Differences in baseline PET/CT lymphoma distribution patterns between DLBCL-NOS and high-risk DLBCL patients
Introduction: Approximately 8%–10% of diffuse large B-cell lymphoma (DLBCL) patients have genetic aberrations, known as high grade B-cell lymphoma double-hit and triple-hit (HGBL-DH/TH, with MYC/BCL2 and MYC/BCL2/BCL6 rearrangements). However, it is unknown whether these subtypes have different distribution patterns on baseline PET/CT compared to cases without rearrangements (wild-type), or with only a single MYC (SH) arrangement, or MYC/BCL6 rearrangements (hereafter collectively referred to as DLBCL-NOS (Not Otherwise Specified)). The aim of this study was to analyze the frequencies in which different nodal stations and extranodal sites were involved, with secondary endpoints including: bulky disease (BD), the number of lesions, the number of nodal stations, the number of extranodal sites and metabolic tumor volume (MTV).
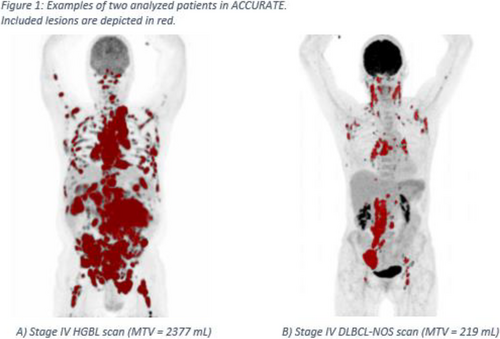
Methods: Baseline PET/CT scans from the HOVON-84 (2006-005174-42), HOVON-130 (2014-002654-39) and HOVON-152 (2017-003631-12) were reviewed. Lesions were included if the uptake was above SUV4.0 using the ACCURATE software tool, which was also used to calculate MTV.Differences in frequencies of involved nodal stations, extranodal sites and the occurrence of BD were determined with X2- and Fisher exact tests. The number of lesions, number of nodal stations, number of extranodal sites, and MTV were analyzed with unpaired T-tests and Mann-Whitney U tests.
Results: 88 DLBCL-NOS patients (66 wild-type, 16 SH and 6 MYC/BLC6) were compared to 38 HGBL cases (26 DH, 12 TH). The HGBL patients showed more frequent involvement of para-aortic (68.4% vs. 48.2%, p = 0.043) and mesenteric (71.1% vs. 37.5%, p < 0.001) nodal stations, and a higher occurrence of gastro-intestinal- (44.7% vs. 21.6%, p = 0.008), pancreatic- (23.7% vs. 8.0%, p = 0.021) and peritoneal (15.9% vs. 3.4%, p = 0.022) extranodal involvement compared to DLBCL-NOS cases. Renal- (18.4% vs. 6.8%, p = 0.061) and dermal (13.2% vs. 3.4%, p = 0.053) localizations were also more common in HGBL than in DLBCL-NOS. In contrast, splenic- and pulmonary hilar node involvement occurred more often in DLBCL-NOS; 27.2% versus 10.5% (p = 0.029) and 28.4% versus 10.5% (p = 0.05) respectively. Furthermore, the total number of extranodal sites involved was found to be higher in HGBL patients (median 2 vs. 1, p = 0.011), as was the MTV (median 777 vs. 305 mL, p = 0.021) and the rate at which BD occurred (57.9% vs. 23.9%, p < 0.001). No difference in the total number of lesions and the total number of involved nodal stations was observed between the two groups.
Keywords: Aggressive B-cell non-Hodgkin lymphoma, Diagnostic and Prognostic Biomarkers, PET-CT
No conflicts of interests pertinent to the abstract.