MUTATIONAL LANDSCAPE OF DIFFUSE LARGE B-CELL LYMPHOMA (DLBCL) AT DIAGNOSIS AND AT PROGRESSION ASSESSED BY CIRCULATING TUMOR DNA ANALYSIS
Introduction: Previous studies have highlighted the potential of circulating tumor DNA (ctDNA) to determine the mutational profile of DLBCL, and assess the molecular changes over time and the genetic mechanisms of resistance. In addition, the quantity of ctDNA could also predict the response and outcome of the patients. The aim of this study was to analyze the mutational profile at diagnosis and its dynamics after frontline treatment and in the refractory/relapse settings.
Methods: We included 65 patients (M/F 32/33, median age 64 years) diagnosed with DLBCL in a single institution between 2016 and 2018 according to the WHO criteria. All patients were treated with chemoimmunotherapy. After initial treatment, 47 patients achieved CR, 4 PR, 7 were refractory and in 7 cases the response was not evaluable. Samples were obtained both at diagnosis and at relapse/progression in refractory/relapsed patients. Tumor genomic DNA (gDNA) was isolated from formalin-fixed paraffin-embedded (FFPE) diagnostic tissue biopsies and at relapse when available. A panel of 115 genes was amplified using a hybridization capture based protocol from 10-30 ng of ctDNA and 150 ng of gDNA (SureSelectXT-Agilent Technologies) and sequenced in a MiSeq instrument (Illumina).
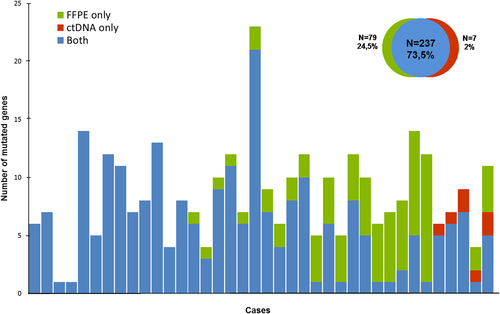
Results: ctDNA was obtained from all patients at diagnosis (median of 34 ng; range: 10-1507 ng) and from 12 refractory/relapsed cases. At least one mutation could be detected in 88% of the cases. Median number of mutations per sample was 6 (0-21 mutations). The genes most frequently mutated at diagnosis in plasma samples were KMT2D, TP53, MYD88, TNFRSF14, PIM1, CREBBP, BCL2 and EP300. In 38 cases, paired FFPE samples were available as detailed in the figure. Sensitivity of ctDNA to detect tumor mutations at baseline FFPE samples was 75% (95%IC: 69.5-80.5). Of note, most of the cases in which mutations were not detected in the ctDNA had a primary extranodal origin. In the 12 cases with a ctDNA sample at diagnosis and at progression, 5 cases showed the same mutational profile, whereas in 6 cases a change in the number of mutated genes was observed (3 cases had fewer mutations; 3 cases had new mutations) and in one case no mutations were detected at relapse. In addition, selection of minor subclonal mutations was observed in 2 cases. Patients with high pretreatment ctDNA levels (>3 log hGE/mL) had a worse PFS and OS than those with low levels (18-month PFS 24 vs 77%; 18-month OS 58 vs 94%; p<0.004).
Keywords: diffuse large B-cell lymphoma (DLBCL); molecular genetics.