Non-spinal low back pain: Global epidemiology, trends, and risk factors
Pourya Shokri, Mahdi Zahmatyar, and Mahdi Falah Tafti contributed equally to this study.
Abstract
Background and Aims
Low back pain (LBP) is one of the most debilitating and prevalent disorders. The prevalence of LBP ranges from 30% to 80%, depending on the population, and increases with age. Causes of LBP are typically classified as spinal and non-spinal. The main goal of this study was to investigate the non-spinal causes of LBP, since neglecting these factors leads to increases in the financial, psychological, and physical burden of LBP on individuals as well as on society.
Methods
The data were extracted after searching the PubMed database and Google Scholar search engine up to October 27, 2021. We included all studies that were conducted on a human population and assessed the effects of epidemiological, biological, psychological, and sociodemographic factors on the incidence or progression of LBP.
Results
The most common causes of non-spinal LBP were diseases such as nephrolithiasis, endometriosis, tumors, fibromyalgia, and conditions like psychological disorders and pregnancy. Nevertheless, the perceived intensity of the pain can be affected by factors such as socioeconomic level, genetics, age, habits, diet, and psychological status.
Conclusion
The epidemiology, etiologies, and risk factors associated with LBP should be more clearly recognized to better prevent, diagnose, and treat the underlying disease and to reduce the burden of LBP.
Key points
-
Low back pain (LBP) is a highly prevalent and incapacitating condition, affecting a significant portion of the population.
-
LBP can arise from various sources, categorized as spinal and non-spinal causes.
-
There are several non-spinal causes of back pain, including conditions like nephrolithiasis, endometriosis, tumors, fibromyalgia, psychological disorders, and pregnancy.
1 INTRODUCTION
Low back pain (LBP) is one of the most frequent types of discomfort and is a common condition in adults. Although back pain is sometimes thought of as a small burden,1 this disorder is one of the most common causes of long-term disability in most countries (65%) in the world.2 It has been estimated that the lifetime prevalence of LBP is between 30% and 80%.3 Previous research has also shown that approximately 6.3%–15.4% of the population experience LBP for the first time each year, and that the chance of a second occurrence within a year ranges from 1.5% to 36%.4 Previous research estimated that in 2019 about 223.5 million people suffered from LBP and that there were 63.7 million years lived with disability.5 Also, in 2019, the highest prevalent cases of LBP were found in the 50–54 age group.6
The etiologies of LBP can be classified into two main types, which are spinal and non-spinal back pain. Spinal back pain originates from the spine, and includes skeletal irregularities, spina bifida, traumatic events, as well as degenerative problems such as intervertebral disc degeneration, and spondylosis. In addition, this category also includes inflammatory diseases like arthritis, as well as nerve and spinal cord problems like spinal nerve compression, sciatica or radiculopathy, spinal stenosis, spondylolisthesis, disc herniations, infectious etiologies, and osteoporosis. Although spinal back pain is common and negatively affects life quality, focusing only on the spinal etiologies of back pain will result in missing a substantial portion of the burden imposed by this disorder.
The non-spinal causes of LBP include kidney stones, which can cause sharp pains in the lower back, usually on one side, especially if it co-occurs with infections of the upper urinary tract.7 Endometriosis often presents itself as low back and abdominal pain, which can periodically occur or worsen during intercourse, and has co-incidence with dysmenorrhea.8 Fibromyalgia is a chronic disease with an idiopathic etiology, and affects approximately 2%–4% of the population. Its common presentations are pain, stiffness, and tenderness in the muscles, tendons, and joints, as well as fatigue, anxiety, and depression.9 Fibromyalgia is diagnosed by centralized bilateral pain in specific body sites, including the gluteal region, but it is perceived as mechanical spinal pain with normal paraclinical findings. Tumors can have an effect on the bony spine or spinal cord, leading to back pain. The most common and leading symptom in patients with spine tumors is back pain.10 Furthermore, tumors with an origin other than the spine can also cause back pain. Metastatic spinal cord compression is the term used to describe this type of lesion. Spinal metastases occur in about 3%–5% of malignant disease patients, leading to collapse at one of several vertebral levels and the development of metastatic spinal cord compression and consequent pain.11 Pregnancy can also be included as a common presentation of back pain. It has been reported that about 50% of pregnant women suffer from some kind of LBP during their pregnancies and even after birth. This kind of back pain can be considered as a complex pain with a combination of mechanical, hormonal, and other factors.12 Dealing with the non-spinal etiologies of LBP can be more challenging and may require more attention in the diagnosis and treatment than spinal etiologies.
Due to the importance of the non-spinal causes of back pain, and the consequent socioeconomic impacts on the individual and society in general, the present study provides a narrative review and a brief history of non-spinal LBP, including its global epidemiology, economic burden, etiologies (i.e., the factors that cause the disease), and risk factors (i.e., the factors that predispose individuals to the disease).
2 METHODS
We searched for publications about lower back pain in Google Scholar and PubMed up to October 27, 2021 using the following keywords: (“low back pain” OR “low backache” OR “back pain” OR “lumbago”) AND (“history” OR “epidemiology” OR “global burden of disease” OR “risk factor” OR “biologic factor” OR “psychological factor” OR “age” OR “genetic” OR “stress” OR “neuromusculoskeletal disorder” OR “Sociodemographic Characteristics” OR “social support” OR “Dietary Patterns”). No search filters were used.
Studies were included if they were conducted on a human population and designed to investigate the effects of biological factors (e.g., age, gender, genetic patterns, and diet), psychological factors (e.g., habits and mental health), and sociodemographic characteristics on the incidence or progression of LBP. Supporting Information: Figure S1 represents the flowchart of study selection.
3 RESULTS
3.1 History
The majority of people suffer from lower back pain at least once in their lifetime, although this problem is usually self-limiting and recovery is achieved within 4–6 weeks.13-16 However, 5%–10% of cases continue for more than 12 weeks and become chronic back pain, leading to a higher disease burden.17, 18 Furthermore, back pain is one of the most common causes of disability in society, with high care and treatment costs, and in 2018 back pain was the leading cause of disability worldwide.13-15, 18 Anatomically, back pain refers to pain in the L1–L5 vertebrae and the sacroiliac area, which continues from the bottom edge of the 12th rib to the iliac crest area.1, 13, 14
The documented history of back pain goes back to 1500 BCE, in an Egyptian case report.19 Furthermore, degenerative changes have been found in Egyptian mummies, which confirm the existence of this problem in ancient times.19 In the 16th–18th centuries, the concepts of rheumatism, rheumatic fever, and arthritis were gradually being recognized and considered to be the cause of back pain.19 Before the industrial revolution and railway construction, transport accidents were not known as causes of back pain. However, from the middle of the 19th century, accident trauma was considered to be one of the leading causes of back pain.19 During the 19th century, with the advancement of pathology and medical science, other factors such as aortic aneurysm, malignancy, women's complaints, abdominal viscera, infectious and inflammatory factors, spinal problems, and trauma were recognized as causes of back pain.19, 20
At present, back pain can be divided into acute (4–6 weeks), sub-acute (6–12 weeks), and chronic (>12 weeks).14, 21 Furthermore, back pain can be axial, radicular (neuropathic), referred, or nociplastic.1, 14 Axial and radicular pains are usually caused by spinal and pathological problems in the spinal column (e.g., trauma, disc problems, problems with the surrounding soft tissues, spinal tumors, infectious, and degenerative problems).20, 22, 23 Radicular pain with nerve involvement causes the pain to spread along the dermatomes.20, 22 Before the 18th century, the treatment for back pain was symptomatic, while in the following centuries, the main treatment for back pain was rest.19 During the 19th century, with the increase in musculoskeletal problems, physical treatments such as physiotherapy, manipulation, electrical therapy, and hydrotherapy were commonly used.19 Interestingly, during the 20th century, patients were encouraged to move as soon as possible and advised not to rest in bed.19 Currently, the treatment of back pain depends upon the etiology and the severity of the pain.22 For the treatment of acute and subacute LBP, massage, acupuncture, heat, spinal manipulation, chiropractic manipulation, physical therapy, traction, and nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended. In contrast, for chronic LBP, NSAIDs, opiates, tramadol, and duloxetine are suggested.22, 24, 25 However, no benefits have been found from the use of acetaminophen, selective serotonin reuptake inhibitors, and tricyclic antidepressants.22, 24-26
3.2 Epidemiology
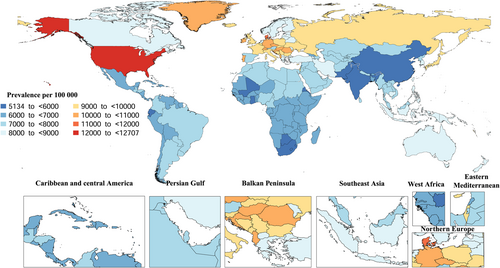
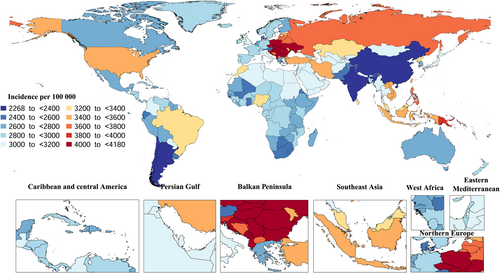
In 2019, the Central Europe and East Asia regions had the highest and lowest age-standardized incidence rates of LBP, with 4106.3 (3639.7–4642.9) and 2317.4 (2050.7–2613.8) per 100,000, respectively. The United States, Denmark, and Switzerland had the highest age-standardized point prevalence of LBP, while China, India, and Ghana had the lowest prevalence rates.6 Figure 1 represents the age-standardized point prevalence of LBP by country.
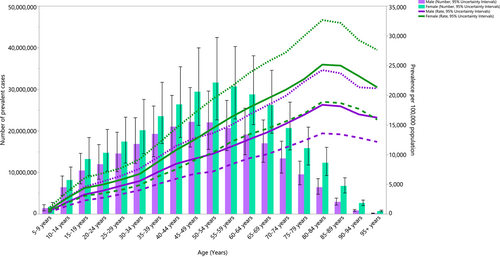
The largest increases in the age-standardized incidence rates of LBP, over the period 1990–2019, were found in Zambia, Mali, and Canada. In 2019, Poland, Vanuatu, and Romania had the highest age-standardized incidence rates of LBP, while India, China, and Singapore had the lowest age-standardized incidence rates (Figure 2).6 Globally, the burden of LBP was slightly higher in females than among males, but this difference was not statistically significant. In 2019, globally, the age-standardized prevalence of LBP increased with age up to the 80–84 year group, and then decreased with advancing age (Figure 3).6
3.3 Etiologies
The lumbosacral and paraspinal regions and their related pathologies cause substantial disability among patients.27 Chronic LBP, which is one of the most significant sociomedical and socioeconomic diseases, represents one of the most common pain syndromes.28-30
At some point in their life, approximately 80% of the population will experience back pain.31 Children also frequently experience LBP, but not as commonly as adults, with almost half of all pediatric patients experiencing back pain 27, 32-34
LBP can develop unexpectedly or progressively, with or without attribution to an originating event.35 Nonspecific LBP, which is defined as a pain of unknown origin extending from the gluteal fold to the upper lumbar vertebrae, is indicated in the vast majority of cases. These pains initiate from an assumed musculoligamentous process.36 Paraspinal muscle spasms and point tenderness are common causes,27 but a simple low back soft tissue injury is the most common cause of back pain in athletes. These soft tissues can be muscles, ligaments, or fascial tissues.27 Essentially, muscle strains and ligament sprains account for as much as 97% of back pain complications, with more severe etiologies comprising less than 5% of all back problems in the general adult population.37 However, LBP develops due to non-musculoskeletal disorders in about 5%–15% of patients.38
In addition to structural injuries and diseases of the spine, pain can also arise from diseases of the intra-abdominal organs, such as the liver, gallbladder, and pancreas. Referred pain can also be seen among the conditions that give rise to LBP, such as posterior abdominal organ diseases, including the uterus, ovaries, and urine bladder, which can all cause lower back pain. Moreover, the psychogenic pain associated with conversion disorder, depression, psychosomatic, and some personality traits can also cause lower back pain.39
Tumors, infections, and primary inflammatory conditions are rare manifestations in an athlete. However, they should still be considered when patients manifest unusual symptoms such as nonmechanical pain, night pain, or constitutional symptoms.27 LBP can also originate from gynecological, urological, gastrointestinal, or neurological problems, making obtaining a differential diagnosis complex.40, 41 Furthermore, nonmechanical etiologies may cause LBP with radiculopathy. For instance, metastatic tumors to the vertebrae, leptomeningeal metastases, or primary spinal tumors can all cause radiculopathy.42-44 In addition, some infections, such as herpes zoster, cytomegalovirus, and Borrelia burgdorferi (the organism causing Lyme disease), can destroy nerve roots.42-44 Moreover, diabetes mellitus, a common systemic illness, can result in lumbosacral radiculopathy or radiculoplexopathy. Diabetes mellitus most likely causes ischemic nerve injury via microscopic vasculitis.45
3.3.1 Renal disease
Back pain may also be a result of kidney disease, due to the common roots of the sensory nerves between the kidneys and the spine. For example, as a result of cyst enlargement, rupture, or infection, nephrolithiasis is commonly reported by patients with autosomal dominant polycystic kidney disease.46 Also, in later childhood, renal diseases are similar to infections (e.g., intervertebral disk infection and paraspinal abscesses), inflammation (systemic lupus erythematosus and rheumatoid arthritis), and leukemia which all cause LBP.47 Moreover, LBP, dysuria, urinary frequency, hematuria, and costovertebral angle tenderness can all be present among patients with acute nephrolithiasis and urinary tract infections, making a clinical diagnosis challenging.48
3.3.2 Endometriosis
Endometriosis is one of the most widespread and common conditions among fertile women, affecting 10%–15% of fertile women.49 Women of childbearing age are the most susceptible to endometriosis, with the highest incidence occurring between 25 and 29 years old.50 Endometriosis is a very complex and common gynecological disorder that should always be considered during the clinical assessment of women with lumbar and pelvic pain.49, 51 Women with symptomatic endometriosis typically experience pain in the hypogastric and perineal regions,52 although they can also experience pain in the lower back and lower limbs.53, 54 Endometriosis is associated with high morbidity and can be one of the differential diagnoses of nonspecific LBP.51
Endometriosis is one of the leading causes of chronic pelvic pain, hysterectomy, infertility, and gynecological hospitalization.50, 55, 56 In addition to the peripheral nociceptive effect of endometrial lesions, central nervous system sensitization is a notable characteristic in women with endometriosis, and is recognized as a critical factor in the pathogenesis of endometriosis-associated pain.57 Furthermore, chronic pelvic pain and endometriosis patients are frequently inclined to depression, anxiety, and fatigue.57
A large proportion of women with endometriosis have other comorbidities, such as fibromyalgia, chronic fatigue syndrome, hypothyroidism, asthma, and autoimmune disorders.58 The risk factors for endometriosis are low body mass index (BMI), a family history, and low levels of exercise, with the hallmark symptoms being generalized pelvic pain, dysmenorrhea, and dyspareunia.50, 55, 56
The initial plan of care for endometriosis is physical therapy, often required as part of an integrative approach to achieve resolution.51, 59 Endometriosis tends to be a chronic and recurrent disorder, and repeated laparoscopies are usually common for its management.51 Nevertheless, laparoscopy alone did not substantially improve long-term outcomes in women with pelvic pain syndromes, such as endometriosis.51 Finally, if endometriosis is misdiagnosed or left untreated, it can progress from a small lesion to a larger one with extensive fibrosis and adhesions.59 It is therefore crucial that thorough physical examinations are conducted and that therapists consider all musculoskeletal, visceral, and psychosocial components to accurately identify the pelvic disorder. This is due to its high morbidity and prevalence, the tendency to manifest itself as nonspecific LBP, and the similar age incidence of endometriosis and nonspecific LBP.51
3.3.3 Tumors
The symptoms and signs of intraspinal tumors depend on their location,31 and their diagnostic features include weakness of the lower extremities, paraspinal or hamstring muscle spasm, back stiffness, nuchal rigidity, painful scoliosis, pyramidal track signs, spine tenderness, relaxed sphincter tone, broad-based gait, or a palpable mass found upon rectal examination.60 In addition, most likely benign spine tumors in children include osteoid osteoma, osteoblastoma, and aneurysmal bone cysts, but tumors of the osseous vertebral column or the spinal canal are exceedingly rare.31 Disseminated metastasis to the lumbar spine is one of the pathological indicators of multiple myeloma. Malignant tumors, such as osteosarcoma, Ewing's sarcoma, lung, stomach, breast, and prostate cancers sometimes metastasize to the lumbar spine.27, 39 When tumors such as neuromas, angiomas, or other tumor types develop in the lumbar cord or lumbar spine, patients can experience intense LBP.27, 39
3.3.4 Pregnancy
Pregnancy-related LBP is one of the most common musculoskeletal complaints among pregnant women, and the majority of pregnant women report LBP and pelvic pain.61 About 50% of pregnant women (ranging from 25% to 90%) will suffer from LBP, one third of which claim this to be a significant problem that causes them severe pain. Most affected women are in their first pregnancy and most commonly between the fifth and seventh month of pregnancy.61-64 LBP is the most common cause of sick leave after delivery,65, 66 with 80% of sufferers claiming that it affects their daily routines and 10% reporting that they cannot work.67 In another study, 61.8% of pregnant women suffering from LBP claimed that the pain was moderate to severe, while 9% claimed that they were completely disabled by the pain.68 The pain can manifest itself either as pain in the pelvic girdle between the posterior iliac crest and the gluteal fold or lumbar pain over and around the lumbar spine above the sacrum. LBP during pregnancy is very similar to lumbar pain experienced by women who are not pregnant and may or may not radiate to the foot. In addition, tenderness in the paravertebral muscles is a common outcome.69 Increased BMI may be a risk factor for pregnancy-related LBP, although not all studies agree.6761
Furthermore, younger age, number of previous pregnancies, previous LBP and pelvic pain, and a history of diagnosed hypermobility and amenorrhea tend to increase the risk of developing LBP and pelvic pain and are more common in women with LBP.61, 64, 70-72 In addition, LBP during menstruation is an additional risk factor for pregnancy-related LBP.62 Furthermore, 85% of women who experienced LBP and pelvic pain during a previous pregnancy reported a reoccurrence in a subsequent pregnancy.67 Actually, LBP occurs twice as often in women with a history of back pain and women who have been previously pregnant.71 Although pregnancy-associated LBP generally resolves postpartum,81 LBP during pregnancy is considered the most critical risk factor for postpartum LBP.65 Physical activity or exercising before pregnancy is the most common approach to managing back pain and is correlated with a decreased risk of developing LBP.73 These practices are also related to the onset of back pain during pregnancy.61, 74
LBP in pregnancy is generally attributed to the many changes in load and body mechanics that occur while carrying a child, such as postural changes or abdominal muscle stretches.66 Moreover, the pain and associated symptoms may be constant or may only occur during specific postural changes or even after extended activity.63 The most frequently suggested mechanism is that the LBP is caused by mechanical factors due to the weight gain during pregnancy, increased abdominal sagittal diameter, the consequent shifting of the body's gravity center anteriorly, and increasing stress on the lower back. Furthermore, the enlarged uterus causes muscle fatigue and results in an extra load on the spine, as well as the response of the intervertebral discs to axial loading, leading to decreased height via compression of the spine, which results in LBP.65, 66, 75, 76
3.3.5 Psychological conditions
Previous research has found LBP to be related to several psychological disorders and their symptoms (e.g., fatigue and insomnia), and abnormal personality traits were significantly more common in patients with LBP.77-80 Furthermore, research has found that psychiatric disturbances were more prevalent among LBP patients.77 For example, neurosis was the most common psychological condition in the LBP group and there was a higher prevalence of neurotic depression among women, but not among men.77
3.3.6 Fibromyalgia
In more than half of fibromyalgia patients (52%), fibromyalgia was preceded by chronic cervicalgia or chronic LBP.81-83 Moreover, psychopathological changes are often observed in patients with fibromyalgia and chronic LBP.84-88
3.3.7 Infection
Spinal infection is a less common cause of LBP.66 It is more likely in patients with a history of recent or ongoing urinary or skin infections, an indwelling catheter, or regular injection use. These infections develop in different situations, for instance, during the development of tuberculous spondylitis or purulent spondylitis after the tubercle bacilli or pyogenic bacteria destroy vertebral bodies or intervertebral discs.39
3.4 Risk factors
3.4.1 Age
Aging is one of the most important risk factors of LBP. Most studies have found that the highest incidence of LBP is in the third decade of life, and the overall prevalence increases until the age of 60–65 years old.21, 89, 90 The prevalence of LBP in people over 50 years old is about three to four times higher than among people aged 18–30 years old.17, 24 Approximately one fifth of patients who visit a physician with back problems are over 65 years old.89 Among young patients, the most common ages for LBP complaints are between 13 and 14 years old,89 with the prevalence of LBP increasing from 1% to 6% in 7–10 year olds to 18% in 14–16 year olds.26 As under 18 years old and over 50 years old are the red zones for back pain, people with LBP in these age groups need more careful investigations to determine the causes.15, 24 In young patients with acute LBP, congenital disabilities, spondylosis, and bone fractures should also be considered.15 Furthermore, in people over 50 years old, LBP can be a sign of malignancy or intra-abdominal problems.15 Thus, in elderly patients, symptoms like night pain, weight loss, and saddle anesthesia are essential for evaluating malignancy.15, 24 In those older than 70, osteoporosis is a risk factor for vertebral fractures,15, 24 and the degenerative changes increase with age.21
3.4.2 Sociodemographic characteristics
Previous studies have shown that several sociodemographic characteristics affect the onset of pain, such as perceived financial strain or deprivation status of the local area.91 Recent studies have also found that discrimination affects both the onset and the severity of the pain.91, 92 Perhaps this may be due in part to differences in access to healthcare.93 Furthermore, the influence of social factors on pain is much larger in the older adult population.94 As such, it is not unrealistic to assume that these factors also play a role in the development of LBP. Socioeconomic factors are complex and multi-faceted, with those related to LBP including poor living conditions (e.g., an area with a high crime rate) and poor housing-induced stress.91, 93, 94 Economic status affects nutrition and dietary habits, as well as health and obesity, which all contribute to perceived pain.94 Inequality and social pressures also affect the individual's psychological health. The use of healthcare services also differs by country and cultures, which also affects the perceived pain.91, 93, 94 Importantly, financial status affects when and how often people use healthcare services, which means that people with poor financial status only visit a doctor when their pain is more severe, compared to more well-off patients.95 Furthermore, many work-related factors are related to LBP, including job satisfaction, fear of not being supported by co-workers, and psychological strain.96
3.4.3 Dietary patterns
Nutritional status is one of the most crucial aspects of health, implying that this also affects LBP. However, there is very little literature investigating diet as a risk factor. It is well known that diet affects various chronic pain disorders; thus, it is plausible to suggest that diet quality and dietary patterns could play a role in LBP.97-101 Studies have shown that some aspects of diet and nutrition could affect LBP. For example, a study by Ghandour et al. found that high caffeine intake affects back pain in female adolescents.98 In addition, research found that although food poverty (lack of access to a healthy diet) was similarly distributed among social classes, adolescents who reported going to bed hungry were more likely to have back pain.99 It has also been established that musculoskeletal health and growth depend on nutrition during adolescence.100 In a study by Zick et al., the nutritional status of an adult population with and without chronic back pain was compared. Even though the calorie intakes were similar for both groups, the diet quality, defined by the consumption of protein, fruits, whole grains, and dairy, was significantly worse in people with chronic back pain, even after adjusting for clinical and sociodemographic factors. This study also found that natural sugars were less present in the diets of those in the chronic back pain group,97 meaning that the type of sugar in one's diet could affect LBP. In another study, this effect was found to be more pronounced in women, meaning that women should pay even more attention to their diet to prevent LBP.101 In summary, as many studies support the role of diet quality in the development of LBP, it is important to take diet and dietary patterns more seriously.97-101
3.4.4 Habits
Much like caffeine, heavy alcohol use, and heavy smoking may play a substantial role in LBP. Alcohol has been shown to affect neck pain,102 so assuming excessive alcohol consumption as a risk factor for LBP appears logical. Alcohol has also been shown to affect pain circuits, which may also contribute to LBP.103 While alcohol does affect functioning and performance, the exact process remains unclear, particularly as alcohol use is associated with other risk factors like smoking and depression.104
The evidence linking smoking to LBP is inconsistent, mainly because some studies of patients with low back disorders report confusing symptoms.105 However, most studies also support the fact that smoking is a risk factor for LBP. In a prospective cohort study, the working population of Finland was observed for 28 years and a correlation was found between smoking and back pain.106 In another study on the Icelandic population, smokers were also shown to have more LBP.107 The effect of smoking on pain and LBP could be due to several reasons. Although the precise physiological mechanism remains unclear, smoking is known to cause chronic pain in long-term users.108 Although it is not the subject of this review, smoking has also been shown to affect spinal degeneration in animal models, which could cause LBP.109 Furthermore, smoking affects the blood flow and nutrition of the spine. In summary, while many studies support the role of smoking in back pain, most of these relate the cause to vertebrae and disc issues.108, 109
3.4.5 Mental health
With a newfound focus on mental health in general, many studies have started evaluating different aspects of mental health, physical health, and pain perception. However, only a small number of studies have investigated the relationship that mental health and depression have with LBP.110-112 In a study by Carrol et al., Canadian patients were followed up for 6–12 months to investigate the relationship that depression has with neck pain and LBP. This study found that socioeconomic factors, health, comorbidities, and previous injury were confounding variables and that depressive symptoms were a strong independent predictor. Patients in the highest quartile of the depression score had a four times higher chance of having LBP, compared to those in the lowest quartile.110 In a prospective longitudinal study by Currie et al., 9909 adults were followed for 24 months to evaluate major depression as a risk factor for chronic LBP. During the study, 3.6% of the depressed population reported a new onset of LBP, while this figure was 1.1% in the nondepressed population, demonstrating a statistically significant relationship between depression and LBP.111 In another epidemiological study of adults over 75 years old, depressive symptoms were shown to be an independent risk factor for the future onset of LBP.112 While most studies support depression as a risk factor, the exact mechanisms are not straightforward. Mental health affects many aspects of physical health, making it hard to pinpoint a specific reason for LBP. A negative view of oneself, poor diet, substance abuse, less attention to physical health, and postponing visits to a physician due to poor mental health, could all contribute to the increased risk of LBP.110-112
3.4.6 Genetics
LBP is a multifactorial disease. Age, weight, height, smoking, occupation, perceptual processes, and mental stress may all play a role in the development and efficacy of treatment for LBP.113-117 Moreover, genetic factors can make individuals more susceptible to environmental risk factors and exposures.118, 119 Previous research found a correlation between LBP and genetics in both the young and adults.120 Furthermore, one study suggests that the heritability of LBP ranges from 30% to 45%.121 Moreover, the genetic factors that affect LBP also play a role in degenerative changes, inflammation, and pain perception.122 Several lines of data show that genetics play a role in the efficacy of treatment by altering the mechanisms by which drugs affect the physiology and the distribution of the drugs throughout the patient's body.123
Several genes have been found to be involved in LBP and in the response to treatment. For example, genetic polymorphisms in genes encoding interleukin 1 (IL-1α), interleukin-1 receptor antagonist (IL-1RN), and interleukin-6 (IL-6) may affect the persistence of low radicular pain. Moreover, genetic variants in the gene-encoding proteins, such as matrix metalloprotease, collagens, and vitamin D receptors, may affect the degeneration of intervertebral discs.122 In addition, pain modulation can be affected by variants in the KCNJ6 gene (A1032G and G1250A), which encodes the components of the GIRK potassium channel, or in the catechol-O-methyl transferase enzyme gene, which breakdowns active catecholamines such as noradrenalin, adrenalin, and dopamine.124 Furthermore, the mu receptor is the first place of action for widely used opioids, so studying variations in this gene is extremely important when evaluating single-nucleotide polymorphism. For example, patients carrying the variant A118G-G allele had a reduced response to morphine and fentanyl treatment and required higher doses for pain relief.125-127
3.4.7 Other factors
Previous studies have shown that fear-avoidance beliefs (FABs) affect chronic LBP and physical disability, especially in older adults.128, 129 While avoidance behaviors are good in injured patients, when there is no physical damage, this behavior damages tissues and worsens the physical condition.129 There is very little literature on FAB as a risk factor for the onset of LBP, but studies have shown that FAB plays a considerable role in patients' prognosis, chronicity, and functionality.128-130 Therefore, clinicians should consider FAB when treating chronic LBP.131 Most studies support the fact that FAB, also known as kinesiophobia, and pain catastrophizing affect the patient's prognosis.132 Ledoux et al. found these factors made no difference to whether or not the functional capacity improved among older adults with LBP.133 In addition, Kovacs et al. found that FAB and pain catastrophizing had a minimal effect on self-reported LBP disability in older adults.134 In short, FAB possibly affects patients' recovery, chronicity, and functional capacity and should not be ignored during treatment.128-134
4 CONCLUSIONS
LBP is common and poses one of the highest burdens across the world. The etiologies are often spinal, but non-spinal etiologies are also common. Consequently, non-spinal etiologies should also be considered in the treatment plan. Renal disease and cyst enlargement, rupture, infection, and nephrolithiasis, along with some inheritable abnormalities, can be the underlying etiology of LBP and may be accompanied by dysuria, urinary frequency, hematuria, and costovertebral tenderness. Among reproductive-aged women, endometriosis should be considered for nonspecific LBP, and about half of pregnant women suffer severe LBP. In psychological disorders, as well as fibromyalgia, psychopathological changes occur in combination with chronic LBP.
Among the risk factors, sociodemographic characteristics such as deprivation and limited access to healthcare services are important. Nutrition also plays an important role in LBP and even with the same calorie intake, poor diet quality can be associated with chronic back pain. Caffeine, heavy alcohol consumption, and heavy smoking are all correlated with LBP. In addition to the environmental factors, genetic factors also influence the likelihood of LBP, including variations in the IL-1RN, IL-6, KCNJ6 gene, and several others. Age is a significant risk factor for LBP. An increase in LBP is observed during the third decade of life, as well as in the 60–65 age group. In those aged more than 70 years old, vertebral fractures and degenerative changes make the LBP problem worse. In the absence of an injury, fear-avoidance beliefs or kinesiophobia can cause tissue damage and can worsen physical condition. As a final conclusion, all of the above-mentioned non-spinal etiologies and risk factors of chronic back pain should be considered during the diagnosis and when making the treatment plan.
AUTHOR CONTRIBUTIONS
Pourya Shokri: Conceptualization; writing—original draft; writing—review and editing. Mahdi Zahmatyar: Writing—original draft; writing—review and editing. Mahdi Falah Tafti: Writing—original draft; writing—review and editing. Mobin Fathy: Writing—original draft; writing—review and editing. Mohammadmahdi Rezaei Tolzali: Writing—original draft; writing—review and editing. Amir Ghaffari Jolfayi: Writing—original draft; writing—review and editing. Seyed Aria Nejadghaderi: Conceptualization; project administration; writing—original draft; writing—review and editing. Mark J. M. Sullman: Writing—review and editing. Ali-Asghar Kolahi: Supervision; writing—review and editing. Saeid Safiri: Conceptualization; supervision; writing—review and editing.
ACKNOWLEDGMENTS
The present study is the part of the project that was supported by the Shahid Beheshti University of Medical Sciences, Tehran, Iran. (Grant no. 32565). The authors would also like to thank the Clinical Research Development Unit of Tabriz Valiasr Hospital, Tabriz University of Medical Sciences, Tabriz, Iran for their assistance in this research.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
TRANSPARENCY STATEMENT
The lead author Saeid Safiri and Ali-Asghar Kolahi affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




