Hospitalizations among children with sickle cell disease enrolled in the Kumasi Sickle Cell Pan African Consortium (SPARCo) database: A cross sectional study
The new aspect of this study: The study highlights the importance of timely and appropriate intervention in preventing mortality in Acute chest syndrome.
The central finding of the study: Vaso-occlusion pain episodes, Acute chest syndrome, and infections are the leading causes of hospitalization in SCD patients.
The specific clinical relevance of this work: Successful treatment of ACS in resource-limited areas requires a high index of suspicion as well as the appropriate institution of individualized fluid therapy, oxygen therapy, and red cell transfusion in aliquots.
Abstract
Background and Aims
Sickle cell disease (SCD) is the commonest monogenic haemolytic disorder in Africa. Despite strides made in its management, a significant proportion of patients are hospitalized from the various complications of the disease. This study set out to describe the main causes and outcomes of hospitalizations among pediatric patients with SCD.
Methods
A cross-sectional study was conducted at the Pediatric Emergency Unit of Komfo Anokye Teaching Hospital within a period of 12 months to recruit pediatric SCD patients. This study looked at causes of admission, length of hospital stay (LOS), and outcome of admission.
Results
Of the 201 SCD patients recruited, 57.2% were males and majority were of SCD-SS phenotype 83.1%. The median age was 6 years. The three leading causes of hospitalization were Vaso-occlusive pain events (VOPE) (39.8%), acute chest syndrome (ACS) (25.9%), and infections (12.4%). Ten (5.0%) of the patients presented with a stroke. High admissions were observed in June (12.4%) and November (16.9%). The median (interquartile range [IQR]) LOS was 6 days (IQR: 4–10). Six (3.0%) of the patients died from complications of the disease during hospitalization.
Conclusion
VOPE, ACS, infections, and acute anaemia from hyperhaemolysis were observed as the most common causes of admissions among SCD patients. A good outcome of discharge was seen in most of the patients that were hospitalized with a median length of stay of 6 days. This study also strengthens the importance of a good SCD database with patient follow-ups for better outcomes in SCD patients.
Key points
- •
What is known: Vaso-occlusive pain episode, ACS, infections, and anaemia are the most common causes of admissions among pediatric SCD patients
- •
What's new: The study highlights the importance of timely and appropriate intervention in preventing mortality in acute chest syndrome (ACS). it also highlights the need for advanced therapy in some selected patients in SCD and the need to the review cost of these therapies.
- •
Clinical implication: Treatment of ACS in resource-limited areas requires a high index of suspicion as well as the appropriate institution of individualized therapy which includes fluid therapy, oxygen therapy, and red cell transfusion in aliquots to ensure a favorable outcome.
Abbreviations
-
- ACS
-
- acute chest syndrome
-
- CHRPE
-
- Committee on Human Research Publication and Ethics
-
- HbSS
-
- haemoglobin SS
-
- KATH
-
- Komfo Anokye Teaching Hospital
-
- LOS
-
- length of hospitalization
-
- PCV
-
- pneumococcal conjugate vaccine
-
- PEU
-
- pediatric emergency unit
-
- REDCap
-
- Research Electronic Data Capture
-
- SADaCC
-
- Sickle Africa Data Coordinating Center
-
- SATS
-
- South African Triage Scale
-
- SCD
-
- sickle cell disease
-
- SMS-KNUST
-
- School of Medical Sciences-Kwame Nkrumah University of Science and Technology
-
- SPARCo
-
- Sickle Pan African Research Consortium
-
- VOPE
-
- vaso-oclussive pain episodes
WHAT DOES THIS STUDY ADD?
The study throws light on the growing dominance of ACS as a cause of admission in SCD and how timely and appropriate intervention can lead to favorable outcomes. It also shows the growing occurrence of stroke in the SCD population and the need for affordable advanced therapies for better outcomes.
WHAT IS ALREADY KNOWN ON THIS TOPIC?
Severe complications such as VOPE, ACS, anaemia, and infections often lead to hospitalization among children with SCD.
1 INTRODUCTION
Sickle cell disease (SCD) is a common genetic disorder of clinical and public health significance and has an estimated worldwide prevalence of 5.2%.1 SCD is either inherited in the homozygous state also known as sickle cell anaemia (HbSS) or in a heterozygous form where an individual co-inherits HbS with another abnormal β globin gene, the commonest being SCD-SC, SCD-Sβ0 thalassemia, and SCD-Sβ+ thalassemia.2 With 25% of the population of Ghana having the Hb S trait and 2% of all babies having the disease,3 SCD has still not received the public health prominence it requires. Children born with SCD in developed countries have an increased chance of survival as compared to children born with SCD in low- and middle-income countries.4, 5 Poor healthcare delivery system and limited management of the disease are key factors.6
Severe complications such as infections, intermittent painful episodes, acute chest syndrome (ACS), stroke, pulmonary hypertension, musculoskeletal problems, and chronic pain often requires hospitalization and affects the quality of life of both the affected child and caregiver/parents.7
Ghana has seen a steady decline of under-five mortalities from 185/1000 live birth in 1969 to 47.9/1000 in 2018. This is mainly from gains made in tackling communicable diseases.8
Comprehensive pediatric sickle cell care has been offered at Komfo Anokye Teaching Hospital (KATH) since 1993 with services offered including newborn screening for SCD,3 provisions of chemoprophylaxis, vaccines, and disease-modifying drugs like hydroxyurea. These therapeutic interventions have been shown to significantly reduce SCD morbidity and mortality.9-11
Complications are common among children with SCD. Mild cases may be treated at home and may not require the expertise of health care personnel but severe to life-threatening complications usually require hospitalization. Comprehensive health care, which includes education on the complications of the disease promotes good healthcare-seeking behavior among parents and patients. In the absence of comprehensive healthcare, there is frequent and prolonged hospitalization from complications of SCD with resultant increased mortality, poor health outcome of patients, increased burden on health facilities (bed occupancy), and the negative socioeconomic impact on the caregivers/parents.12-14 A study by Brown et al.15 in Nigeria reported a median duration of admission of 8 days with Musculoskeletal complications emerging as the leading cause of increased risk for prolonged hospitalization.
Previous studies in Ghana on SCD focused on management, psychosocial and economic impact with little on the profile of patients with SCD.3, 16, 17 Furthermore, in our search, we found no studies conducted in Kumasi on the epidemiological characteristics of SCD hospitalizations. This article, therefore, describes the epidemiological characteristics, main causes, and outcomes of hospitalization among a cohort of pediatric patients with SCD.
2 METHODOLOGY
2.1 Study design
A cross-sectional study of patients admitted at the Pediatric Emergency Unit (PEU) and the pediatric haematology ward at KATH was done.
2.2 Study site
KATH is located in the Kumasi metropolis, the regional capital of the Ashanti Region in Ghana. The Ashanti Region has a population of 5,432,485 with an annual growth rate of 5.4%.18 KATH is a tertiary hospital with a bed capacity of 1200.19 The Child Health Directorate of KATH runs specialist outpatient clinics 5 days a week and a 24-h inpatient service. The clinic attends to about 5584 patients annually (KATH Performance Review, 2019: Unpublished Report).
PEU runs a 24-h service for all pediatric emergency admissions. Patients are triaged using The Modified South African Triage Scale (SATS), a physiology and symptom-based scale, which is used to determine the urgency with which patients are to be seen based on which of the four colors they are assigned. Patients are managed based on the draft Sickle Cell Management guidelines for Ghana. This guideline was based on the National Institute of Health SCD management guidelines. Patients with SCD emergencies are stabilized at the PEU and later transferred to the haematology wards. SCD care in KATH starts right after new-born screening and those enrolled at the clinic are started from 2 months of age on twice-daily penicillin prophylaxis. They are offered the infant series of pneumococcal conjugate vaccine (PCV), folic acid, and parental or caretaker education about SCD management in young children. Infants are scheduled to be reviewed every 2 and 3 months after infancy as specified in the standard operating procedure of the Center. Also, health maintenance evaluations include blood tests- complete blood counts with reticulocyte count, metabolic panel to assess kidney and liver functions, Transcranial Doppler ultrasonography (TCD) and eye screening are done for patients.
2.3 Study population
The study involved children from 2 months to 17 years, diagnosed with SCD and registered in the Kumasi-Sickle Pan Africa Research Consortium (SPARCo) database. SPARCo is a consortium of the Muhimbili University of Health and Allied Science (Tanzania), University of Abuja (Nigeria), Kwame Nkrumah University of Science and Technology (Ghana), and the Data Coordinating Center (DCC), now Sickle Africa Data Coordinating Center (SADaCC) to develop a database to capture and evaluate the outcomes of SCD patients. The Kumasi-SPARCo has enrolled over 3000 SCD patients within a period of 3 years (2018–2021).
2.4 Sample size estimation
We designed the study to last for 12 months thereby capturing all possible seasonal variations in the causes of admissions. To estimate the mortality and minimal prevalence of admission of 7%, using a confidence level of 95%, a precision of 3.5% from the estimated prevalence, and a nonresponse rate of 5%, a minimum of 200 patients were required for the study. Using the 2017 total admission of 232 SCD patients as a guide, we decided to recruit all patients who came into admission during the period of study.
2.5 Study procedure
All patients enrolled in the SPARCo database were eligible for the study, however, only hospitalized patients with SCD at KATH, within the period from April 2019 to March 2020 were recruited within the period of 12 months (April 2019 to March 2020). Upon enrollment, and stabilization of the patients to the pediatric haematology ward, the patients were followed up until discharge. The variables for this study included socio-demographic data of parent/guardian and child, hospitalization diagnosis, length of hospital stay (LOS), and outcome of hospitalization. Residential status was categorized as rural or urban; where an urban area was defined as towns or communities with 5000 and above residents.20
2.6 Ethical consideration
Ethical approval for the conduct of this study was obtained from the Committee on Human Research Publication and Ethics (CHRPE), a joint ethics committee of the Komfo Anokye Teaching Hospital and the School of Medical Sciences-Kwame Nkrumah University of Science and Technology (SMS-KNUST). Both assent and consent were obtained from patients (≥8 years) and parents/caregivers, respectively. Also, for patients less than 8 years consent was obtained from caregivers/parents.
2.7 Data management, validation, and analysis
Data were entered directly into a database designed with Research Electronic Data Capture (REDCap).21, 22 It was reviewed for completeness, inconsistencies, and discrepancies. The data was exported to Stata (STATA/SE version 14.0) for analysis. Data were presented using tables. Continuous variables were summarized by median and inter-quartile range whilst categorical variables were summarized in the form of frequencies and percentages. The confidence level of 95% was used.
3 RESULTS
3.1 Background characteristics of patients
From April 2019 to March 2020, 3074 admissions were recorded at the PEU, KATH, and 201/3074 (6.5%, 95% confidence interval [CI]: 5.7–7.5) had SCD. Approximately 43% of the SCD patients 86/201 (42.8%, 95% CI: 35.9–49.9) were females. The median age was 6 years (interquartile range [IQR]: 3–10 years). Biological parents formed the majority 189/201 (94.0%) of the primary caregivers of the patients with 154/201 (76.6%) of them being employed. More than half 117/201 (55.7%) were referred from other healthcare facilities. A total of 162 (80.6%) [162/201] of the patients reside in urban communities. The SCD phenotypes of the patients were SCD-SS 167/201 (83.1%), SCD-SC 33/201 (16.4%), and SCD-Sβ+-thalassemia 1/201(0.5%). Using the modified SATS,23 83/201 (41.3%) of the patients were triaged yellow and 13/201 (6.5%) were triaged red (Table 1).
| Variable | Frequency (n = 201) | Percentage (%) |
|---|---|---|
| Gender | ||
| male | 115 | 57.2 |
| Age (years) | ||
| <5 | 92 | 45.8 |
| 5–10 | 69 | 34.3 |
| 11–17 | 40 | 19.9 |
| Primary caregiver | ||
| Biological parent | 189 | 94.0 |
| Other relatives | 12 | 6.0 |
| Patient referred | 112 | 55.7 |
| Caregiver employed | 154 | 76.6 |
| Residency | ||
| Urban | 162 | 80.6 |
| SCD phenotype | ||
| SCD-SC | 33 | 16.4 |
| SCD-SS | 167 | 83.1 |
| SCD-Sβ+-thalassaemia | 1 | 0.5 |
| Triage color code | ||
| Red (emergency) | 13 | 6.5 |
| Orange (very urgent) | 47 | 23.4 |
| Yellow (urgent) | 83 | 41.3 |
| Green (nonurgent) | 58 | 28.9 |
| The outcome of admission | ||
| Died | 6 | 3.0 |
| Length of hospital stay (LOS) | ||
| ≤3 days | 46 | 22.9 |
| 4–7 days | 74 | 36.9 |
| >7 days | 81 | 40.3 |
| Median (IQR) | 6 (4–10) |
- Abbreviations: IQR, interquartile range; SCD, sickle cell disease.
3.2 The trend in admission of SCD patients
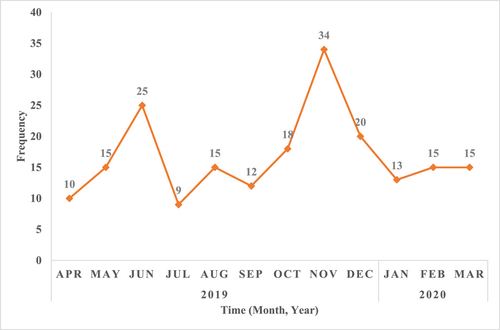
The median number of admissions per month to PEU among SCD patients was 15 over the 12-month study period. November 2019 had the highest number of admissions (34/201, 16.9%) and July 2019 (9/201, 4.5%) reported the lowest (Figure 1).
3.3 Reasons for admission of SCD patients
Vaso-occlusive pain episode (VOPE), ACS, and infections were the top three causes of admission of the patients (Table 2).
| Diagnosisa | Frequency (n = 201) | Percentage (%) |
|---|---|---|
|
80 | 39.8 |
|
52 | 25.9 |
|
25 | 12.4 |
| Streptococcus pneumoniae meningitis | 1 | 0.5 |
| Osteomyelitis | 1 | 0.5 |
| Lower Resp. Tract Infections | 1 | 0.5 |
| Septic arthritis | 2 | 1.0 |
| Urinary Tract Infection | 3 | 1.5 |
| Otitis media | 4 | 2.0 |
| Septicaemia | 13 | 6.5 |
|
19 | 9.5 |
|
14 | 7.0 |
|
14 | 7.0 |
|
11 | 5.5 |
|
10 | 5.0 |
|
6 | 3.0 |
|
3 | 1.5 |
|
3 | 1.5 |
- Note: The italic values show the breakdown of the specific infection, the absolute frequency and percentage.
- Abbreviations: ACS, acute chest syndrome; SCD, sickle cell disease; VOPE, Vaso-occlusive pain events.
- a More than one diagnosis present in some patients.
- b Clinical and laboratory diagnosis of infection.
3.4 Clinical diagnosis of infection
Out of the 25 children diagnosed with suspected bacterial infections (of which 13 were cases of septicaemia), there was no bacterial growth on blood culture in 21. The organisms isolated in the 4 positive cultures were 2 Coagulase-Negative Staphylococcus (CoNS), 1 Klebsiella species, and 1 Streptococcus pneumoniae (Table 2).
3.5 Patients diagnosed with VOPE, ACS, and stroke
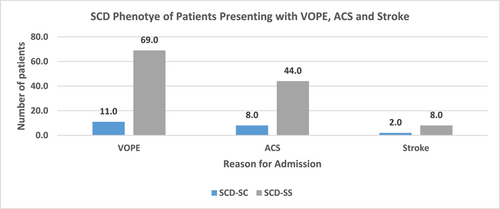
Among the patients that were admitted, SCD-SS phenotypes were the most predominant patients admitted as a result of VOPE (n = 69/80, 86.25%), ACS (n = 44/52, 84.62%), and stroke (n = 8/10, 80.0%) (Figure 2).
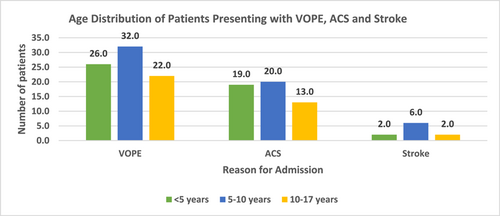
Also, the majority of patients between the ages of 5–10 years were admitted as a result of VOPE (n = 32/80, 40.0%), ACS (n = 20/52, 38.4%), and stroke (n = 6/10, 60.0%) (Figure 3).
3.6 Outcome of admissions
Six patients [6/201] (3.0%, 95% CI: 1.1–6.4) died. The causes of death were: Acute kidney failure, sepsis with multiorgan dysfunction, hyperhaemolysis with severe anaemia, acute chest syndrome, complications of stroke, and Streptococcus pneumoniae meningitis. Five out of the six deaths had SCD-SS phenotype and one person had SCD-SC phenotype. The SCD-SC patient died from hyperhaemolysis with severe anaemia. Five of the patients who died were males. The median LOS was 6 (IQR: 6–10), with 81/201 (40.3%) discharged after more than 7 days (Table 1).
4 DISCUSSION
The study findings show that SCD still places a high burden on our scarce medical resources despite efforts being made to reduce SCD-related morbidity and mortality. In the current study, SCD admissions made up 6.5% of the total admissions at pediatric unit and 6.95% of SCD patients enrolled in the SPARCo registry, respectively.
SCD-SS was more prevalent as compared to SCD-SC in the study, with a percentage of 83.1% versus 16.4%. This correlates with data from the newborn screening program in Kumasi and the SPARCo database which had SCD-SS as the predominant phenotype. SCD-SS patients also have a more severe form of the disease and are likely to be admitted.24
The male preponderance in admissions aligns with study findings reported by Ikefuna et al.25 and Abhulimhen-Iyoha et al.26 in Nigeria. In the adult population, this gender disparity has been demonstrated and has been attributed to hormonal variation postpuberty. Again, some studies attributed the worse clinical course in males to their impaired response to chronic vascular injury which would otherwise increase the production of nitric oxide.27
In this study, the peak of admissions was noted in June and November which coincides with the rainy season (April-November) in Kumasi (where the study was conducted).28 This may seem to support the growing literature on the association between acute pain episodes and exposure to cold weather conditions. Cold exposure results in peripheral Vaso-constrictions with the attendant reduction in blood flow velocity and subsequent HbS polymerization. This could be the reason for the increase in admissions around this period.29-31 This association was first observed in a case report, where the cold climate was reported to have a significant association with infection and acute pain in SCD patients.32 Following this report about 10 decades ago, many studies with stronger evidence have proven this association.29, 30, 33 It is therefore safe to attribute the observed increase in the cases in June and November to the cold weather as cold weather is known to cause vasoconstriction which leads to vaso-occlusion causing acute events in sickle cell patients.
VOPE was the leading cause of admissions of SCD patients in this study which is similar to reports by Salman et al.34 in Iraq and Brown et al.15 in Nigeria. There are variations in the causes of admissions among SCD patients worldwide with VOPEs being predominant in the developed worlds and infections leading in LMIC.30, 35 Ikefuna et al.25 reported infections as the leading cause of admissions in Nigeria whilst Adekile, reported vaso-occlusive pain events as the cause in Kuwait.36 Although this study was conducted in a low-income country, the infection prevention measures (pneumococcal vaccination as well as penicillin prophylaxis) that have been incorporated into the comprehensive care offered to our patients with SCD in no small ways, may have contributed to infection being in third place as a cause of admissions. As part of the expanded program on immunization in Ghana, all children are given the Hemophilus influenza type b vaccine and 13-valent PCV using a 3-dose primary series at ages 6, 10, and 14 weeks with no booster, and this started from 2002 to 2012, respectively.24
We opine that these infection prevention measures may have led to infection being in third place instead of the first as a cause of hospital admission. This finding conforms with the 84.0% reduction in the incidence of infection after initiation of oral penicillin prophylaxis as reported in a study in Jamaica.37 Again, the positive effect of pneumococcal vaccination on infections in SCD patients is supported by Halasa et al.,38 which demonstrated a decline in the rate of invasive pneumococcal disease by 90.8% and 93.4% in children aged less than 2 and 5 years, respectively.26 The 21 out of 25 negative cultures could be attributed to the fact that most of the patients had been referred from other facilities where they had already been given antibiotics.
ACS, an important cause of morbidity and mortality in children with SCD was the second leading cause of admission and agrees with findings from a study by Abd Elmoneim et al.38 in Saudi Arabia.39
To ensure favorable outcomes for our patients with ACS, patients are treated individually concerning fluid management, and blood transfusion is given in aliquots to prevent fluid overload as per our protocol. In most studies on SCD admissions conducted in Africa, the trio have maintained the first three positions as causes of hospitalizations.34, 40
In this study, the common cause of acute anaemia was hyper-haemolysis which is similar to studies in Nigeria by Juwah et al.,41 and Adegoke et al.14
Stroke accounted for admissions in 10 out of 201 patients (5%), which is comparable to what was documented by Adeogoke et al., in southwestern Nigeria where the prevalence of stroke was 3.0% of admissions. This value is, however, lower than the 11.0% recorded prevalence of pediatric stroke in England and France before systematic screening and intervention.13 Again, 8 in 10 of the patients with stroke had SCD-SS phenotype and were aged less than or equal to 10 years, in line with what was documented by Ohene-Frempong et al.42 that the highest risk of first ischaemic stroke is during the first decade.
The last decade has seen unprecedented advances in the treatment of SCD with the introduction of Hematopoietic Stem Cell Transplant (HSCT), gene therapy and other several clinical trials on targeted therapies in SCD. The 5% of the participants with stroke are all potential candidates for advanced therapy in SCD.43
The main challenge envisaged with the use of advanced therapy in our patients is cost as the average Ghanaian with a minimum daily wage of 1.2 US dollars44 will have to work for over 4000 years to acquire the 2.8 million dollars which is the estimated cost of gene therapy.45
About 3.0% of admitted patients died in our study, largely occurring in males and SCD-SS. This mortality rate is comparable to the 1.9% reported by Brown et al.15 and 2.7% recorded by Abhulimhen et al.26 in Nigeria. Ikefuna and Emodi,25 however, documented a case fatality of 8.5% which is higher than what was recorded in this study.46 The lower death rate compared to Ikefuna et al.25 in Nigeria, could be attributed to better and comprehensive care given to our patients including early detection (new-born screening), infection prevention measures such as vaccination and penicillin prophylaxis, pediatric intensive care services, and improvement in environmental conditions. The causes of death observed in this present study confirm the common causes of death reported among SCD patients and hence management and strict monitoring of admitted SCD patients must be of priority. Mortality in males was higher than that in their female counterparts which could be because males have a worse course of the disease compared to females.31
The median length of stay was observed to be higher (6 days) in comparison with a study by Bou-Maroun et al.,47 and Gerais et al.48 Prolonged hospitalization has been observed to have a poorer outcome with associated higher exposure to iatrogenic harm as well as the effect on the healthcare system not excluding the negative socioeconomic impact on the patient and the community.14, 46
The need for the fever to settle for at least 48 h before discharging pediatric patients in the directorate (as an in-patient management protocol) could be one of the reasons for the longer hospital stay. Further studies may be required to throw more light on this issue.
A study by Nienke Seiger et al.49 in 2013 reported that children with chronic illness (16%) like SCD were more likely to be under-triaged as compared to the 11% of children presenting to the emergency unit without chronic illness. With a majority of our patients being triaged yellow and green (70.2%) and our study reporting a comparatively higher average length of stay, under-triaging is one concept that should be critically looked at as a triage system if employed appropriately, should not only improve patient flow and reduce waiting time but also reduce the overall length of stay and mortality.
5 STUDY LIMITATION
The study included only admissions at KATH and hence did not take admissions at other health facilities into consideration.
6 CONCLUSION
VOPE, ACS, infection, and anaemia are the most common causes of admissions among pediatric SCD patients in KATH. A higher proportion of death occurred among patients with phenotype SCD-SS and the median length of stay was 6 days. The study showed that SCD is a significant cause of admissions. Further studies on the trends of admissions over a longer duration are required to evaluate the impact of comprehensive care on hospitalization events in pediatric patients with SCD.
AUTHOR CONTRIBUTIONS
Yaa Gyamfua Oppong–Mensah: Conceptualization; Data curation; Supervision; Writing—original draft; Writing—review & editing. Samuel Frimpong Odoom: Data curation; Formal analysis. Isaac Nyanor: Data curation; Formal analysis. Evans Xorse Amuzu: Formal analysis. Suraj Abubakar Yawnumah: Data curation. Emmanuel Asafo-Adjei: Conceptualization; Writing—review & editing. Samuel Blay Nguah: Supervision; Writing—review & editing. Daniel Ansong: Conceptualization; Writing—review & editing. Alex Osei-Akoto: Conceptualization; Writing—review & editing. Vivian Paintsil: Conceptualization; Supervision; Writing—review & editing.
ACKNOWLEDGMENTS
SPARCo 1 Hub for and SADACC for the provision of resources that enhanced our data collection Abdul Razak Mohammed, Elliot Eli Dogbe, and Dr Paul Obeng for supporting data collection and verification. The study was funded by the National Heart, Lung and Blood Institute (NHLBI), Grant Number 1U24HL135881 through the Muhimbili University of Health and Allied Sciences (MUHAS) Sickle Cell Program. The funders had no involvement in conceptualization of the study, the study design; data collection, analysis, and interpretation of data; writing of the report; and the decision to submit the report for publication.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
TRANSPARENCY STATEMENT
The lead author Yaa Gyamfua Oppong–Mensah affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
Data available on request due to privacy/ethical restrictions. Data supporting the findings of this study are available from the corresponding author.




