Letter to the Editor: Living Donor Liver Transplantation or Deceased Donor Liver Transplantation in High Model for End-Stage Liver Disease Score—Which Is Better?
TO THE EDITOR:
We read with interest the study by Wong et al.(1) We congratulate the authors for the commendable work. We would like to share our concerns regarding the study.
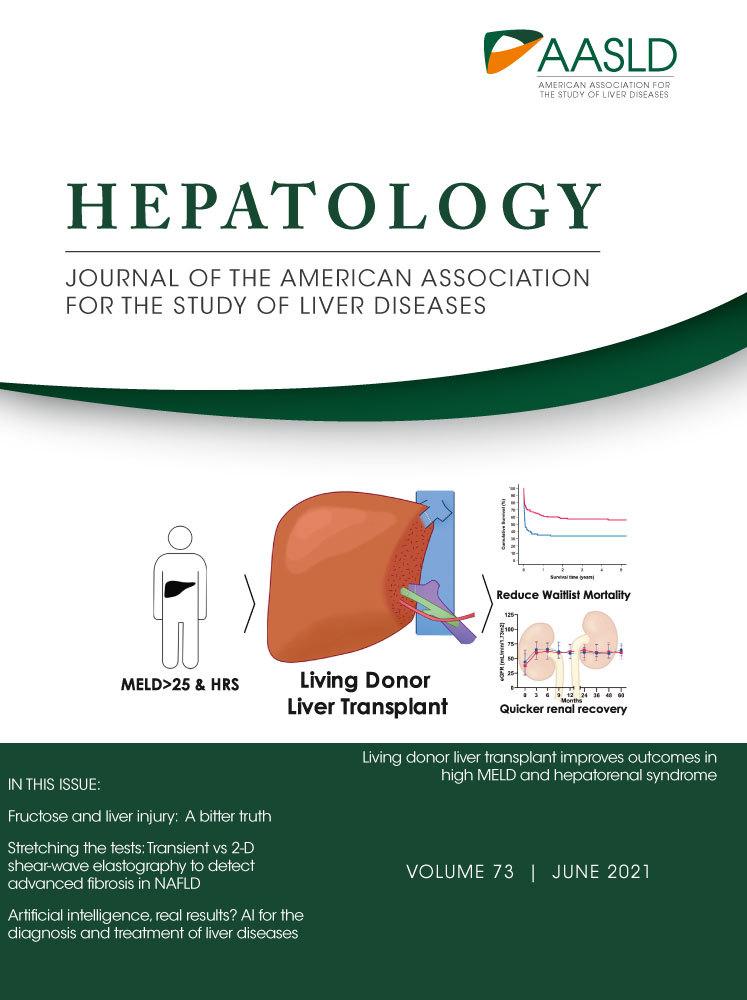
There were a greater number of patients with hepatorenal syndrome (HRS) in the deceased donor liver transplantation (DDLT) group than the living donor liver transplantation (LDLT) group.(1) Presence of HRS, even in a low Model for End-Stage Liver Disease (MELD) patient, increases the risk of waitlist mortality, which may be one of the reasons for higher waitlist mortality in the DDLT group.(2) Recently, Piano et al. showed that terlipressin responders have better 30-day survival, longer waiting list time, and lower MELD score at the time of liver transplantation.(3) We wonder if there were any differences in the number of patients with terlipressin response.
Secondly, the most common etiology of liver disease was hepatitis B. It would be interesting to know the bridging therapies used in both groups, which may have provided more window for liver transplantation. It would also be interesting to know the number of patients with alcoholic hepatitis, for which steroids are a potential therapy and nonresponders may have poor outcomes. Further, early liver transplantation is a feasible option for steroid nonresponders.(4)
Last but not least is the time to transplant. Time to transplant would be shorter in LDLT and is a major advantage of LDLT.(1) LDLT would improve outcomes due to easy availability of organ and reduce the waitlist mortality. With the current study showing no difference in perioperative or postoperative outcomes, LDLT would be a preferred choice for patients with a high MELD score. However, LDLT is not common. LDLT is more frequent in Asian countries, while DDLT is more frequent in others. With the increasing prevalence of liver disease worldwide and the shortage of organs, policies to educate about both LDLT and DDLT are required for better outcomes of patients with liver disease.
Author Contributions
A.V.K. and P.K. were responsible for the study concept and design; A.V.K., P.K., and M.S. were responsible for compilation and initial drafting; A.V.K., B.M., D.N.R., and P.N.R. were responsible for final editing and critical revision. All authors approved the final draft.