Self-help application for obsessive-compulsive disorder based on exposure and response prevention technique with prototype design and usability evaluation: A cross-sectional study
Abstract
Background and Aims
Obsessive-compulsive disorder (OCD) is a relatively common disorder that, due to its debilitating nature, significantly affects personal abilities, job performance, social adjustment, and interpersonal relationships. There are significant barriers to accessing evidence-based cognitive-behavioral therapy as a first-line treatment for obsessive-compulsive disorder. Mobile health applications (Apps) offer a promising way to improve access to evidence-based therapies while overcoming these barriers. The present study was to design and evaluate a prototype of a self-help application for people with OCD (the most common pattern of OCD) based on the exposure and response prevention (ERP) technique.
Methods
This work was developed in four different phases. (1) Needs assessment: a thorough literature review, reviewing existing related programs and apps, and interviewing patients and psychiatrists; (2) Creating a paper prototype: considering the functional features identified in the previous phase using wireframe sketcher software. (3) Creating a digital prototype: developing an actual prototype using Axure RP software based on the information obtained from an expert panel's evaluation of the paper prototype. (4) Prototype usability evaluation: through a heuristic evaluation with experts and usability testing with patients using the SUS questionnaire.
Results
After requirement analysis, requirements were defined in the areas of information and educational elements, and functional capabilities. Prototypes designed based on identified requirements include capabilities such as in-app online self-help groups, assessing the severity of the symptoms of the disorder, psychological training, supportive treatment strategies, setting personalized treatment plans, tracking treatment progress through weekly reports provided, anxiety assessment, and setting reminders.
Conclusion
The results of the heuristic evaluation with experts made it possible to identify how to provide information and implement the capabilities in a way that is more appropriate and easier for the user.
1 INTRODUCTION
Obsessive-compulsive disorder (OCD) is a common and disabling anxiety disorder characterized by recurrent, intrusive, unwanted thoughts, images, or urges that cause anxiety or distress and are usually followed by repetitive behaviors, rituals, or mental acts used to decrease anxiety.1
It is the fourth most common psychiatric disorder after phobias, addictions, and depression2 and the 10th leading cause of disability, according to the World Health Organization.3 The prevalence estimated for OCD is about 1%–3% globally, with a rate higher in the developed world at 2%–3%,4-6 and is associated with substantial reductions in health-related quality of life,7, 8 as well as impairments in education, social relations, and family functioning.9 According to a recent study that investigated significant anxiety disorders in Iran, the 12-month prevalence of OCD in Iran is 5.1% and is the second most common anxiety disorder.10 Contamination OCD is the most common pattern of obsessive-compulsive disorder, followed by excessive or ritualistic washing or severe avoidance of things that are assumed to be contaminated,11, 12 which accounts for approximately a quarter of all obsessive themes in the United States and is the most common OCD concern worldwide.13
Despite the disability associated with symptoms, most individuals with OCD delay seeking treatment.14 If untreated, OCD usually involves a recurrent period and becomes chronic.15 Therefore, early diagnosis and treatment are essential for long-term outcomes and the prevention of prolonged suffering.16
The first-line nonpharmacological treatment for a type of OCD is a form of cognitive-behavioral therapy (CBT) called “exposure and response prevention (ERP).” Studies documenting the benefits of ERP treatment have found that over 75% of patients experience improved OCD symptoms during treatment. The majority show long-term improvement 2–3 years after treatment. Several meta-analyses and clinical significance analyses indicate that 60%–80% of patients who complete treatment with ERP, particularly those who engage in treatment with compliance and motivation, get significantly better.17
Despite strong empirical support for ERP and its effectiveness in treating OCD patients,14, 18 many affected patients do not have access to this treatment.19, 20 Geographic isolation, restricted access to qualified therapists who are skilled in the treatment of anxiety disorders, direct and indirect costs of treatment, fear of stigmatization or discrimination, logistic issues such as conflicts with work, limited time, and scheduling difficulties are significant barriers to receiving such evidence-based psychotherapies (EBPs).20-24 Consequently, it is essential to innovate approaches to improve access to such evidence-based psychotherapy.
Remote treatment via technology-based interventions (TBIs), including computer-based and Internet-based interventions (CBIs), as a way to improve access to evidence-based psychotherapies, has attracted a lot of attention.25 TBIs provide treatment to patients who otherwise may not have access to help and improve healthcare for those seeking treatment by providing immediate access to evidence-based interventions.26
A growing body of literature supports using technology to implement evidence-based treatments (CBT and ERP) for OCD through self-help intervention with minimal therapist contact. Self-help interventions are useful to increase access for those in remote and rural areas and for patients who cannot afford treatment costs.25, 27-29
There is a growing body of evidence supporting the efficacy of TBIs in OCD treatment.30-36 Still, there are limitations, such as a lack of portability or access across the wide variety of contexts in which OCD symptoms occur (e.g., in the car, at work, while shopping) and limited access to techniques that may influence adherence to ERP, such as practice reminders. A generalized use of mobile phones, ease of use, and the multitude of functions performed by mobile phones and their mobility have made mobile technology the most powerful tool in providing health interventions.37 Mobile health applications may overcome the limitations of TBIs while improving access to evidence-based psychotherapy.
Despite recent efforts by researchers to use mobile applications for the dissemination and implementation of evidence-based psychotherapy,38-40 research on mobile applications for patients with obsessive-compulsive disorder is still in its infancy.
Given that the success of the treatment of these patients is more related to the patient's efforts to change behavior, mobile applications that can help them on an ongoing basis are useful. Therefore, in this regard, this study aimed to design and evaluate the usability of a prototype of a self-help application based on the “exposure and response prevention” technique for people with OCD contamination.
2 METHODS
The research framework was planned based on a prototyping model, which is one software development life cycle model (SDLC model) to meet the project goals. This methodology is based on the use of prototyping as a mechanism, aiming to create high-quality apps through a collaborative atmosphere where users participate actively in prototyping.41
- ▪
Needs assessment
- ▪
Building a paper prototype
- ▪
Building a digital prototype
- ▪
Usability evaluation
2.1 Needs assessment
Initially, a review article on previous related research in this area was conducted. Also, free Android apps and web-based remote health programs focusing on the education and treatment of obsessive-compulsive disorder using the CBT technique were reviewed for self-help (to identify problems in the app that should be avoided and useful features that can be included in the design). To determine the user's needs, a user survey was conducted with 15 patients with OCD contamination who were referred to clinics and psychological centers at Shiraz University of Medical Sciences and selected the convenience sampling method. For this purpose, patients were interviewed semistructured based on a series of fixed questions to determine their specific needs or requirements in relation to the app and their ideas and expectations. In addition, an expert survey was conducted using a researcher-made checklist with five psychiatrists who were members of the psychiatry department of Shiraz University of Medical Sciences (psychiatrist or doctorate in clinical psychology) specializing in behavioral-cognitive therapies to identify and determine app features and capabilities.
- 1.
Member of the Faculty of Psychiatry, Shiraz University of Medical Sciences (neuropsychologist or doctorate in clinical psychology) with at least 5 years of teaching experience in the field of health.
- 2.
Having work experience in the field of obsessive-compulsive disorder
- 3.
Having expertise in behavioral-cognitive therapies
- 1.
People with a primary diagnosis of obsessive-compulsive disorder (obsessive-compulsive disorder) based on DSM-5 and with the approval of a psychiatric specialist
- 2.
Patients between the ages of 18 and 60 years
- 1.
Unwillingness to participate in the study
The checklist was prepared based on the results of the literature review and existing system evaluations. The total requirements extracted were discussed in a joint meeting with the expert panel (including two psychiatrists specializing in CBT, one medical education specialist, and one medical informatics specialist [with at least 5 years of experience in health education]) and examined following the behavioral-cognitive therapy guidelines for obsessive-compulsive disorder and the remote treatment guidelines. Finally, a list of requirements was prepared, including functional capabilities, information, and educational elements that should be included in the application.
2.2 Paper prototype design
The final application's overall and simple design was created in the second phase, considering the requirements identified in the first phase using the wireframe sketcher tool. This wireframe includes user interface components, menus, and links. In addition to the components' location, how they work and interact was also determined.
At this phase, the educational content of the app was determined based on a self-help treatment approach and protocols of cognitive-behavioral therapy for obsessive-compulsive disorder, with an emphasis on the principles of “exposure and response prevention.”
This wireframe, along with the educational content related to all parts in the form of a paper prototype, was provided to an expert panel (including two psychiatrists specializing in CBT, one medical education specialist, one medical informatics specialist (with at least 5 years of experience in health education), and one specialist in the user interface [UI] and user experience [UX] design) for evaluation to review and approve the training content, identify problems and improvement points, and note their views and comments to be modified during the digital prototype design phase.
2.3 Digital prototype design
In the third phase, the problems identified in the paper prototype were fixed, the necessary refinements were made, and a digital prototype was developed using the Axure RP 9 software for Android OS.
2.3.1 Testing
Finally, in this phase, two types of usability evaluations were conducted: (1) a heuristic evaluation of the app prototype using informaticists with experience in interface design and/or human-computer interaction; (2) end-user usability testing:
2.3.2 Heuristic evaluation
Five medical informatics specialists that had at least a Master's degree in Medical Informatics trained in human-computer interaction and had a published article in medical informatics. Each expert independently examined the prototype user interface in terms of heuristic principles and entered the problems found in the data collection form, a standard form based on the heuristic method proposed by Nielsen.42 Three medical informatics specialists have confirmed the validity of the content of this form. This form consists of a table containing columns for problem description, place of problem, violation of the heuristic principle, severity rating of the problem, comments, and suggestions.
Furthermore, for each problem identified, a degree of severity should be assigned according to Nielsen's severity rating scale, ranging from 0 (no problem at all) to 4 (catastrophe problem). Finally, the sum of the problems related to each heuristic principle was classified into one of five categories based on the average severity of the problem: 0–0.5 no problem, 0.6–1.5 minor problem, 1.6–2.5 small problem, 2.6–3.5 big problem, and 3.6–4 serious problems.43
2.4 Usability testing with end-user
Ten patients (with the initial diagnosis of mild to moderate contamination OCD based on DSM-5 and approved by a psychiatrist, individuals who had not undergone cognitive-behavioral therapy or “exposure and reaction prevention” therapy) who did not participate in the design process were asked to rate the prototype's usability using the System Usability Scale (SUS) questionnaire. Ten participants were selected because past research had shown that the minimum percentage of problems identified rose from 55% to 82% and the mean percentage of problems rose from 85% to 95% when the number of users was increased from 5 to 10.44 The validity and reliability of this questionnaire were evaluated by Diyanat et al.45
2.5 Ethical considerations
Permissions and letters of recommendation were received from the Director of the Research Deputy of the School of Management and Medical Information Sciences, Shiraz University of Medical Sciences (SUMS) (IR.SUMS.REC.1398.449). Confirmations were also received from the security office of the university.
2.6 Data analysis
The process of data analysis was done using SPSS 21 software and descriptive statistics. Descriptive statistics used included frequency, frequency percentage, standard deviation.
3 RESULTS
Further on, the results of this study are presented following the same sequence of methodological phases as described previously.
3.1 Requirement analysis
Following the requirements analysis performed by the expert panel, the approved requirements were classified into two areas according to Table 1:
| Information and educational element | Disorder |
|
| App features and how to use it |
|
|
| Functional capabilities | Creating a personalized treatment plan
|
|
| Providing support strategies
|
||
| Setting reminders
|
||
| Tracking treatment progress
|
||
| Online Self-Help group | ||
3.2 Description of the prototype
This app prototype was designed for remote education and treatment for people with OCD contamination. Therefore, educational and psychological information and intended capabilities based on the ERP technique were provided as follows:
At the beginning of the app, an introduction to the app and its capabilities is provided. After creating an account and logging in to the app, on the home page, there is a capability called an online self-help group in which people with contamination OCD can exchange their experiences and ideas with other people with similar experiences, gather information, help each other, solve their problem easier, and, in addition to their loved ones, have solidarity with others (Figure 1).

In the treatment tab (Figure 2), after an initial assessment of the patient using the Yale-Brown Obsessive-Compulsive Scale for identifying OCD severity and the provision of psychological training about contamination OCD and its causes and symptoms, cognitive behavioral therapies for this disorder and their effectiveness, the introduction of the components and principles of ERP and how it works on OCD, how to set an exposure hierarchy, and how to utilize the exposure practice tool, the person can select the personalized treatment program. Since symptoms (obsessions, compulsions, and triggers) in people with OCD vary from person to person, a personalized treatment and management plan is needed. As a self-help tool, the guides in each step of setting a treatment plan will help users create the most effective exposures for their OCD symptoms. After entering their exposures, rating their anxiety, and creating their personal exposure hierarchy, instructing them where to begin and when to move on to more anxiety-provoking exposures. For each exposure practice, assessing anxiety, setting reminders, setting timers, and scheduling exposure practices can be done.

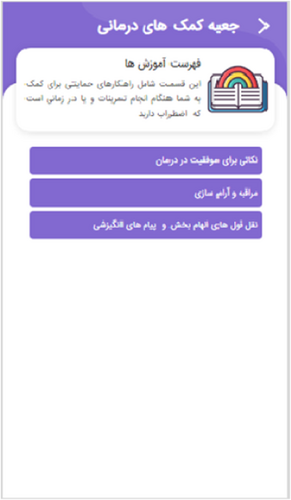
In the treatment aid toolbox tab, supportive strategies are provided to help a person when practicing exposure or experiencing anxiety. These strategies are tips for success in therapy, motivational messages, meditation, relaxation, and inspirational quotes (Figure 3).
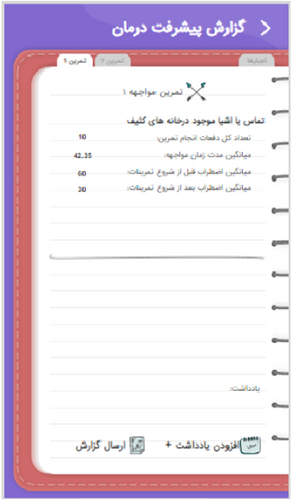
In the treatment progress tracking tab, progress tracking is done. The progress track will reset every week. For weekly practices, information is provided about the total number of times each practice is performed, the average duration of exposure, the average anxiety rate before and after the practices, changes in the method or duration, and the frequency of compulsions. The person can also record and note their experiences during the practice and email weekly progress reports to their therapist (Figures 4 and 5). In addition, periodic assessments of OCD severity can be done by setting reminders throughout the treatment period based on the app's recommended schedule.

3.3 Results of prototype evaluation
3.3.1 Usability testing with end-user
The characteristics of the 10 patients with OCD who evaluated the prototype as potential app users were as follows. Eight of them were women, and two were men. Their mean age was 34-year-old. 70% of patients with experience using mobile apps related to health or treatment had a university education, and 30% of patients without experience had a diploma or lower.
To analyze the results of usability evaluation, the mean score given by each evaluator to the questions in the SUS questionnaire using IBM SPSS Statistics 22.0 was calculated. The mean score was 76.75. Therefore, the usability of the app prototype was shown to be “good” from the end-user's perspective.46 The lowest score given by the evaluators is 65, and the highest score is 92.5.
The details of the patient's responses to the SUS statements in this usability evaluation are provided in Table 2. Based on the following results, features such as “frequent use of the system,” “ease of use,” “having good capabilities,” “fast learning of using the system,” and “confidence in using the system” had high scores. However, “the complexity,” “the need for an expert to use,” “the inconsistency in this app prototype,” “the difficulty of using the system,” and “the need to learn a lot before starting work” had a lower score, which indicates the usability of the prototype app is good.
| System Usability Scale | Mean | SD |
|---|---|---|
| I think that I would like to use this system frequently | 3.2 | 0.36 |
| I found the system unnecessarily complex | 0.9 | 0.29 |
| I thought the system was easy to use | 3.2 | 0.16 |
| I think that I would need the support of a technical person to be able to use this system | 0.9 | 0.69 |
| I found the various functions in this system were well integrated | 2.9 | 0.09 |
| I thought there was too much inconsistency in this system | 0.8 | 0.36 |
| I would imagine that most people would learn to use this system very quickly | 2.9 | 0.89 |
| I found the system very cumbersome to use | 0.9 | 0.69 |
| I felt very confident using the system | 2.8 | 0.16 |
| I needed to learn a lot of things before I could get going with this system | 1.1 | 0.49 |
| SUS score | 76.75 |
- Abbreviation: SD, standard deviation.
3.3.2 Heuristic evaluation
In prototype evaluation using components presented by Nielsen (heuristic evaluation), a total of 148 usability problems, respectively, were identified. Five evaluators identified 13, 23, 25, 31, and 40 problems, respectively. Duplicate, similar, unintentional problems and problems caused by prototype restrictions were removed, and disagreements about the violated heuristic principle for each problem were resolved. Finally, 39 problems were identified, some of which have been identified by several evaluators. Table 3 presents the frequency of identified usability problems based on their severity and the violated heuristics.
| Average severity | Severity | ||||||
|---|---|---|---|---|---|---|---|
| Violated heuristic | Rating | Cosmetic | Minor | Major | Catastrophe | Total | Severity of problem |
| 1. Visibility of system status | 1 | 1 | 0 | 0 | 0 | 1 | Minor |
| 2. Match between the system and the real world | 2.6 | 0 | 7 | 8 | 0 | 15 | Big |
| 3. User control and freedom | 2.6 | 0 | 4 | 5 | 0 | 9 | Big |
| 4. Help and documentation | 2.6 | 0 | 3 | 5 | 0 | 8 | Big |
| 5. Consistency and standards | 2.6 | 3 | 5 | 8 | 0 | 14 | Big |
| 6. Help users recognize, diagnose, and recover errors | 2.5 | 0 | 1 | 1 | 0 | 2 | Small |
| 7. Error prevention | 0 | 0 | 0 | 0 | 0 | 2 | No problem |
| 8. Recognition rather than recall | 2 | 1 | 2 | 1 | 0 | 4 | Small |
| 9. Flexibility and efficiency of use | 2 | 0 | 1 | 0 | 0 | 1 | Small |
| 10. Aesthetic and minimalist design | 3.1 | 8 | 4 | 1 | 3 | 16 | Big |
In prototype evaluation using components presented by Nielsen (heuristic evaluation), a total of 148 usability problems were identified. Five evaluators identified 13, 23, 25, 31, and 40 problems, respectively. Duplicate, similar, unintentional problems and problems caused by prototype restrictions were removed, and disagreements about the violated heuristic principle for each problem were resolved. Finally, 39 problems were identified, some of which have been identified by several evaluators. Table 3 presents the frequency of identified usability problems based on their severity and the violated heuristics. Out of the problems extracted, 2.6% (n = 1) were identified by five of our evaluators; 2.6% (n = 1) were identified by four evaluators; 10.25% (n = 4) by three evaluators; 20.5% (n = 8) by two evaluators; and 64.10% (n = 25) problems were identified by one evaluator.
The results of the evaluation showed that of all the identified problems, most are related to components: aesthetic and minimalist design (22.9%), and the least are related to components: visibility and system status (1.4%), flexibility and efficiency of use (1.4%), and error prevention (0%).
The average severity rating of the identified problems ranged from 1 (small problem), related to the visibility of system status, to 3.1 (big problem), related to aesthetic and minimalist design. Among the main problems identified which can be solved in the final application, we can mention problems related to the “aesthetic and minimalist design” principle. The content of the psychological tutorials and the treatment toolbox is monotonous, high, and boring, and the images, sounds, and multimedia can be used to make the training more attractive and effective. Also, the tutorials can be more concise and case-by-case, and the more important ones can be highlighted and presented in a variety of colors and fonts. Evaluators assigned a severity rating of four to this problem. Some of the most common problems related to each principle, along with evaluators' comments and suggestions for solving them, are listed in Table 4.
| Violated heuristic | Problem (severity rating) | Sample comment |
|---|---|---|
| 1. Visibility of system status | Mentioning the capabilities of the app in the slides introducing the program without mentioning that these are the capabilities app1 | Provide a brief explanation at the beginning of the slide that indicates that these capabilities are in the application |
| 2. Match between the system and the real world | Using inappropriate icons for the app guide character, patient assessment, self-help group guidelines, start of exposure practice, details of exposure practice, and review of exercises2 There are no “undo” and “redo” functions on some pages of the app3 | Use the appropriate icon or show a tooltip. Insert undo and redo buttons. |
| 3. User control and freedom | ||
| 4. Help and documentation | Lacking instructions for using the application for the user and how to set up a treatment plan4 | Show a short tutorial video at the beginning of installing the app about how to use the app. Embed a description link in a part of the application so the user can refer to it whenever she wants and read the description and help. |
| 5. Consistency and standards | Improper use of « and » in the button related to exit, end, and Yale-Brown test operations3 | Delete icon “«” and icon “»” or use the icons appropriate to the operation |
| 6. Help users recognize, diagnose, and recover errors | Lacking information on the page that sets a hierarchy of exposure about why exposures should be chosen from the least disturbing to the most worrisome3 | Provide adequate explanations for why it should start from the least disturbing |
| 7. Error prevention | No problem was identified | |
| 8. Recognition rather than recall | If the user has difficulty setting up a treatment plan and the details of ERP practicing, he or she should seek help from his or her memory and may not remember where he or she got the info3 | Embed a description link in a part of the application so the user can refer to it whenever she wants and read the description and help |
| 9. Flexibility and efficiency of use | Information on how to perform the compulsions on the page of rituals must be entered manually, which may be difficult for many users in terms of concept and writing and cause them not to complete this part2 | Provide examples of performing the compulsions in the tooltip format when the mouse is over this option. Record how to perform compulsions by voice. |
| 10. Aesthetic and minimalist design | The texts are intertwined and very uniform3 | Use colors, tables, shapes, drop-down lists, or other design features to make the text attractive. Major. |
4 DISCUSSION
Many current health interventions for healthcare-related topics are designed based on existing structures in the healthcare system. They may not be as effective as those that involve end users in the design process.47 Recently, user-centered design approaches have been used to build mobile health applications, focusing on chronic illness, lifestyle and mental health interventions, and remote patient monitoring. Studies have shown that using a user-centered approach in designing and evaluating a mobile phone application allows for a more useful design while increasing usability and user satisfaction. Working with potential users of the final app allows them to identify the features and information that users need and implement them in the application in a way that is easier and more understandable to the user.48 In this study, user-centered design principles have been used in the design and development of prototype applications (through participatory design with the cooperation of end users in the needs assessment, design, and evaluation).
In the needs assessment phase, the results of interviews with patients showed that due to problems such as difficulty in accessing a qualified therapist, saving time and money related to face-to-face visits, social stigma, and sometimes due to the negative effects of drugs, they prefer more active participation and acceptance of more responsibility in their treatment process, both remotely and through psychotherapy. Wooton, in his study, showed that different types of remote treatments (including low-intensity and high-intensity therapy, self-guided, and therapist-guided therapies) for obsessive-compulsive disorder are effective in reducing symptoms, and the results of their study were not significantly different from face-to-face treatment.49 Based on the findings of a study by Hogg, it has been shown that self-help, especially when provided through computer software or the Internet, is effective in treating anxiety disorders and improving treatment outcomes through self-care. The results are similar to those in general psychological anxiety disorder therapies. Therefore, self-help should be a standard treatment for patients seeking help from public health services.50 Pearce also found in a review of self-help treatment interventions for obsessive-compulsive disorder that self-help programs, while improving access to treatment, significantly reduced the severity of symptoms and treatment dropout rates. However, the results showed that self-help interventions with minimal therapist contact and predominantly self-help interventions improved clinical outcomes more than self-guided self-help interventions.28 This study attempts to use the feature of widespread use and portability of mobile devices to improve access to treatment materials in all situations and when OCD symptoms may occur to create a self-help program for mobile devices that, while improving access to treatment for people who have difficulties accessing treatment, enables patients to participate more actively in their treatment process.
Application prototype: with four main stages including assessment, psychological training, personalized treatment planning, tracking treatment progress, and capabilities such as an in-app self-help group, setting reminders for exercises, periodic assessment of the severity of disorder by performing a Yale-Brown test, a treatment aid toolbox (including supportive strategies to motivate the patient and help them during exercise or when experiencing general anxiety), and tracking the progress of treatment by providing a weekly progress report. The main stages of the application are designed following the necessary components for implementing cognitive-behavioral therapy with the technique of exposure and prevention of response to obsessive-compulsive disorder mentioned in the study of Redi.51 Some of these capabilities have been used in therapeutic interventions designed in studies by Boisseau et al.38 and Lenhard et al.52 and Greshkovic et al.53 that have determined the effectiveness of these interventions in improving the symptoms of obsessive-compulsive disorder in the studied samples. In the context of mobile health interventions, combining design features such as practical and easy-to-use content, program personalization, reminder setting, self-monitoring, and feedback to help individuals chart their progress may enhance the ability to increase user experience and participation and, in turn, reduce the likelihood of dropouts from self-guided therapies.54
Finally, to evaluate the usability of the application prototype, a heuristic evaluation has been performed with experts based on Nielsen principles to identify usability problems and a usability evaluation with the end user. One of the strengths of heuristic evaluation was the expertise and activity of the evaluators. Studies have shown that having expertise in both the evaluation and the system under study helps to identify problems better and increase the validity of evaluation results.55, 56 All assessors had medical informatics expertise, experience in healthcare, experience in human-computer interaction, and heuristic assessment skills, as well as experience in designing mobile health interventions. Patients gave positive feedback about the application in response to open-ended questions about their view of the application and the extent to which it conforms to their needs, goals, and skills. They also found it useful. However, some patients stated that this application did not have all the required information, capabilities, and functions that they expected. Of course, their expectations were beyond the scope of the study.
This study was one of the first feasibility studies of OCD applications in Iran. Due to the participation of specialists and your patient in the design and development of this study, its reproducibility increases. It is also suggested to study other areas of OCD.
In future research, we intend to develop the prototype and create the final Android mobile app, add features such as online communication with the therapist, cover all types of obsessive-compulsive disorder, evaluate the effectiveness and satisfaction of patients with the disorder from the final application, and compare the results with traditional face-to-face therapy in clinical trial studies.
4.1 Limitations
In the requirements identification phase, due to the lack of internal electronic treatment programs and access to all available external electronic treatment programs for obsessive-compulsive disorder (such as IOS-based applications and applications that are not free), there were limited patterns for design.
On the other hand, the treatment steps in this application are designed based on exposure and response prevention techniques. Exposure and response prevention techniques are recommended as the first line of treatment for patients who are not too depressed, anxious, or ill or who prefer psychotherapy to medication. Therefore, this application does not include remote treatment for people with severe symptoms of obsessive-compulsive disorder and depression.
5 CONCLUSION
The results of this study led to the design of a prototype of a self-help application for patients with obsessive-compulsive disorder based on exposure therapy and response prevention by a multidisciplinary team. The requirements identification and analysis phase identified components and guidelines for designing a therapeutic application using the exposure and response prevention technique. We hope that by using the components and following the instructions in the application design, patients use this application for self-treatment using exposure and response prevention; a reduction in symptoms and severity of the disorder can also occur effectively. The application of the four main stages of assessing the severity of OCD symptoms, psychoeducation, setting a personalized treatment plan based on exposure and response prevention techniques, and tracking the progress of treatment can help in the self-treatment of people with OCD contamination.
By creating an application prototype and evaluating whether it meets the basic needs of patients or not, both a better and more practical understanding of patients' potential problems when working with the final application was provided. Ideas and feedback from evaluations performed by patients and heuristic evaluation specialists were obtained that can be used to develop the final application. The usability evaluation results with the application's potential users showed that they reported the application as usable. In addition, heuristic evaluation with experts led to the identification of problems and suggestions for solving them. In the final version, in addition to solving the problems identified by the evaluators in how to provide information and implement the capabilities of the application in a way that is more practical, appropriate, and convenient for the user, the problems caused by the limitations of the prototyping tool in the correct and complete implementation of the capabilities will be eliminated and the user interface will be improved. Therefore, it seems that this application, as an effective intervention, can be useful in helping patients with OCD contamination with self-medication with exposure and prevention methods. In future research, while developing a digital prototype and creating the final Android mobile app, evaluation of usability, effectiveness, satisfaction of patients with obsessive-compulsive disorder from the final application, and comparison of results with traditional face-to-face treatment should be done in a clinical trial. We also intend to cover other types of obsessive-compulsive disorder and implement features such as online communication with the therapist for remote consultation, virtual meetings, and recording personal and therapeutic information in the patient profile to present to the therapist. The findings of this study and future research could contribute to emerging studies on the use of mobile applications in performing evidence-based psychotherapy.
AUTHOR CONTRIBUTIONS
Rita Rezaee: Conceptualization; data curation; methodology; project administration; software; supervision; writing—original draft; writing—review & editing. Ziba Parsa: Conceptualization; methodology; project administration; software; writing—original draft; writing—review & editing. Laaya Ahmadzadeh: Conceptualization; formal analysis; methodology; project administration; resources; visualization; writing—original draft; writing—review & editing. Leila Ahmadian: Conceptualization; methodology; project administration; supervision; visualization; writing—original draft; writing—review & editing. Sepehr Avazzadeh: Conceptualization; methodology; project administration; software; supervision; writing—original draft; writing—review & editing. Milad Ahmadi Marzaleh: Conceptualization; data curation; methodology; project administration; software; validation; writing—original draft; writing—review & editing.
ACKNOWLEDGMENTS
This project has partly been supported by a grant from the Shiraz University of Medical Sciences. The financial resources of Shiraz University of Medical Sciences had an impact on the collection, analysis and design of the application. Receiving financial resources has not had any adverse effect on the results.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Milad Ahmadi Marzaleh affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available.




