337 | ALLOGENEIC HEMATOPOIETIC STEM CELL TRANSPLANTATION FOR PRIMARY CENTRAL NERVOUS SYSTEM LYMPHOMA: AN ANALYSIS FROM THE EBMT LYMPHOMA WORKING PARTY
Introduction: Despite a high proportion of patients with primary central nervous system lymphoma (PCNSL) achieving complete remission (CR) following first-line treatment, relapses still occur in about 50% of patients. The prognosis in the relapsed/refractory (R/R) setting remains poor, and therapeutic options, including salvage chemotherapies, radiotherapy, CAR-T-cell or experimental combinations of small molecules like BTKi and IMIDs are limited and partly not approved. Allogeneic hematopoietic stem cell transplantation (allo-HSCT) has shown curative potential in various lymphoma subtypes; however, data on its efficacy in PCNSL is limited to a small number of published cases worldwide.
Methods: We conducted a retrospective, registry-based analysis using data from the European Society for Blood and Marrow Transplantation (EBMT), including adult patients diagnosed with PCNSL who underwent allo-HSCT between 2016 and 2022.
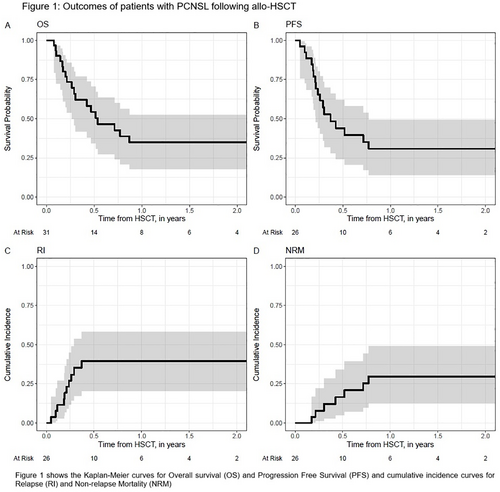
Results: A total of 31 patients were included, with a median age of 50 years (range: 22–68) at the time of allo-HSCT. The median follow-up period was 1.5 years (95% CI: 0.9–5.8). Males comprised 58% of the cohort, and 61% of patients had a Karnofsky performance status ≥ 90%. The median time from diagnosis to allo-HSCT was 22 months (range: 4–196). Most patients were heavily pretreated, with 54% having received ≥ 3 prior lines of therapy, 12% having received two, and 35% having received one. Prior to allo-HSCT, 57% of patients were in CR, 23% in partial remission (PR), and 20% had active R/R disease. The most frequently used conditioning regimen was a combination of Busulfan, Fludarabine, and Thiotepa (42%). Post-transplant cyclophosphamide was administered in 40% of patients. Total body irradiation (TBI) based conditioning was used in 23% of cases. Donors were predominantly related (48% matched, 26% haploidentical), while 26% were unrelated. The overall survival (OS) rates at 1 and 2 years were 34.9%. Progression-free survival (PFS) at 1 and 2 years was 30.8%. The relapse incidence (RI) was 39.6% in the first year and did not increase in the second year. Non-relapse mortality was 29.7% at 1 and 2 years. Chronic graft-versus-host disease was observed in 24.9% of patients at both 1 and 2 years. The GvHD-free, relapse-free survival (GRFS) rates were 19.9% at 1 and 2 years.
Conclusion: In this large registry-based cohort of patients with PCNSL undergoing allo-HSCT, our findings indicate that allo-HSCT is an effective treatment in a subset of patients. The stable RI beyond one year may suggest a potential for long-term disease control in approximately one third of transplanted patients.
Research funding declaration: This is an analysis supported by the EBMT Lymphoma Working Party
Keywords: cellular therapies; aggressive B-cell non-Hodgkin lymphoma; extranodal non-Hodgkin lymphoma
No potential sources of conflict of interest.