Activity counseling early postelective percutaneous coronary intervention (ACE-PCI): Mixed-methods pilot randomized controlled trial
Australian New Zealand Clinical Trials Registry (ANZCTR): ACTRN12621000927820p, https://www.anzctr.org.au/ACTRN12621000927820p.aspx, Registered July 15, 2021.
Abstract
Background
Physical activity (PA) levels of people with coronary heart disease are low in the first 30 days after percutaneous coronary intervention (PCI), increasing the risk of recurrent cardiac events. Following PCI, PA counseling delivered by a physiotherapist before discharge may increase the PA levels of patients. Preliminary work is required to determine the effects of the counseling session compared to usual care.
Objectives
To investigate the feasibility and potential efficacy of a brief physiotherapist-led PA counseling session immediately after an elective PCI compared to usual care for improved PA early post-PCI.
Methods
Using concealed allocation and blinded assessments, eligible participants (n = 30) were randomized to a physiotherapist-led PA counseling session (30 min) or usual care (nurse-led PA advice < 5 min). The primary outcome was daily minutes of moderate-to-vigorous PA (accelerometry; 3 weeks). Secondary outcomes included cardiac rehabilitation intention, anxiety and depression levels (Hospital Anxiety and Depression Scale), and quality-of-life (MacNew questionnaire). Recruitment, retention, and attrition were assessed for feasibility. Semistructured interviews were conducted with 13 participants to determine intervention acceptability, and barriers and enablers to PA.
Results
Between and within-group comparisons were not significant in intention-to-treat analyses. All feasibility criteria were met except for retention and attrition of participants. At 3 weeks, only 25% of participants were planning to attend cardiac rehabilitation, with no between-group differences. Increased PA at 3 weeks was associated with participants that were younger, without other chronic disease,s and more active immediately following discharge. Interviews revealed personal, environmental, and program-based themes for barriers and enablers to PA.
Conclusions
A physiotherapist-led PA counseling session may not improve PA levels early post-elective PCI compared to very brief PA advice delivered by nurses. A larger multicentre randomized controlled trial is feasible with minor modifications to participant follow-up. Further research is required.
1 INTRODUCTION
Percutaneous coronary intervention (PCI) is the most used procedure for myocardial revascularisation globally.1, 2 International guidelines for the management of acute coronary syndrome (ACS; heart attack and unstable angina) recommend that individuals hospitalized with ACS, including those undergoing a PCI, receive physical activity (PA) counseling and referral to a cardiac rehabilitation program before discharge.3, 4 Increased PA and exercise-based cardiac rehabilitation are associated with positive health benefits for people with ACS such as reduced cardiac and all-cause mortality, reduced risk of hospital readmission, and improved aerobic capacity.5, 6 However, nearly half of ACS patients (84% post-PCI) do not exercise at all during Weeks 2–5 postdischarge7 and cardiac rehabilitation attendance is low.8
To identify best practices and factors that may influence outcomes, international comparisons are useful to provide a broader perspective of health and healthcare.9 Using the same methods, device-measured PA was compared in Australia and Sweden approximately 3-weeks post-PCI.10 Swedish PCI participants completed more moderate-to-vigorous physical activity (MVPA) than Australian participants. Swedish ACS patients typically receive a 30-min physiotherapist-led PA and exercise counseling session before discharge,11 which may explain the difference in MVPA. Physiotherapists are well-placed to promote PA, treating and considering any underlying conditions that may impair someone's physical capacity to be physically active. In Australian and New Zealand hospitals, it has been reported that less than half of ACS patients receive PA advice before discharge,12 with post-PCI PA advice usually very brief (<5 min) delivered by cardiology nurses.
Currently, it is not clear in Australian ACS guidelines how much PA advice before discharge should be provided, whether it should include written advice, and who should provide the lifestyle counseling. Further investigation is required of post-PCI PA advice in Australia, which may impact postdischarge activity levels, decreasing the risk of recurrent cardiac events. Therefore, the aims of this pilot randomized controlled trial were to (i) examine whether a 30-min physiotherapist-led PA counseling session before discharge improves accelerometer daily minutes of MVPA over 3 weeks compared to <5-min nurse-led PA advice (usual care) in a sample of Australian adults' postelective PCI; and (ii) determine the feasibility of the study protocol.
2 METHODS
2.1 Design and study setting
A pilot (two parallel arms, 1:1 allocation ratio) mixed-methods randomized controlled study was conducted in one Australian private hospital. Using a computer-generated random number sequence and concealed group allocation (sealed, consecutively numbered opaque envelopes), participants were randomized after their baseline assessment to one of two groups: physiotherapist-led PA counseling or usual care. The Consolidated Standards of Reporting Trials statement: extension to randomized pilot and feasibility trials and Good Reporting of A Mixed Methods Study checklist were used to guide reporting (File S1).
2.2 Inclusion and exclusion criteria
Eligible participants were aged ≥ 18 years with stable coronary heart disease (CHD) who received an elective PCI ± myocardial infarction. Cardiology nursing staff recruited participants following their PCI. Participants were excluded if they had a primary diagnosis of atrial fibrillation, New York Heart Association class II–IV symptoms of heart failure, uncontrolled arrhythmias, severe chronic obstructive pulmonary disease, uncontrolled hypertension, symptomatic peripheral artery disease, unstable angina, uncontrolled diabetes, inadequate English language, and cognitive skills, and were unable to walk or wear an accelerometer due to disability. All eligible participants received an Australian Heart Foundation booklet and were referred to a comprehensive (exercise and education) cardiac rehabilitation program. The average length of stay in the hospital following a PCI is 1–2 days.1
2.3 Interventions
2.3.1 Physiotherapist-led PA counseling
The intervention group received a 30-min PA counseling session from a single physiotherapist before discharge. The main purpose of the session was to encourage PA immediately after discharge, according to the participant's medical status and preferences, recommending light-to-moderate PA which could be progressed gradually. The benefits of PA, the PA guidelines post-PCI according to the frequency, intensity, time, and type principle, and individual barriers and enablers of PA were discussed, including the level of confidence to be physically active, as well as safety measures such as the warning signs of a heart attack. Individuals undertaking secondary prevention post-PCI are encouraged to meet the public health PA guidelines to improve health outcomes.13 The World Health Organization PA guidelines for adults with chronic disease recommend that individuals should complete 150–300 min of moderate-intensity aerobic PA; or 75–150 min of vigorous-intensity aerobic PA or a combination of both per week.14 MVPA should be completed on most days per week (frequency) and a variety of MVPA (type) is recommended including domestic, occupational, transportation, and leisure activities, noting any activity is better than none. Comprehensive cardiac rehabilitation was promoted, outlining that exercise screening would be performed at the start of the program allowing a more individually tailored exercise prescription. The physiotherapist then collaborated with the participant to design and provide them with a written individualized PA program outlining their goals; initial PA frequency, intensity, duration, and type according to their preferences; progression of their PA program; and monitoring of the participant's PA intensity and symptoms. The physiotherapist delivering the intervention received 2 h of training before participant recruitment with one of the research team members, an experienced cardiac rehabilitation clinician and teaching and research academic trained in adult education and behavior change counseling. The physiotherapist had been practicing clinically for 16 years in acute and rehabilitation hospital settings and had 6 years' of experience working in both acute cardiac care and cardiac rehabilitation. No changes to the delivery of the counseling session were made due to the COVID-19 pandemic.
2.3.2 Usual care
Usual activity advice after a PCI was provided by a cardiology nurse in <5 min, that is, no heavy lifting, pushing, or pulling for 1 week. Gentle walking on flat surfaces was encouraged for the first week then gradually increasing walking over the following few weeks.
2.4 Outcome measures
Outcome measures were collected at baseline and 3-weeks post-PCI. The assessor at baseline was blinded to group allocation and trained in all measurement procedures. To maintain blinding at 3 weeks no assessors directly collected data, with participants mailed an accelerometer and questionnaires.
The primary outcome measures were daily minutes of MVPA measured using a triaxial commercial accelerometer (ActiGraph GT3X) and feasibility. Participants wore the accelerometer on their right hip during waking hours for 7-consecutive days. All data was downloaded as raw data (30 Hz), converted to 15-second epochs (time interval), and then counts per minute (cpm) using the Actilife software. Data was excluded if: <10 h per day wear time and <4 days of valid data. The Sasaki vector magnitude 3 cut-point was used to determine time spent in MVPA (≥2690 cpm).15 To measure sedentary behavior, the vector magnitude cut-point was used (<150 cpm), categorizing light PA as 150–2689 cpm. Estimating daily time spent in PA and sedentary behavior was calculated by dividing the total time spent (minutes) in each threshold by the number of valid days. Adherence to the PA recommendations, 150 min of MVPA per week (sufficient time), was calculated based on estimates of daily minutes in MVPA and multiplied by 7 to estimate a week. Feasibility was defined as recruitment, retention, and attrition (≤25% participants lost to follow-up), and acceptability (semistructured interviews) of the brief physiotherapist-led PA counseling intervention.
Secondary outcomes included self-reported cardiac rehabilitation attendance intention, anxiety and depression levels (Hospital Anxiety and Depression Scale16, 17: score between 0 [best outcome] and 21 [worst outcome] for either anxiety or depression) and quality-of-life (MacNew questionnaire18: maximum possible score in any domain is 7 [high health-related quality of life], and the minimum, 1 [poor health-related quality of life]). At 3 weeks, semistructured interviews via phone or Zoom (30 min) were conducted by two research team members (A. F., S. J. C.) with participants in both groups to determine barriers and enablers to PA early in their recovery and the acceptability of the intervention (File S2). Interviewing participants continued until no new concepts or categories were formed and there was no need for further elaboration of the concepts or categories. All interviews were audio-recorded and professionally transcribed, and transcripts were returned to participants for member checking.
At baseline, clinical and sociodemographic information was collected with questions regarding the participant's education level, relationship status, current employment status, and the presence of any other chronic diseases. Height and weight were taken using a standardized set of scales and a stadiometer. PA levels over the last 12 months were self-reported using the CARDIA Physical Activity History (PAH), asking about participation in 13 specific MVPA activities (8 high-intensity activities; 5 moderate-intensity activities) over the previous year, including sports, exercise, home maintenance, and occupational activities.19, 20 The PAH is scored in exercise units (EUs) representing a weighted sum of intensity, duration, and frequency of the activity over the previous year. The total score reflects all 13 activities and a score of 300 EUs approximates the public health recommendations of at least 150 min of MVPA per week.21
2.5 Sample size
An important purpose of this study was to provide an estimate of the potential effect size of providing a physiotherapist-led PA counseling session before discharge post-PCI on PA levels. There is no prior appropriate data assessing the change in PA levels using accelerometry on which to base a sample size estimate for this comparison with usual care. Therefore, the study sought to recruit 30 participants for this purpose. Data from this study will be used to inform planning for future studies.
2.6 Data analysis
Analyses were carried out following intention-to-treat principles. For missing data at 3 weeks, no change from baseline was assumed. In addition, a less conservative approach (per-protocol analysis) was completed using only participants who provided baseline and 3-week data. The normality of the data was assessed using the Shapiro–Wilk test. For between-group analyses, unpaired t tests and the Mann–Whitney U test were used, using χ2 analysis for categorical data. For within-group analyses, changes in variables were analyzed with paired t tests or Wilcoxon signed-rank tests. Associations between PA at 3 weeks and outcome measures were assessed using Spearman correlations (ρ). All analyses were conducted using SPSS version 27. The significance level was set at p < 0.05.
The qualitative data analysis was based on Braun and Clarke's thematic analysis approach.22 Two experienced qualitative research team members independently coded four transcripts using inductive data analysis (S. J. C., N. F.). The identified codes were discussed between the researchers (S. J. C., N. F.) to compare understandings of the content and definitions behind each code and then the remaining transcripts were coded by both researchers. Generated themes and subthemes from the codes were then discussed and categorized as a barrier or an enabler to PA. Subthemes were deductively categorized into personal, environmental, and program-level barriers and enablers as these factors need to be considered when designing PA programs to maximize adoption and maintenance,23 including consideration of intervention acceptability. Using both thematic analysis and framework analysis enabled the researchers to identify potential barriers and enablers to PA early post-PCI, informing the acceptability and feasibility of the inpatient physiotherapist-led PA counseling session in future studies.
3 RESULTS
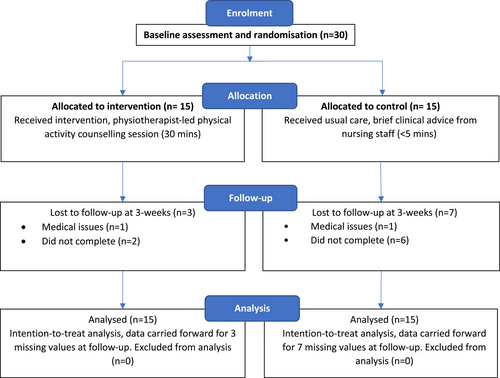
Thirty participants were recruited between September 2021 and July 2022 (Figure 1). Recruitment was interrupted by COVID-19 restrictions, with elective PCIs reduced at times during 2021–2022. Most participants were male, born in Australia, not working in the labor force, tertiary educated, in a relationship, and were non-smokers without type 2 diabetes (Table 1). Half of the participants had one other chronic disease (apart from heart disease or type 2 diabetes) such as chronic lung disease or osteoarthritis. Participants mean age was 67 ± 10 years, ranging from 41 to 82 years. On average, participants self-reported they were exceeding the public health PA guidelines over the last 12 months. Twenty-nine participants provided valid accelerometer results at baseline and 19 participants at 3 weeks. At 3 weeks, 67% (20/30) of participants completed assessments (Figure 1).
| Characteristic | Intervention (n = 15) | Control (n = 15) |
|---|---|---|
| Age (years), mean (SD) | 67.7 (10.2) | 65.9 (10.4) |
| Gender, n male (%) | 12 (80) | 11 (73) |
| Country born, Australia n (%) | 12 (80) | 10 (67) |
| BP meds, yes n (%) | 11 (73) | 12 (80) |
| Cholesterol meds, yes n (%) | 13 (87) | 12 (80) |
| Employment, not in labor force n (%) | 10 (67) | 6 (40) |
| Relationship status, n partner (%) | 12 (80) | 11 (73) |
| Education level, n tertiary (%) | 9 (60) | 10 (67) |
| Current smoker, n no (%) | 14 (93) | 14 (93) |
| Type 2 diabetes, n no (%) | 10 (67) | 13 (87) |
| Other chronic disease, nil n (%) | 7 (50) | 7 (54) |
| Measures of disease risk | ||
| Body mass index (kg/m2), mean (SD) | 30.1 (4.7) | 30.4 (6.4) |
| CARDIA PAH (self-reported) | ||
| Moderate intensity score (EU) | 226 (163) | 215 (125) |
| High-intensity score (EU) | 148 (145) | 329 (312) |
| Total physical activity (EU) | 418 (208) | 586 (301) |
| Television viewing (h/day) | 3.5 (1.9) | 3.7 (2.4) |
- Abbreviations: BP, blood pressure; CARDIA PAH, CARDIA Physical Activity History questionnaire; EU, exercise units; med, medications.
The intention-to-treat analysis indicated no significant difference between or within groups in device-measured PA levels at 3 weeks, except for the decreased number of sedentary bouts and breaks within the usual care group (p = 0.017) (Table 2). Per-protocol analyses found similar results. At baseline, 24% (n = 7/29; 4 intervention, 3 usual care) of participants were insufficiently active, with 32% (n = 6/19; 3 intervention, 3 usual care) insufficiently active at 3 weeks. The effect size for increasing daily minutes of device-measured MVPA during this study was small (Cohen's d = 0.4). The sample size needed to detect a change of this magnitude between groups, with a two-sided significance of p < 0.05 and power of 80%, is a minimum of 200 participants (100 in each group), calculated using G*Power version 3.1.9.4.
| ActiGraph 15s | Groups | Difference within groups | Difference between groups Week 3 | ||||
|---|---|---|---|---|---|---|---|
| Week 0 | Week 3 | Week 3 minus Week 0 | |||||
| Int (n = 14) | Con (n = 15) | Int (n = 14) | Con (n = 15) | Int | Con | Int minus Con | |
| MVPA min/day | 41 (22.6) | 50.4 (31.9) | 42.3 (24.5) | 54.4 (35.7) | 1.3 (8) | 4 (13.2) | −12.1 (−35.4 to 11.3) |
| LPA min/day | 226 (57) | 225 (47) | 223 (54) | 231 (54) | −2.6 (28.7) | 5.4 (32.8) | −7.6 (−49.1 to 33.9) |
| Sedentary min/day | 578 (154) | 556 (85) | 588 (157) | 543 (92) | 9.5 (61) | −14 (47) | 44.9 (−52.2 to 142.1) |
| Duration sedentary bouts/day (min) | 21 (3) | 20 (4) | 22 (2) | 21 (5) | 0.7 (2.4) | 0.7 (2.3) | 0.8 (−2.1 to 3.6) |
| Number of sedentary bouts/day | 13 (5) | 12 (4) | 14 (6) | 11 (4) | 1.1 (3.1) | −1.1 (1.6)* | 2.5 (−1.4 to 6.5) |
| Number sedentary breaks/day | 12 (5) | 11 (4) | 13 (6) | 10 (4) | 1.1 (3.1) | −1.1 (1.6)* | 2.5 (−1.4 to 6.4) |
| Wear time min/day | 856 (179) | 832 (74) | 853 (169) | 828 (89) | −3.3 (5.7) | −4.4 (4.5) | 24.8 (−78.2 to 127.8) |
| VM counts/day | 364,477 (122,424) | 406,757 (153,691) | 368,874 (126,277) | 430,096 (187,861) | 4397 (36,317) | 23338 (79,619) | −61221 (−183,017 to 60,573) |
| Steps/day | 5578 (2242) | 5706 (3218) | 5310 (2234) | 6007 (3458) | −267 (751) | 301 (1154) | −696 (−2913 to 1520) |
- Abbreviations: CI, confidence interval; Con, control group; Int, intervention group; LPA, light physical activity; MVPA, moderate-to-vigorous physical activity; VM, vector magnitude.
- * p = 0.017.
There were no differences at 3 weeks between or within groups for quality-of-life, anxiety, and depression (Table 3). However, there was a trend for anxiety levels to improve within participants that received the PA counseling session (p = 0.056, effect size = 0.49).
| Outcome | Groups | Difference within groups | Difference between groups | ||||
|---|---|---|---|---|---|---|---|
| Week 0 | Week 3 | Week 3 minus Week 0 | Week 3 | ||||
| Int (n = 15) | Con (n = 15) | Int (n = 15) | Con (n = 15) | Int | Con | Int minus Con | |
| MacNew Global, mean (SD) | 4.8 (1.1) | 5.2 (0.8) | 5.2 (1.2) | 5.5 (0.7) | 0.4 (0.8) | 0.3 (0.5) | −0.24 (−0.97 to −0.50) |
| MacNew Physical, mean (SD) | 4.6 (1.3) | 4.8 (1) | 5.2 (1.3) | 5.1 (1) | 0.6 (1.1) | 0.3 (0.7) | 0.08 (−0.76 to 0.92) |
| MacNew Emotional, mean (SD) | 4.8 (1) | 5.5 (0.6) | 5.2 (1.2) | 5.7 (0.6) | 0.4 (0.8) | 0.2 (0.4) | −0.50 (−1.2 to 0.21) |
| MacNew Social, mean (SD) | 5.1 (1.2) | 5.3 (1.1) | 5.4 (1.3) | 5.7 (1) | 0.3 (0.8) | 0.4 (0.8) | −0.29 (−1.1 to 0.54) |
| HADS-Anxiety, median (Q1, Q3) | 7.1 (5.8) | 5.2 (2.2) | 5.4 (4.8) | 5.1 (1.6) | −1.6 (2.9) | −0.07 (1.3) | 0.3 (−2.6 to 3.1) |
| HADS-Depression, median (Q1, Q3) | 5 (5.9) | 3.3 (1.9) | 3.4 (2.9) | 3.4 (1.8) | −1.6 (5.7) | 0.13 (1.8) | 0 (−1.8 to 1.8) |
| HADS-total, median (Q1, Q3) | 12.1 (10.7) | 8.5 (2.9) | 8.9 (7.1) | 8.5 (3.1) | −3.1 (7.9) | 0.07 (2.2) | 0.4 (−3.8 to 4.6) |
- Note: MacNew, MacNew quality-of-life questionnaire.
- Abbreviations: CI, confidence interval; Con, control group; HADS, Hospital Anxiety and Depression Scale; Int, intervention group.
Three participants visited the emergency department in the 3-week follow-up period (1 intervention, 2 usual care), and one intervention participant was admitted to the hospital twice with cardiac and noncardiac medical issues. Only one in four participants was planning to attend a cardiac rehabilitation program, with no difference between groups (intervention, 2/11; usual care 3/8).
Increased PA at 3 weeks was associated with younger participants (ρ = −0.44, p = 0.02), participants without type 2 diabetes (ρ = −0.51, p = 0.004) or other chronic disease (ρ = −0.39, p = 0.047) and participants with higher device-measured PA immediately following discharge (ρ = 0.95, p < 0.001).
3.1 Qualitative data
My physical capacities have been more limited by my problem with my knee, than the heart itself. (ACE18, usual care, male 77 years)
doing things where I'm not near the hospital sort of bothers me. (ACE6, usual care, male, 62 years)
I get a bit worried and go to various doctors, but what they tend to tell you is in conflict to each other. (ACE13, usual care, male, 73 years)
certainly having a person to do it with, either a… you know, someone to sort of take me along or someone who comes along with me. I don't feel that comfortable doing any of it on my own. So, you know, certainly one enabler is finding somebody to do it with me. (ACE6, usual care, male, 62 years)
Environmental enablers were being physically active where participants felt safe (e.g., in populated areas closer to health services) and in good weather. Receiving a tailored exercise program from a health professional, and doctors advising patients to be physically active were program-based enablers.
3.2 Acceptability of the interventions and need for cardiac rehabilitation
Well, I identified with the physiotherapist that you know I'd been through all this post bypass physiotherapy, and I'd benefited from that, and I didn't think that she was in a position to offer me any other benefits, yeah. (ACE7, intervention, male, 72 years)
I had one of the physiotherapists talk to me, she gave a kind of a plan sort of how to escalate things slowly. And I'm trying to do that first, and see how things go. (ACE27, intervention, male, 49 years)
So I just, it was very generic, and I just didn't know how literally to take it. (ACE3, usual care, female, 74 years)
Participants, both intervention and usual care, reported cardiac rehabilitation was not routinely offered and if it was, participants felt that they were not a priority for this program, and it would be more useful for others.
4 DISCUSSION
A physiotherapist-led PA counseling session did not make a difference to device-measured PA levels in the first 3 weeks of postelective PCI or intention to attend cardiac rehabilitation. However, targeted patient-centered PA advice, such as intensive PA counseling, may be particularly required for patients that are older, less active, and with multiple co-morbidities according to the mixed methods result. A larger multicenter randomized controlled study is feasible for this study protocol as all feasibility criteria were met except for retention and attrition of participants which can be addressed with a blinded in-person assessor or increased remote support at follow-up.
Limited studies have considered PA levels within the first 30 days after hospitalization for ACS ± PCI, with very few evaluating the change in PA from discharge to 30 days. Studies that have, reported low patient PA levels, with 56%–93%24-27 not meeting the PA guidelines and 40% of patients following an ACS event not completing 30 min of MVPA on any day in the first 5 weeks postdischarge.7 Older patients (≥75 years) following a PCI for ACS have also been found to have lower MVPA levels and higher levels of sedentary behavior compared with postelective (stable angina) PCI patients.24 A limitation of these comparisons is that measurement of PA differs between studies, with some using self-report26, 27 and others using devices.24, 25 Regardless, activity levels appear to be low and unchanged in patients early post-PCI. Considering this lack of change, 3 weeks may be too soon to observe PA changes despite this being a critical period when health behaviors may be influenced, although improvements in PA have been reported at 3 months following an ACS event27 and up to 6 months in cardiac rehabilitation populations.25
Sedentary behavior was high in this cohort (>9 h/day) and did not change over 3 weeks, similar to previous studies within the first 30 days post-ACS event.10, 28 Device measured sedentary behavior greater than 7.5 h/day is associated with an increased risk of all-cause mortality.29 Additionally, participants self-reported they were watching television > 3.5 h/day on average over the last 12 months. Television viewing, a proxy for sedentary behavior, is associated with all-cause mortality in adults with CVD.30 Compared to 2 h, self-reported television viewing greater than 2 h/day increases risk of all-cause mortality in people with CVD, placing post-PCI patients at high risk of death from any cause.30
The associations found between higher PA levels and age, baseline activity and multiple co-morbidities are supported by the qualitative data. This is consistent with the correlates and determinants of PA in patients post ACS ± PCI7, 27 and in the general adult population.31 In Australia, survival post-PCI has remained relatively stable from 2002 except for the 2014-to-2016 period where there was a decrease in survival, potentially due to risk factors for CHD prevention, such as physical inactivity.32 Trends in PCI have seen a decrease in length of stay and an increase of PCIs in the older population.33 This is particularly relevant considering the association we found with age and activity level post-PCI. Older age34 and comorbidities34-36 have been associated with unplanned hospital admissions within the first 30 days post-PCI, with readmission rates up to 17%.34, 36, 37 Additionally, in-hospital cardiovascular events during a hospitalization for ACS are 2.5 times more likely to occur in inactive patients compared with active patients, with in-hospital complications having a stronger association with physical inactivity than length of hospital stay.26 Thus, there is a need for effective PA interventions post-PCI, particularly for those that are older, with co-morbidities and low baseline levels of activity to prevent readmissions and improve survival.
As found within the qualitative data, time, motivation, social support, and enjoyment are common determinants of PA.31 Neighborhood design is also a determinant of PA31 and this seems particularly relevant to our participants that have a fear of subsequent cardiac events and express a need to be active in a space that is close to medical facilities. High levels of kinesiophobia, or fear of movement, have been found in 20% of patients with coronary artery disease and is associated with low levels of PA.38, 39 Our findings indicate that increased support and discussion of fear or confidence to be active should be included in future inpatient physiotherapist-led PA counseling sessions which may improve patient PA levels early in their recovery post-PCI. Conflicting messages from health professionals were found to be a program-based barrier to PA. This has been reported for cardiac rehabilitation attendance, with contradictory messages in the hospital and the physician not recommending cardiac rehabilitation barriers to attendance.40 Increased education for cardiac health professionals on PA guidelines is recommended to avoid conflicting information, using a patient-centered approach, behavior change techniques, and shared decision-making, with this information included in ACS guidelines. Additionally, cardiac rehabilitation messaging needs to be clear and consistent to improve attendance rates, as similar to our study, in Australia only 28% of patients referred are attending cardiac rehabilitation.8
5 LIMITATIONS
In this pilot study, the sample size was small, and the attrition rate was high, therefore, the results should be interpreted with caution. To improve the attrition rate, an assessor collection of data may be needed. This was also a single-center study, conducted in a private hospital where most participants were tertiary-educated men, limiting the generalizability of the results. Participants were also not excluded if they were already meeting the PA guidelines before inclusion in the study, which may have limited improvements in PA levels. For the qualitative data, the voluntary sample of interview participants may not represent the perceptions of all patients post-PCI or within this study, creating a selection bias. Additionally, the physiotherapist delivering the intervention may have required increased training on PA counseling post-PCI, including the use of behavior change techniques and tools, such as motivational interviewing.
6 CONCLUSION
A physiotherapist-led PA counseling session may not improve PA levels in the first 30 days postelective PCI compared to very brief PA advice delivered by nurses. Further research is feasible and is needed in nonelective PCI, public patient samples; with larger sample sizes and longer follow-up to determine whether the physiotherapist-led PA counseling session results in the increased adoption and maintenance of PA post-PCI, particularly in older, less active patients with co-morbidities.
AUTHOR CONTRIBUTIONS
Nicole Freene: Conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; supervision; writing—original draft; writing—review and editing. Suzanne J. Carroll: Data curation; formal analysis; funding acquisition; investigation; methodology; writing—review and editing. Allyson Flynn: Data curation; formal analysis; funding acquisition; investigation; methodology; writing—review and editing. Sarah Bowen: Data curation; investigation; methodology; writing—review and editing. Roslyn Holley: Data curation; investigation; methodology; writing—review and editing. Kerry Rodway: Data curation; investigation; methodology; writing—review and editing. Theo Niyonsenga: Formal analysis; funding acquisition; investigation; methodology; writing—review and editing. Rachel Davey: Funding acquisition; investigation; methodology; writing—review and editing.
ACKNOWLEDGMENTS
The authors would like to thank all participants in this study and the staff at National Capital Private Hospital who provided support during the angiotensin-converting enzyme-percutaneous coronary intervention trial, recruiting all participants (cardiology nurses), collecting baseline data (ward clerk), and delivering the physical activity counseling session (physiotherapist) and brief advice (cardiology nurses). Sincere thanks to Kacie Patterson, the research assistant for this trial. Funding for this study was provided by a University of Canberra Faculty of Health Seed Grant. Open access publishing facilitated by University of Canberra, as part of the Wiley - University of Canberra agreement via the Council of Australian University Librarians.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
All potential participants were required to read a plain language information statement describing the study. They were then asked to provide written consent to participate in the study, including participating in the semistructured interview at the end of the 3-week data collection period. To confirm their initial consent to an interview at 3 weeks, secondary verbal consent was obtained before each follow-up interview. Ethics approval was obtained from the University of Canberra Human Research Ethics Committee (HREC-9190).
TRANSPARENCY STATEMENT
The lead author Nicole Freene affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The datasets used and analyzed during the study are available from the corresponding author upon reasonable request.