42 | CIRCULATING TUMOR DNA FOR MONITORING PRIMARY MEDIASTINAL B-CELL LYMPHOMA IN COMPLEMENT TO PET: A PROSPECTIVE MULTICENTER LYSA STUDY
Introduction: Positron Emission Tomography (PET), is routinely used for Primary Mediastinal B-cell Lymphoma (PMBL) therapy guidance, but has limited sensitivity (Se) and specificity (Sp) for minimal residual disease (MRD) assessment in this disease.
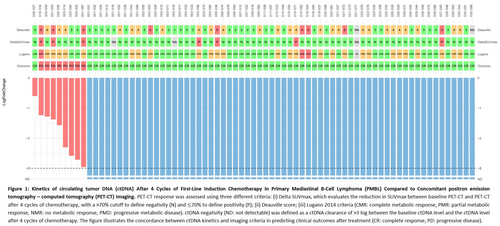
Methods: In the prospective CAMIL study (NCT04824950), we evaluated ctDNA and PET in newly diagnosed PMBL patients (pts) treated with immunochemotherapy (ICT) at 31 LYSA centers (2021–2023). PET4 response was centrally reviewed, with a ΔSUVmax threshold of > 70% to define negativity. Blood samples were collected before ICT and on PET4 day. ctDNA was analyzed using a CAPP-seq protocol (∼380 kb selector, 155 genes, > 2000× coverage, detection limit: 10−3).
Results: Of 84 pts with centrally confirmed PMBL, the median age was 32 years (Q1: 26; Q3: 40), with 64% female. Key features: elevated LDH (85%), PS 0–1 (91%), stage I-II (67%), IPI 0–2 (89%), renal/adrenal involvement (3.6%), bulky disease ≥ 10 cm (70%), mediastinal (100%) and extra-nodal involvement (50%). Median metabolic tumor volume (MTV, fixed SUV4 method) and total lesion glycolysis (TLG) were 453 cm3 (231; 664) and 4022 (2019; 7918). Induction regimens were R-CHOP14 (61%) and R-ACVBP (39%). For consolidation, three pts underwent autologous transplantation, four received radiotherapy, and the others continued ICT. Baseline ctDNA was detected in 82/84 (98%) pts, with a median level of 755 hGE/mL, 8.9% variant allele frequency, 7 variants per gene, and 101 variants per sample. Among 131 mutated genes, the most frequent were BCL6 (98%, mainly non-coding), SOCS1 (89%), IGLL5 (85%), B2M (73%), and CD83 (72%). PET4 was performed in 98% of pts and was negative in 90.2%, regardless of induction regimen. ctDNA4 negativity (> 3 log clearance) was achieved in 88% (64/73) with no regimen differences. ctDNA4 outperformed PET4 in predicting progressions (9 events), with higher Se (1 versus 0.44), Sp (0.99 versus 0.94), positive predictive value (0.89 versus 0.5), and negative predictive value (1 versus 0.93). After a median follow-up of 21.5 months, 1-year (yr) PFS and OS were 90.5% and 99% (1 non-lymphoma related death). 1-year PFS was 93.2% for PET4- versus 62.5% for PET4+ pts (p < 10−4) and 98.4% for ctDNA4− versus 33.3% for ctDNA4+ pts (p < 10−4). ctDNA4+ pts had higher median baseline TLG (8448 versus 3622, p = 0.033) and MTV (836 versus 417 cm3, p = 0.03). In univariate analysis, CRP (HR = 1.19 [1.07; 1.33]), LDH (HR = 1.21 [1.08;1.37]), MTV (HR = 1.26 [0.98;1.61]), PET4+ (12.4 [3.3; 46.9]) and ctDNA4+ (78.1 [9.5;641.7]) were associated with inferior PFS, whereas ctDNA4-/PET4- was associated with a better outcome (HR = 0.01 [0;0.08]). In a multivariate model for PFS including CRP, LDH, MTV, and ctDNA4-/PET4-, ctDNA4-/PET4- was associated with longer PFS (HR 0.07 [0.01; 0.69], p = 0.023).
Conclusion: ctDNA analysis by CAPP-seq in PMBL is informative for 98% of pts. Each somatic variant served as an MRD biomarker. PET4 response and ctDNA4 clearance were strong and complementary predictors of outcome.
Research funding declaration: This work was supported by grants from Centre Henri Becquerel (AO_2020), CALYM (ANR-2022), GEFLUC (AO_2021), Ligue Contre le Cancer (Seine-Maritime committee, AO_2021), Prix Bertrand Coiffier (LYSA/ELI), and ABBVIE.
Keywords: PET-CT; liquid biopsy; aggressive B-cell non-Hodgkin lymphoma
No potential sources of conflict of interest.