be pivotal in preempting and safeguarding against sleep disturbances.58 These interconnected relationships underscore the complex interplay between anxiety, cognitive flexibility, brain neuroplasticity, and sleep disturbances, necessitating more in-depth exploration and consideration in future research endeavors.
Although the epidemic occurred few years ago, recent studies underscore its long-term effects, particularly on economic growth,60 financial hardships and unemployment rates.61 Worldwide, these consequences influence a range of social issues, including lifestyle, alcohol and tobacco use, physical activity levels, sleep disorders,62 depression,63 and in some instances, an elevated risk of suicide.64
5 STRENGTHS AND LIMITATIONS
The study reveals critical theoretical and practical insights into the mental health of health care workers during the COVID-19 pandemic. These findings suggest that enhancing resilience and cognitive flexibility can mitigate anxiety's adverse effects, promoting better mental health and reducing sleep issues and suicidal thoughts. Practically, the study advocates for targeted mental health interventions, resilience training, and cognitive flexibility enhancement within health care settings. The robust methodology and focus on a relevant population further underscore the study's significance in informing effective strategies to support health care workers' well-being during high-stress periods.
Despite the commendable aspects of this study, it is crucial to acknowledge several constraints that require consideration. These include potential sampling bias due to the regional focus, a cross-sectional design that limits causal inference, and the potential for response bias in self-reported data. Given the findings and these limitations, it is advisable to consider conducting longitudinal studies to grasp temporal relationships better. Additionally, utilizing diverse samples of health care workers and exploring neurobiological mechanisms within mental health could further enhance our understanding of this complex issue.
6 CONCLUSIONS
The study delved into the relationships between various psychological factors among medical staff engaged in COVID-19 activities. It revealed that Corona disease anxiety had strong links with sleep disturbances and suicidal thoughts, highlighting the widespread impact of heightened anxiety on mental health. The stress response triggered by anxiety led to disrupted sleep patterns and an increased risk of suicidal ideation. The research underscored the urgent need for tailored interventions and mental health support for health care workers combating pandemic challenges. Resilience was identified as a significant protective element that mitigated the adverse effects of Corona disease anxiety, and sleep issues. It acted as a buffer against the adverse psychological and physiological outcomes of heightened anxiety, suggesting that interventions to foster resilience could alleviate the mental health toll on health care professionals. Cognitive flexibility, a crucial cognitive trait, was discovered to mediate the connections between Corona disease anxiety, suicidal thoughts, and sleep disturbances. This highlighted the role of adaptable thinking in influencing mental health outcomes during crises. The study's exploration of the bidirectional relationships between cognitive flexibility, neuroplasticity, and mental health outcomes offered potential for innovative intervention strategies. Ultimately, the intricate interplay among these factors underscored the importance of a comprehensive approach to addressing the mental health challenges faced by health care personnel during a pandemic. The study contributes to the growing knowledge base informing mental health strategies for health care workers, providing a basis for further research and targeted interventions. Prioritizing the health of frontline staff is still essential in light of COVID-19's continuing consequences and other potential future pandemics.
During the preparation of this work, the authors used ChatGPT 3.5 to help translate the manuscript from Persian to English and improve the language. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
AUTHOR CONTRIBUTIONS
Saeid Yazdi-Ravandi and Arya Haddadi chose the topic, designed the study, and defined the concepts. Arya Haddadi did a literature search and researched the background. Arya Haddadi did the data collection. Nasrin Matinnia did data analysis. The draft was written and prepared by Arya Haddadi and Saeid Yazdi-Ravandi. All authors discussed the results and participated in editing the final version of the article.All authors have read and approved the final version of the manuscript. Saeid Yazdi-Ravandi had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
ACKNOWLEDGMENTS
The authors thank and appreciate the cooperation of all participants in this research. This research was funded by the Islamic Azad University of Hamedan and Hamadan University of Medical Sciences and conducted as part of the first author's Master's thesis in Clinical Psychology. No grants were declared.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
Before filling out the surveys, participants received detailed information about the study, and their informed consent was obtained.
TRANSPARENCY STATEMENT
The lead author Saeid Yazdi-Ravandi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
All authors have read and approved the final version of the manuscript. Saeid Yazdi-Ravandi had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.