723 | VANISHING BILE DUCT SYNDROME IN HODGKIN’S LYMPHOMA: A CASE SERIES FROM HOSPITALS IN THE COMMUNITY OF MADRID
A. Garcia Noblejas, A. López García, A. Lario Arribas, A. De Laiglesia Lorenzo, P. Fernández-Caldas González, and F. J. Peñalver Párraga equally contributing author.
Introduction: VBDS is a disorder that leads to severe liver failure due to the progressive destruction of intrahepatic bile ducts. It should be suspected in cases of cholestasis without other causes of hepatitis. Liver biopsy being the diagnostic gold standard. Few cases of VBDS have been reported as a paraneoplastic manifestation of Hodgkin lymphoma (HL), with immune mechanisms likely playing a role. The prognosis of HL with VBDS is poor, with a significant risk of progression to liver failure and death. Its treatment poses a challenge and the administration of ABVD at full doses is contraindicated due to its hepatotoxicity.
Methods: We present a multicenter, observational, and retrospective case series study performed in hospitals of the Community of Madrid (HCAM), Spain, involving patients diagnosed with HL who developed VBDS.
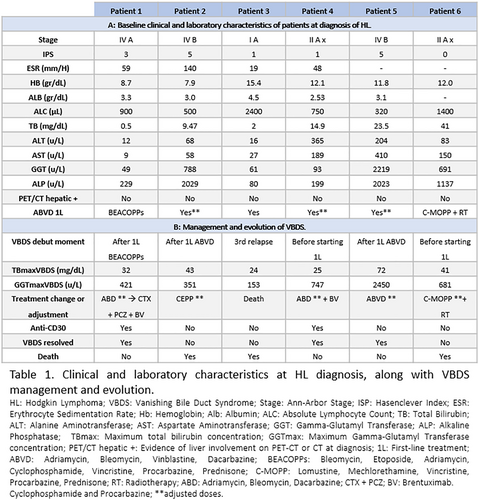
Results: Six cases of VBDS associated with EH were confirmed by liver biopsy at HCAM between 2000 and 2022 one of them postmortem. Two cases were excluded due to the lack of histological confirmation. Table 1 presents the clinical and laboratory characteristics at HL diagnosis, along with the management and evolution of VBDS. 50% were males, and the median age at diagnosis was 42 years (range 27–58). The histology was classical HL in all patients, and 50% presented with localized disease. At the time of HL diagnosis, imaging tests (PET-CT and CT) showed no evidence of liver involvement, and cases 1 and 3 had nearly normal liver profiles. ABVD treatment was administered in 66% of cases, with dose adjustments in 3 out of 4 patients based on liver function. ABVD treatment was the first-line therapy in 66% of cases, with dose adjustments in 3 out of 4 patients based on liver function. In 3 cases (50%), VBDS was diagnosed after the initiation of first-line treatment, with a median time of 37 days. In 2 cases, it preceded the diagnosis of HL, and in 1 case, it was diagnosed at the third relapse with a fatal outcome. The overall mortality rate in our series is 50%. The three surviving patients are in complete remission (CR), with one having more than 10 years of follow-up. Two out of three patients had localized-stage HL, which is considered a favorable prognostic factor according to the literature. Brentuximab (BV) was administered in combination with chemotherapy in two of these patients.
Conclusions: VBDS associated with HL is rare, but it carries a potentially poor prognosis, highlighting the importance of early suspicion and, when possible, histological diagnosis. The available literature on this topic is limited, which makes our case series potentially valuable in providing insights into the clinical presentation, management, and prognosis of this condition. Although we do not have sufficient data to establish an alternative therapeutic protocol to standard treatments, the results of our series suggest that the use of BV may be effective, showing favorable outcomes in terms of response and survival.
Keyword: Hodgkin lymphoma
No potential sources of conflict of interest.