Effective process quality control management for constipation prevention in hospitalized patients with acute coronary syndrome: An observational study
Abstract
Objective
To evaluate the effectiveness of monitoring and managing process quality control indicators in the prevention of constipation among hospitalized patients with acute coronary syndrome (ACS).
Methods
A total of 512 hospitalized patients diagnosed with ACS between January and June 2022 were screened for inclusion in the study. Ultimately, 456 eligible participants were enrolled and divided into two groups based on the chronological order of admission: the control group and the observation group. Upon admission, both groups of patients received routine constipation prevention measures in the department. However, the observation group was subjected to targeted process quality control management, which included monitoring and managing five indicators related to constipation prevention: correctness of bowel movement recording; usage rate of laxatives; execution rate of physical interventions; implementation rate of constipation prevention education; completion rate of dietary structure and habit assessments. Data were analyzed using SPSS, with t tests and χ2 tests for group comparisons.
Results
In comparison to the control group, the observation group demonstrated significant advantages in terms of constipation incidence, completion rates of the five process quality control indicators, occurrence rates of adverse cardiac events during defecation, and PHQ-9 scores before discharge. These disparities demonstrated statistical significance with a p value < 0.05.
Conclusion
Target-oriented process quality control management is shown to be effective in reducing constipation incidence and adverse cardiac events during constipation episodes, as well as alleviating depressive symptoms among ACS patients, thus providing a safe and effective approach to constipation prevention.
1 INTRODUCTION
With the global population aging, cardiovascular diseases (CVD) have emerged being a significant factor in both worldwide fatalities and disability, imposing an increasingly significant burden on both health and society.1 The gradual increase in the prevalence of CVD, driven by factors such as an aging population and unhealthy lifestyles, has prompted extensive research into potential risk factors. One such factor of interest is constipation.2
Constipation, a prevalent digestive concern, is defined as the persistence of symptoms for a minimum of 6 months, with at least two of the following symptoms occurring in over one-fourth of defecations during the past 3 months: straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal obstruction/blockade, and the need for manual maneuvers to facilitate defecation. Additionally, there should be fewer than 3 defecations per week, absence of loose stools, and insufficient criteria for diagnosing irritable bowel syndrome.3 In recent years, there has been a burgeoning interest within the scientific community to investigate the connection between constipation and CVDs.2, 4, 5 Previous studies have revealed that constipation affects a substantial proportion of patients with CVD, with estimates indicating rates of up to 50%.2 Additionally, in patients with acute coronary syndrome (ACS), this percentage may reach as high as 53.3%.6 Furthermore, constipation, in turn, influences the prognosis of CVD and is linked to an elevated independent risk of adverse cardiovascular outcomes and cardiovascular risk factors, particularly an increased susceptibility to arteriosclerosis.7, 8
Of particular concern is the fact that straining during defecation can result in elevated intra-abdominal pressure and an increased volume of blood returning to the heart, thereby adding to the workload of the heart. This heightened stress on the cardiovascular system increases the risk of adverse cardiac events, especially in patients with ACS.2, 7 Therefore, the proactive prevention of constipation during the hospitalization of ACS patients is not only a nursing priority but also a challenging endeavor5, 9
Preventing constipation in patients with coronary heart disease has become a cornerstone of clinical practice,10 and a wealth of research has underscored the pivotal role played by a range of interventions in this domain. These interventions encompass medication,10, 11 conventional therapies,11 nursing care,11, 12 and traditional Chinese medicine treatments.13, 14 Of particular note is the pronounced impact of scientifically sound and effective nursing care in managing constipation among patients. However, when it comes to the practical implementation of these measures, there is a notable absence of effective quantitative metrics and objective assessment tools. Consequently, the translation of these approaches into widespread clinical adoption and quality control measures becomes challenging. The application of nursing sensitivity quality indices allows for a comprehensive evaluation encompassing the structural, procedural, and outcome aspects of nursing practices.15 This approach facilitates genuine and objective assessments of nursing quality, serving as an effective safeguard for both nursing quality and patient safety.15, 16
Hence, the primary objective of this study was to evaluate the effectiveness of process quality control indicators in preventing constipation among ACS patients. Additionally, the study aimed to establish robust quantitative standards and objective evaluation methods for the implementation of these measures, with the ultimate goal of facilitating their widespread adoption in clinical practice.
2 METHODS
2.1 Study population
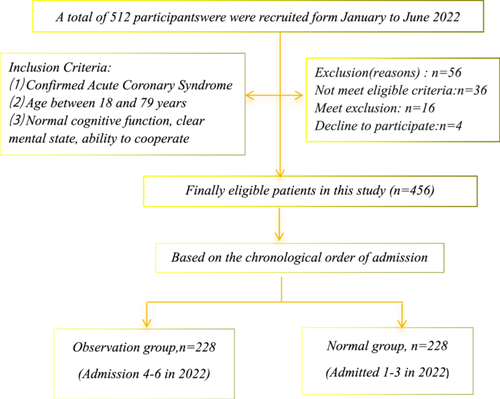
This observational study enrolled 512 patients diagnosed with ACS at the Cardiology Department of Dongjie Hospital and Jinshan Hospital within Fujian Provincial Hospital between January and June 2022. After rigorous screening, 456 eligible participants were selected. Out of these, 228 patients admitted from January to March 2022 constituted the routine group, while the remaining 228 patients admitted from April to June 2022 formed the observation group. The allocation process is illustrated in Figure 1.
2.2 Inclusion and exclusion criteria
Inclusion Criteria were as follows: (1) Confirmed ACS17; (2) Age between 18 and 79 years; (3) Normal cognitive function, clear mental state, ability to cooperate, and all participants in the study provided informed consent for their participation. Exclusion Criteria were as follows: (1) Severe systemic conditions affecting vital organs such as the liver, brain, or kidneys; (2) A history of mental illnesses including schizophrenia or schizoaffective disorder (ICD-10: F20.x or F25.x) or bipolar disorder (ICD-10: F31.x)18; (3) Patients currently taking sedative medications; (4) A history of chronic constipation that cannot be managed with medications or techniques; (5) Acute onset of various infections, fevers, or other systemic diseases.
2.3 Ethical considerations
Our study was ratified by the Ethics Committee of Fujian Provincial Hospital (Ethics Approval No. 202201002). All research objects were ensured that they were volunteering, and they could quit the research anytime. The confidentiality of their data was strictly maintained.
2.4 Intervention methods
We adopted a comprehensive approach to develop an educational program for preventing constipation in hospitalized patients. First, we conducted a thorough review of relevant literature4, 6, 9-14 on constipation prevention to gather evidence-based best practices. Second, we consulted clinical and nursing experts from the hospital's departments of gastroenterology and cardiology to obtain their professional insights and recommendations. Lastly, we integrated past practical experiences into the process of formulating the educational content. Following these steps, we devised educational materials covering various aspects including diet and fluid intake, bowel habits, medication therapy, exercise and activity, positioning in bed, continuous monitoring, family support, precautions, and emotional relief. This approach ensures the fulfillment of multifaceted needs for preventing constipation in hospitalized patients and allows for personalized customization based on individual patient circumstances.
2.4.1 Routine group interventions
The routine group shall follow established measures for preventing constipation in ACS patients as determined by the department. These measures include: (1) Daily Defecation Records: Upon admission, a detailed daily record of the patient's defecation status (frequency, stool characteristics, and the process of defecation) shall be maintained. Any notable findings should be promptly reported to the attending physician, who will provide appropriate preventive measures based on their assessment; (2) Laxative Medication Tracking: For patients prescribed laxative medications, a meticulous record of medication usage shall be maintained; (3) Dietary Assessment: A comprehensive assessment of the patient's dietary habits and structure shall be conducted, with prompt correction of any unfavorable dietary practices; (4) Constipation Education: Educational sessions shall be conducted to impart knowledge and awareness about preventing constipation; (5) Management of Severe Constipation: For patients experiencing persistent and severe constipation, the following interventions will be considered: If constipation persists for ≥48 h despite laxative use, guided abdominal massage shall be administered three times a day, with each session lasting 10–15 min; If constipation persists for ≥72 h, seluna anus insertion may be prescribed; If constipation persists for ≥96 h, a low-pressure enema will be administered.
2.4.2 Observation group interventions
In the observation group, process quality control indicators were devised and executed, and the Department's Nursing Quality Control Group convened to formulate five specific process indicators, which include:
Accuracy rate of defecation recording
This indicator calculates the percentage of patients for whom defecation conditions were accurately documented. It is expressed as follows: (Number of patients with accurately recorded defecation conditions/Total number of patients) × 100%.
Laxative medication consumption rate
This indicator evaluates the percentage of patients who were administered laxative drugs in accordance with doctor's orders after admission. This encompasses medications such as polyethylene glycol, lactulose, and self-prepared laxatives. The formula for this rate is: (Number of patients taking laxative drugs/Total number of patients) × 100%.
Implementation rate of constipation prevention education
This indicator assesses the percentage of patients who received education on constipation prevention. The formula is: (Number of patients who received constipation prevention education/Total number of patients) × 100%.
Implementation rate of physical interventions
This indicator calculates the percentage of patients who underwent physical interventions, including abdominal massage, seluna anal opening, and low-pressure enema. The formula is: (Number of patients who implemented physical interventions/Total number of patients) × 100%.
Accuracy of dietary habits and structure assessment
This indicator measures the percentage of patients who underwent an accurate assessment of their dietary habits and structure. It is calculated as follows: (Number of patients who underwent dietary habits and structure assessment/Total number of patients) × 100%.
2.4.3 Effective supervision and management of key steps in constipation prevention
Quality control nurses oversee daily process indicators for constipation prevention. If there are issues with timely implementation or accuracy, they collaborate with nursing staff, identify causes, and implement corrective plans. Weekly reports on indicator completion and patient constipation rates are sent to the department. Fishbone charts are constructed, analysis for addressing major issues, with ongoing real-time monitoring.
2.5 Evaluation methods
2.5.1 Incidence of constipation and process indicator implementation
Comparison of the incidence of constipation and the implementation of process indicators during hospitalization was conducted between the two groups. Constipation was defined as reduced frequency of defecation (<3 times per week) and the presence of hard, dry stool or difficulty in defecation.19
2.5.2 Cardiac adverse events during defecation
Compared the occurrence of cardiac adverse events during defecation between the two groups.
2.5.3 Assessment of depression levels
Changes in depression levels between the two groups were compared using the Patient Health Questionnaire-9 (PHQ-9) to assess depression. Screened for depressive symptoms by inquiring if participants had encountered various depressive symptoms within the preceding 2 weeks. Among commonly used depression scales, PHQ-920 has the highest sensitivity (95%). Each questionnaire score corresponds to five severity levels: “None” (0–4 points), “Mild” (5–9 points), “Moderate” (10–14 points), “Severe” (15–19 points), and “Extremely Severe” (20–27 points).
2.6 Statistical analysis
SPSS 26.0 software was employed for statistical analysis. Data are presented using various descriptive measures, including frequency, percentage (%), mean with standard deviation, and median with range. For qualitative data, frequency and percentage (%) were used, and the χ2 test was applied for analysis. Quantitative data, when conforming to a normal distribution, were expressed as x ± s (mean ± standard deviation). When not following a normal distribution, data were presented as median with range. All tests were bilateral, and p < 0.05 was considered statistically significant.
3 RESULTS
3.1 Participants' demographic characteristics and baseline data
The baseline survey and demographic comparison between the two groups did not differ significantly (p > 0.05), as demonstrated in Table 1.
| Variable | Observation group (n = 228) | Routine group (n = 228) | χ2/Z/t | p Value |
|---|---|---|---|---|
| Age, mean (SD), years | 62.6 (13.60) | 64.33 (12.11) | 1.032 | 0.303 |
| Male, n (%) | 179 (78.50) | 184 (80.70) | 0.256 | 0.569 |
| Education, n (%) | 2.2369 | 0.282 | ||
| Senior school or less | 181 (79.39) | 173 (75.88) | ||
| Junior college or greater | 47 (20.61) | 55 (24.12) | ||
| Marriage, n (%) | 4.677 | 0.223 | ||
| Married | 225 (98.68) | 223 (97.81) | ||
| Divorce | 2 (0.88) | 3 (1.31) | ||
| Widowed | / | 2 (0.88) | ||
| Single | 1 (0.44) | / | ||
| Emergency stent, n (%) | 94 (41.23) | 88 (38.60) | 2.170 | 0.141 |
| History of coronary intervention, n (%) | 45 (19.74) | 48 (21.05) | 1.412 | 0.235 |
| Hypertension, n (%) | 145 (63.60) | 151 (66.23) | 1.333 | 0.248 |
| Diabetes, n (%) | 87 (26.00) | 92 (25.00) | 0.026 | 0.871 |
| Heart failure, n (%) | 36 (15.79) | 39 (17.110) | 0.307 | 0.579 |
| Malignant tumor, n (%) | 32 (14.04) | 28 (12.29) | 1.006 | 0.605 |
| Chronic constipation, n (%) | ||||
| Smoking, n (%) | 104 (45.61) | 109 (47.810) | 1.225 | 0.464 |
| Defecation (%) | 3.339 | 0.198 | ||
| Smooth | 129 (56.58) | 131 (57.46) | ||
| Hard | 99 (43.42) | 97 (42.54) | ||
3.2 Comparison of the implementation rate of the defecation process index between the two groups
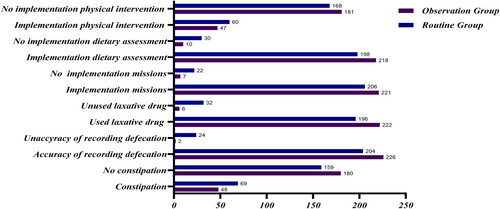
The incidence of constipation and the completion rate of process quality control indicators in the observation group were significantly superior to those in the routine group demonstrating statistically significant distinctions with (p < 0.05), as illustrated in Table 2 and Figure 2.
| n | Constipation n (%) | Accuracy of recording defecation n (%) | Laxative drug use rate n (%) | Mission implementation rate n (%) | Dietary assessment implementation rate n (%) | Physical intervention implementation rate n (%) | |
|---|---|---|---|---|---|---|---|
| Observation group | 228 | 48 (21.05) | 226 (99.12) | 222 (97.37) | 221 (96.92) | 218 (95.61) | 47 (97.92) |
| Routine group | 228 | 69 (30.26) | 204 (89.47) | 196 (85.96) | 206 (90.35) | 198 (86.84) | 60 (86.85) |
| χ2 | 2.2521 | 4.443 | 4.405 | 2.878 | 3.311 | 2.086 | |
| p | 0.024 | <0.001 | <0.001 | 0.004 | 0.001 | 0.037 |
3.3 Comparison of the incidence of cardiac adverse events between the two groups
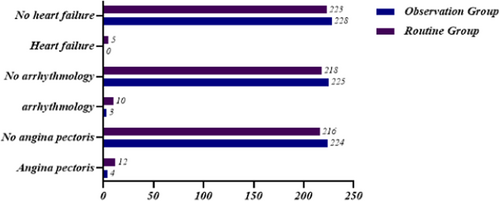
The occurrence of adverse cardiac events induced by defecation in the observation group (7 cases) was markedly reduced in comparison to those in the conventional group (27 cases). Additionally, there were no instances of heart failure events in the observation group. Importantly, neither group experienced any sudden death events. These differences were statistically significant (p < 0.05), as detailed in Table 3 and Figure 3.
| n | Cardiac adverse events | |||
|---|---|---|---|---|
| Angina pectoris n (%) | arrhythmology n (%) | Heart failure n (%) | ||
| Observation group | 228 | 4 (1.75) | 3 (1.32) | 0 (0) |
| Routine group | 228 | 12 (5.26) | 10 (4.39) | 5 (2.19) |
| χ2 | 2.036 | 1.970 | 2.248 | |
| p | 0.042 | 0.049 | 0.025 | |
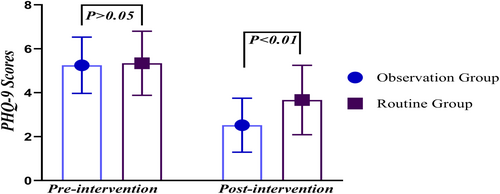
3.4 Comparison of depression levels between the two groups
Upon discharge, the PHQ-9 score in the observation group (2.52 ± 1.23) was significantly lower compared with that in the control group (3.67 ± 1.58). This difference was highly statistically significant (p < 0.01), as presented in Table 4 and Figure 4.
| Time measured | Observation group (n = 228) | Routine group (n = 228) | t (Z) | p Value |
|---|---|---|---|---|
| Preintervention | 5.25 ± 1.28 | 5.34 ± 1.46 | −0.778 | 0.437 |
| Postintervention | 2.52 ± 1.23a | 3.67 ± 1.58b | −8.672 | <0.001 |
Changes in PHQ-9 scoresc |
2.68 ± 0.89 | 1.98 ± 1.21 | 7.662 | <0.001 |
- a Compared with preintervention based on paired-sample t test, t = 23.221, p < 0.001.
- b Compared with preintervention based on paired-sample t test, t = 11.722, p < 0.001.
- c Median (range); based on nonparametric Mann–Whitney U test between two groups.
4 DISCUSSION
4.1 Process quality control indices serve as an effective guarantee of nursing quality stability and effectiveness
According to the Expert Consensus Opinion on Chronic Constipation in China (2019),21 the current prevalence of constipation in China ranges from 4.0% to 10%, and it shows a positive correlation with age. Constipation may also be linked to factors such as reduced mobility, the use of specific medications, coexisting health conditions, and diminished rectal sensory and motor function.22, 23 In this study, it was noted that the incidence of constipation was notably high, reaching 42.98% in patients diagnosed with coronary heart disease, a figure significantly higher than the 27.4% reported by Hu Chunying et al.24 This discrepancy could potentially be attributed to the mature age structure of the participants in our study. Furthermore, constipation is believed to elevate the risk of coronary heart disease. Recent cohort studies have consistently shown a markedly increased incidence of coronary heart disease among individuals with constipation undergoing medical examinations compared with those without constipation.5, 25, 26
Preventing constipation plays a pivotal role in the clinical nursing of CVDs. Process indicators serve as valuable tools for assessing and overseeing critical elements and facets of nursing measures. They also serve as scientific instruments for objectively evaluating the quality of clinical nursing and the effectiveness of nursing interventions.15, 16, 27 It represents a crucial component of nursing service quality.16 Furthermore, there exists a close causal relationship between process indicators and outcome indicators, with a strong correlation. In a study conducted by Yufei et al.,28 monitoring process indicators, such as establishing monitoring groups and clarifying indicator content, among 536 patients with acute myocardial infarction, ultimately reduced the incidence of constipation. Similarly, Li et al.29 conducted indicator monitoring on subcutaneous hematomas caused by subcutaneous injection of enoxaparin sodium, effectively preventing the occurrence of hematomas.
In this study, process indicators were incorporated into the implementation of constipation prevention measures for ACS patients to facilitate quality control supervision. The findings revealed that the occurrence of constipation in the observation group was significantly lower at 21.05% compared with the control group's 30.26% (p < 0.05). Furthermore, when compared with the control group, the observation group exhibited significantly higher completion rates for all five process indicators, demonstrating marked advantages with high statistical significance (p < 0.01). This finding aligns with the research conducted by Yang et al.,9 Chunxiang et al.30 Additionally, in the study conducted by Xiao et al.31 on sensitive indicators of orthopedic nursing quality, it was emphasized that process indicators and outcome indicators are complementary. Neglecting the evaluation and monitoring of nursing work structure or process while solely focusing on outcome indicators may result in unstable nursing quality.
4.2 Goal-oriented process quality control measures contribute to a reduction in the incidence of adverse events during bowel movements in ACS patients
Numerous prior studies have consistently established a strong association between constipation and CVDs.2, 7, 8, 32 These associations can be attributed to several factors. Patients frequently resort to Valsalva maneuvers when faced with challenging defecation,33 and felt nerous,2 and stress-induced blood pressure34 elevation amplifies the risk of adverse cardiac events. Notably, Ishiyama et al.2 highlighted that forced defecation can lead to a notable increase in blood pressure, around 20 mmHg. Recently, there has been a suggestion that constipation, characterized as a clinical manifestation of ecological disruption,35, 36 may play a partial role in the pathogenesis of atherosclerosis. This association could potentially lead to an elevated risk of coronary heart disease, ischemic stroke, and overall mortality. Therefore, our department undertook a comprehensive approach to address the impact of constipation on the prognosis of CVDs and its potential consequences in ACS patients.
In January 2021, our department initiated a program aimed at establishing sensitive indicators for preventing and managing constipation in patients with ACS. As part of this initiative, patients admitted with ACS were prescribed laxative medications, and proactive measures were implemented to prevent constipation, including patient education and dietary evaluation. Despite these efforts, there were instances of constipation and associated cardiac complications, which highlighted a need for better process control. In response to these challenges, our study shifted its focus toward preventing constipation as the primary goal. We implemented a more rigorous quality control and process management system while closely monitoring changes in patients' conditions. Timely predictions and treatments were administered as needed. As a result, there were no instances of sudden cardiac events in either group of patients, and the experimental group did not experience any cases of heart failure. Additionally, the incidence of cardiac adverse events was significantly lower in the experimental group compared with the control group.
4.3 The implementation of nursing quality control can reduce the depression of ACS patients, and also enhance the comprehensive abilities of nurses
Research findings indicate that patients with ACS not only grapple with physical health issues but also face substantial mental health challenges. According to previous studies, approximately 20% of individuals with coronary heart disease report experiencing psychological symptoms such as depression and anxiety.37 Furthermore, mental health problems have been recognized as independent risk factors for worsening coronary heart disease, with anxiety and depression symptoms associated with a 1.6-fold increase in all-cause mortality among coronary heart disease patients.38 Moreover, several studies39, 40 have consistently revealed that a significant proportion of ACS patients exhibit concurrent symptoms of depression and constipation, indicating a correlation between these two conditions. The acute onset of ACS serves as a potent psychological stressor for patients, particularly those experiencing it for the first time. This stress-induced situation may result in elevated catecholamine levels in the body, exacerbating depressive symptoms. Simultaneously, it can lead to autonomic dysfunction and a reduction in gastrointestinal peristalsis, ultimately leading to constipation.41 Notably, constipation itself has been linked to heightened levels of anxiety, depression, and a diminished quality of life.42
In this study, it was found that 32.02% of patients in the observation group and 32.98% in the conventional group exhibited depressive symptoms before intervention, which slightly lower than Ozer et al.39 reported 34%–36.5%. Therefore, addressing constipation and mental health issues should be integral to the treatment of patients with ACS. The study's results demonstrated that patients in the observation group had significantly lower PHQ-9 scores at discharge than those in the control group. This improvement was attributed to effective and timely communication between nurses and patients, as well as a substantial reduction in constipation incidence observed during the study. Additionally, the continuous monitoring of process indicators throughout the research facilitated the early identification of issues and enabled root cause analysis and improvement. This approach not only enhances nurses' theoretical knowledge and educational skills but also bolsters their problem-solving abilities.
4.4 Limitations
This study has certain limitations that should be taken into account when interpreting the results. First, patient self-reported measures, such as bowel movements, were utilized. However, we recognize the inherent reliability challenges associated with patient self-reporting. Factors like memory biases and subjective perceptions may lead to potential inaccuracies. Despite our attempts to validate patient self-reports using medical records and other means, these methods also have limitations. Second, the study was conducted during the COVID-19 pandemic, and due to the challenges posed by the outbreak, sampling was limited to a single hospital. Additionally, the study's sample size was not large enough. Therefore, future research should place greater emphasis on patient self-reported data and consider adopting more effective methods to assess the reliability and accuracy of such data, such as conducting reliability and validity tests. Additionally, exploring similar studies across multiple medical centers could help address these limitations.
5 CONCLUSION
In summary, the effectiveness of goal-oriented process quality control management in preventing constipation among hospitalized patients with acute ACS. It not only significantly reduces the incidence of constipation but also minimizes adverse cardiac events during constipation episodes and alleviates depressive symptoms in patients. Therefore, the establishment of quantitative criteria and objective evaluation methods is crucial for healthcare providers to ensure the effectiveness of constipation prevention measures.
AUTHOR CONTRIBUTIONS
Xing Miao and Hui Jiang carried out the studies. Xing Miao performed the analyses. Yan Zheng and Xiufang Huang were in charge of coordination and direct implementation. Yan Zheng collected the data. Xing Miao drafted the manuscript. Xing Miao and Hui Jiang conceived and designed the study. All authors contributed to editing the draft of the manuscript and have approved the final manuscript.
ACKNOWLEDGMENTS
The authors would like to extend their gratitude to all the staff in the Department of Cardiology, Fujian Provincial Hospital for their valuable assistance in this project. This work was supported by a grant from the Natural Science Foundation of Fujian Province (Grant No. 2022J01418).
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Hui Jiang affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
All authors have read and approved the final version of the manuscript. Hui Jiang had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis. All the data and materials are available, the authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.